Top News

An interimVA OIG report on patient wait times at the Phoenix VA verifies the whistleblower’s claim that employees were hiding patient scheduling delays. They bypassed the electronic wait list application and instead sent screen shots of the appointment request directly to the outpatient treatment area, which was then responsible for entering them into the system but often ran weeks or months behind. The improved wait times allowed leaders to collect bonuses. OIG investigators added that inappropriate scheduling is a national problem, with schedulers gaming the electronic system in a variety of ways to show short appointment waits. They also noted that audit controls for the Phoenix VA’s VistA system were turned off. There’s no way VA Secretary Eric Shinseki keeps his job past the middle of next week given that he’s like Moses parting the Red Sea as politicians and bureaucrats of both parties put whatever distance they can between themselves and him as the lightning rod for public outrage.
Reader Comments

From The Product: “Re: Covisint. Lays off over 100, about 25 percent of the newly IPO’d company. Healthcare was rumored to have taken a huge hit, especially in analytics. The new CEO came in with the promise to streamline and cut he did.” Unverified. The new CEO said in the earnings call last week (revenue down 5 percent, EPS –$0.27 vs. –$0.10) that he is disappointed in the company’s performance and plans to cut costs and change leadership.
HIStalk Announcements and Requests
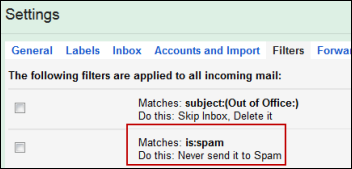
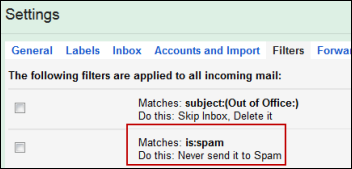
The latest in the long list of things I hate about Gmail is that its overactive spam filter can’t be customized or turned off. A reader said they sent me several emails that I finally found in Gmail’s spam folder (or label or whatever Gmail calls it) even though they bore no resemblance whatsoever to spam. I created the above filter since I would rather manually delete 50 spam messages than lose one important one.
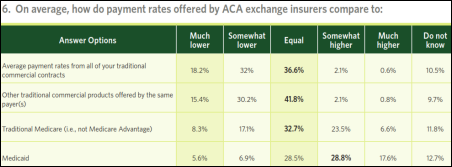
This week on HIStalk Practice: An MGMA physician survey finds that both physicians and patients are frustrated with the impact of ACA insurance exchanges. Atlantic City casino workers take healthcare matters into their own hands. Seema Rao, MD offers six tips on how to prepare for Meaningful Use. Healthcare actually fares worse than retail when it comes to security performance. Thanks for reading.
This week on HIStalk Connect: Dr. Travis covers Mary Meeker’s annual Internet Trends presentation, which touches on all things technology, and now includes a section on the convergence of technology and healthcare. The CEO of 23andMe discusses the future of personal genetics testing after the FDA shuts down sales of its healthcare-focused genetic testing product. Aver Informatics closes an $8.5 million Series A round to continue development on its "episode-based" financial analytics platform.
Listening: Swedish indie pop from Lykke Li. If you like (or Lykke) her, you’ll probably enjoy Bat for Lashes.
Acquisitions, Funding, Business, and Stock

Quality Systems (NextGen) reports Q4 results: revenue up 4 percent, EPS $0.12 vs. $0.24., missing earnings estimates. From the earnings call, the acquisition of Mirth integration engine was important as the company tries to repackage its EHR offerings into a clinical data repository that has population health management potential. Sales of inpatient core clinicals and financials aren’t doing so well, apparently. QSII shares dropped 4 percent on Thursday after the pre-market open announcement. Above is the one-year share price chart of QSII (blue) vs. the Nasdaq (red).
Sales
Kimball Health Services (NE) chooses the RazorInsights One clinical and financial system.

Miami Children’s Hospital (FL) will implement Xerox’s ICD-10 Complete.
In England, Viapath signs a seven-year, $18 million contract to implement the Cerner PathNet anatomic pathology system at Guy’s and St. Thomas’s Hospital.
Colorado Regional Health Information Organization selects Sandlot Solutions to extend its interoperability capabilities.
Allina Health (MN) chooses Omnicell for medication automation.
Intermountain Healthcare will use genomics-driven cancer care software from Synapse.
Upper Peninsula Health Plan (MI) will conduct a pilot to manage its Medicaid readmissions using infrastructure from Informatics Corporation of America .
People

Richard A. Caplin, CEO of The HCI Group, is selected as a finalist for EY Entrepreneur of the Year for Florida.

Orlando Portale has resigned as chief innovation officer of Palomar Health and will advise companies, investors, and provider organizations.


Nephrology EHR vendor Acumen Physician Solutions promotes Hugh Gaston to VP of operations and Jason Holcomb to VP of business development.

Remedy Informatics hires Scott C. Howard, MD, MSc (St. Jude Children’s Research Hospital) as chief medical officer.

Danny Sands, MD, MPH joins “digital checkup” vendor Conversa Health as chief medical officer.

The president and CEO of Athens Regional Medical Center (GA) stepped down last week over a problematic Cerner implementation and the ensuing physician revolt. SVP/CIO Gretchen Tegethoff has become the project’s second executive casualty as the hospital announced her resignation Thursday.
Announcements and Implementations
Arcadia Healthcare Solutions announces Launchpad, which allows users to create and monitor quality improvement programs and share them internally or with peer groups.

AMIA announces availability of its updated online Clinical Informatics Board Review Course to prepare physicians for the board subspecialty exam that includes new assessment questions and simulated exam questions. A 12-month subscription includes 23 hours of CME and costs AMIA members $1,495. AMIA reminds physicians that current practitioners need only take the exam to earn certification since they are grandfathered in until 2018, but starting then, a 24-month fellowship will be required.

The 2014 Health Privacy Summit will be held June 4-5 in Washington, DC, with National Coordinator Karen DeSalvo, MD as one of its keynote presenters.
Cerner makes 600 medical calculators available free as an MPage within PowerChart in a partnership with MedCalc3000.
PatientSafe Solutions makes Lead411’s list of “Hottest Southern California Companies.”
Government and Politics
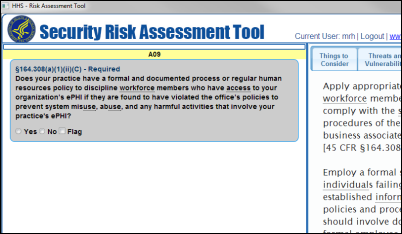
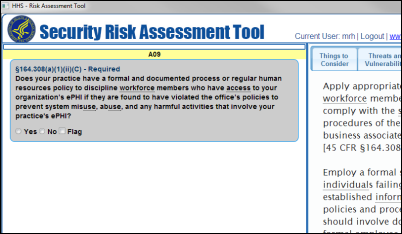
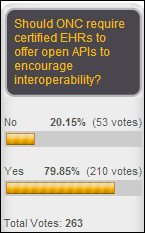
HIMSS says ONC’s Security Risk Assessment Tool is not intuitive, contains legalese that the average provider won’t understand, and references only one of several security frameworks (NIST’s.) I also noticed that ONC can’t figure out how set up a download that works for Windows 8.1 (not running the tool, just downloading it) and when I installed it under Windows 7, it gives a warning that there’s no digital certificate and shows its source as “unknown publisher” (consider the irony given that this is a security tool.) I agree that it’s full of needlessly complex wording, a reminder that just as you don’t let programmers design apps on their own, government wonks should bring in someone to put some end-user polish on their prototype. I’m still trying to figure out how to de-install it since it didn’t add itself to the start menu, the desktop, or Control Panel’s list of installed programs. I finally figured out that it just downloads to your default location (without asking or telling) and runs directly from there, which is primitive.
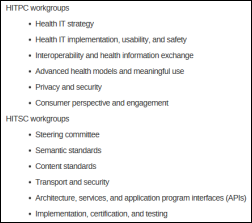
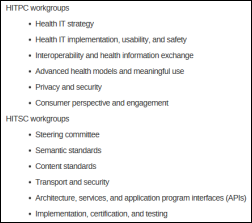
ONC seeks work group members for its Health IT Policy and Health IT Standards committees. Applications are due Friday, June 6.

Meanwhile in Florida, Governor Rick Scott says he’ll sue the VA for not allowing state inspectors to conduct unannounced visits to its Florida hospitals. The VA has repeatedly reminded Scott that states have no authority over the VA, but the grandstanding governor keeps sending inspection teams for the VA to turn away. Scott gained personal expertise with unannounced hospital inspections in his role as chairman and CEO of Columbia/HCA when the FBI and IRS raided several of its hospitals for Medicare fraud in 1997, which the company later admitted and paid $2 billion to make go away.
Here’s US CTO Todd Park’s pitch for Health Datapalooza, which kicks off this weekend in Washington, DC. I would be more interested in hearing him describe his holdings and participation in IPO flameout Castlight Health, but I’ll still be at Health Datapalooza. I also noted in reading Jonathan Bush’s new book that he lavishes extensive praise on Todd Park’s work ethic, brains, and nerdiness. I’ve interviewed hundreds of people and he’s still one of the nicest and most interesting of them.

Speaking of athenahealth, the company owned 8 percent of Castlight Health at its IPO, with athenahealth’s Jonathan Bush saying the profits led him to invest in more companies. “We bought an airplane and we made enough on that to buy a bunch of airplanes.”
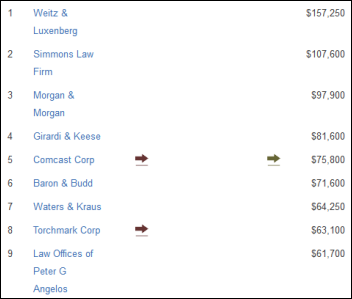
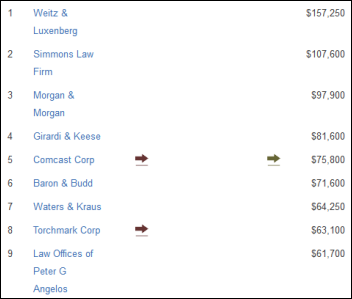
A TIME article says Congress killed the patent troll law because of pressure from Senator Harry Reid (D-NV), who has received $4 million in campaign contributions from lawyers and law firms (some of them listed above in his top contributors list). Patent troll lawsuits now make up 62 percent of all infringement suits, up from 29 percent just two years ago, with estimates of $29 billion in costs to defendants in the past three years. Companies will get no relief thanks to Senator Patrick Leahy (D-VT), who pulled the bill he had introduced while uttering an impressive array of unconvincing excuses that didn’t include being scared of Harry Reid.
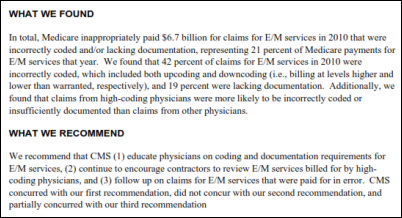
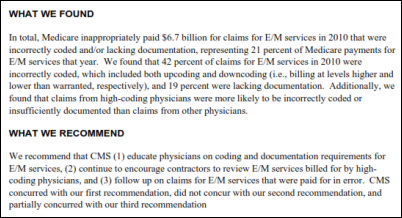
An HHS OIG investigation finds that Medicare paid $6.7 billion too much for office visits in 2010 based on the judgment of professional coders reviewing a small random sampling of claims, but the agency says it’s not cost-effective to for it to review the billing history of doctors who always charge for level 5, the most expensive visits.
Meanwhile, The Economist says thieves pillage the American healthcare system for $272 billion per year. It cites an example of a luxury apartment complex in South Florida that housed 500 residents who were collecting Medicaid checks. It says that ethnic mobs with weapons stockpiles have moved from cocaine trafficking to prescription drug fraud because it pays as well and the penalties are lighter. It also points out medical identify theft and the fact that CMS has yet to act on a GAO suggestion that it stop printing Social Security numbers on Medicare cards. One doctor made $12 million for writing narcotics prescriptions, with the required documentation (images or urine samples) conveniently available for purchase from entrepreneurs who set up shop at the clinic’s front door. It could get worse, the article says, as Medicare and Medicaid beneficiaries move to managed care that will provide the minimally effective government watchdogs with even less information with which to direct their unremarkable efforts.
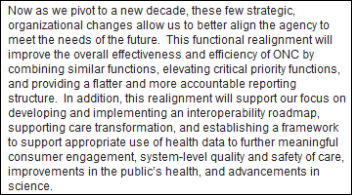
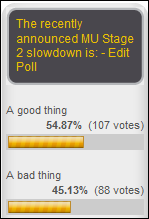
John Halamka offers thoughts on the Notice of Proposed Rulemaking that would change Meaningful Use attestation for this year. It’s really only a 90-day breather since the 2015 year still starts on October 1, 2014, so hospitals struggling with Transition of Care summary exchanges, electronic MARs, and portals don’t get much of a break. He suggests relaxing those requirements or changing the reporting period to any 90 day-period in 2015. Transition of Care is a noble idea, but community-based doctors can’t receive those summaries because they either don’t have a Direct address or there’s no way to look them up. He suggests allowing a hardship exemption where that’s the case. He adds that even CMS/ONC are confused because they keep individually tweaking the regulations such that, “It’s getting to the point that even the authors cannot answer questions about the regulations because there are too many layers.” He suggests simplifying the program for Stage 3, eliminating certification requirements and addressing only a few big-picture policy goals — he likes the idea of building Meaningful Use into the Merit-based Inventive Payment System that offers rewards but does not impose penalties.
Other
Samsung announces Simband, an experimental wristwatch whose sensors can measure blood pressure, ECG, oxygen, and heart rate. Samsung will make the device available to researchers to develop their own health-related wearable apps and devices, referring to it as a “design platform” rather than a product. The company also announced SAMI, an open software platform that collects data from wearable devices. Samsung also announces the $50 million Samsung Catalyst Fund to ramp up development of “disruptive sensors and algorithms” and a partnership with UCSF to validate them. All this comes just ahead of Apple’s expected wearables announcement at its developer conference next week.
Rumors say that Microsoft may be working on wearable sensors of its own, possibly incorporating Kinect sensors in a smart watch. The potential data partner is rumored to be Caradigm, of which Microsoft owns 50 percent in its joint venture with GE.
Over 400 medical school graduates failed to match for a residency this year, victims of a system in which medical school enrollments have increased while the number of available residency positions has remained unchanged for more than 15 years. Congress pays the cost of residencies and hasn’t changed the $10 billion in annual taxpayer dollars it has made available since 1997 to fund them, creating a bottleneck where larger medical school classes won’t change the total number of new doctors. The only positive development is that competition has pushed more graduates out of high-income specialties such as dermatology and orthopedics and into primary care.

Fitch Ratings keeps the bonds of MetroHealth (OH) at A-, with one of its positive observations being that the health system’s Epic system has helped it stay profitable despite a challenging payor mix.
CIO writes about an informal, information-sharing alliance of three CIOs of non-profits who “join forces to battle cancer.” The CIOs are from the American Cancer Society, the Leukemia and Lymphoma Society, and the fundraising arm of St. Jude Children’s Research Hospital. The most interesting part is the description of the increasing ability to match large data sets (clinical or genomic) to an individual patient’s condition to optimize treatments. Its quotes from other CIOs include this one from Pat Skarulis of Memorial Sloan Kettering: “Everyone on my staff knows someone who’s been affected. Some have fought cancer themselves. We’re not doing something for some remote benefit, something that might do some good in the future. We see on a day-to-day basis how what we do effects people’s lives. Every day that we don’t know something is a day we haven’t helped someone."
Sponsor Updates
- Ingenious Med’s Karen England discusses the ICD-10 delay.
- Concur App Center names Healthcare Data Solutions as its partner of the year for the second consecutive year.
- IHT2 offers a white paper on adding management to an LIS.
- Medical Records Associates acquires TrustHCS’s cancer registry services division.
- Awarepoint partners with Integrating the Healthcare Enterprise for interoperability demonstrations during AAMI 2014.
- DataMotion’s Bob Janacek details the difference of “push” and “pull” delivery methods for encrypted email.
- Arcadia Healthcare Solutions, CTG Health Solutions and Certify Data Systems discuss the challenges of creating and operating a successful ACO.
- PMD launches a HIPAA-compliant notification system with short, fun videos explaining the how and why.
- DrFirst, Forward Advantage, and Imprivata partner to provide e-prescribing of controlled substances for Meditech and MAGIC/OSAL platforms.
- Triangle Business Journal profiles PatientPay.
- HIStalk sponsors named on the HCI 100 for 2014 include 3M, ADP AdvancedMD, Alere Accountable Care Solutions, Allscripts, Beacon Partners, Capario, Capsule Tech, CompuGroup Medical, Craneware, CTG Health Solutions, Cumberland Consulting Group, eClinicalWorks, Elsevier, Emdeon, Encore Health Resources, ESD, Experian Health/Passport, Greenway, Harris Corp, Health Data Specialists, HealthStream, Iatric Systems, Impact Advisors, Imprivata, Infor, InterSystems, MModal, McKesson, MedAssets, Medhost, Merge, Navicure, Netsmart, Nordic Consulting, Optum, Orion Health, Perceptive Software, Premier Inc,, Quality Systems (NextGen), Siemens Healthcare, Sunquest Information Systems, Surgical Information Systems, T-System, TeleTracking Technologies, The Advisory Board Company, The SSI Group, Trizetto, Vocera, and Wolters Kluwer Health.
EPtalk by Dr. Jayne

I once read that part of being an effective writer is being a good reader. That’s pretty easy for me since I love to read. Sometimes I read for knowledge, sometimes I read for advice, and sometimes I just read for entertainment. Even in fiction my taste occasionally drifts to work-related content (Kate Scarpetta, anyone?) or high-tech thrillers (Dale Brown), although lately I’ve been choosing some fairly fluffy “beach read” type novels.
I’ve read a couple where the characters are in the film or TV industry. That’s about as far as it gets from my real life, so I suppose that’s good to allow my brain to recharge. Last week’s read included a plot line around a proposal for a TV show that was turned into a pilot and eventually a series. Assuming it was even halfway accurate, the process that a script goes through before it makes it to the home screen resembles either making sausage or creating CMS regulations, whichever you prefer.
There have been many notable medical TV characters. My personal favorites are the entire cast of “M*A*S*H,” “Quincy,” Beverly Crusher, and of course Dr. Quinn. I was too busy running a solo practice when “House” and “Grey’s Anatomy” initially came out, so I’m catching up on those via Netflix. My newest favorite, though, is BBC’s “Call the Midwife.”
I was in a 1950s public health mood (after finishing Season 2) when I read the HIStalk Monday Morning Update that referenced an article about physicians lacking physical diagnosis skills. I’ve had the privilege of working in extremely remote areas and I don’t disagree. I trained at a prominent medical school where technology was everywhere.
While on one rotation, I was asked what I thought about a murmur. My attending actually laughed at me when I said I thought we should get an echo for more information. Unlike the academic medical center where you could get a same-day echo, these patients had to travel several hours and generally wait a week or more to be scheduled.
During the first two years of medical school, the teaching of physical exam skills was cursory at best. We received a lecture about a given topic and were then turned loose to examine each other. It felt like preschoolers playing doctor. Unless someone has an unusual finding, there’s not much to learn from a crop of healthy 24-year-olds.
Even in third year when we examined real patients, we were generally by ourselves and without anyone more senior to make sure we understood the significance of what we were seeing, hearing, or feeling. Professional or “standardized” patients that coach students were just coming onto the scene.
The feeling that my medical education was somehow lacking (despite the steep tuition payments) became even clearer during a fourth-year rotation. I was at a community hospital that had a large number of residents who had trained at international medical schools. I quickly realized that most of them had not only studied in another country, they had been practicing physicians for years. They were repeating their training to try to get positions in the US.
My favorite resident was a neonatologist from the former Soviet Union. She could hear a tiny murmur from across the room and knew what it was before anyone else. Despite her busy schedule, she actually took the time to teach us, unlike many of the faculty who made it seem like teaching students was interfering with their research. Unfortunately, she couldn’t get a residency in her field and was therefore learning adult medicine after being in practice for nearly a decade.
There are a lot of pressures moving us away from physical diagnosis and towards tests. Patients often feel that high-tech evaluations are more accurate or just better than time honored skills. Others want data to convince them they’re OK rather than a person, who might be wrong. Defensive medicine, skyrocketing malpractice awards, and a fear of any kind of bad outcome (even if not preventable) cause unnecessary testing and added expense. Add that to the expectation that physicians complete an entire visit (including history, physical, documentation, and billing) in less than 10 minutes and corners are going to be cut.
In one of our offices, the exam rooms have speakers and a radio station constantly plays throughout the office to disguise the fact that there is no soundproofing in the walls. Without the radio, you can hear everything happening in the next room. Unfortunately, each room’s volume control is on the wrong side of the exam table, leading to decreased willingness for physicians to walk around, turn it down, use the stethoscope, and then turn it back up, especially during an increasingly compressed office visit.
The Washington Post article also mentions the fact that insurance pays for tests but doesn’t compensate us for spending extra time with the patient performing a more thorough history and physical. We are paid based on the amount of physical exam that is medically necessary based on the diagnosis – not what we do. I don’t get credit for performing diagnostic maneuvers if I end up determining that there is nothing wrong with you, because only a low level visit is justified.
Distraction is also an issue. I had a student shadowing me a few months ago. After seeing a particular patient for a rash, I asked what she thought about his tremor. She was so busy flipping through his chart that she missed a classic physical finding. I couldn’t blame the EHR for this one – the patient was a brand new patient and had brought his paper military file with him. The student was fixated on that, probably because it was a novelty.
Back to my initial thoughts about relaxing with a good book or learning about how TV shows are produced. A few years ago, there was a group of PBS series that took modern families and placed them in historical environments – “Frontier House,” “Colonial House,” and “The 1900 House” are the ones I remember watching. This was the educational aspect of the early reality shows.
If anyone knows anyone in the entertainment industry, I want to propose some sequels. Let’s do them all again, but with modern physicians in the cast. Let’s give them the tools of the trade appropriate to the time period and see how well they do with common period ailments.
Better yet, mix it up with graduates from top-tier research schools, primary care-oriented state schools, and schools in countries that lack abundant technology. In keeping with the spirit of today’s reality shows, let’s keep score. Any patient they misdiagnose or can’t help with the technology at hand gets added to their “kill chart” and lowers their rankings. And when they successfully figure out what to do with some of the odd-looking medical equipment from their time periods, they can earn points.
I think it would be entertaining, but I don’t think the outcomes would be surprising. I’ll bring my little black bag, my amputation knife, and my trephining drill. Who’s with me?
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis, Lorre.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.


























































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…