Top News

Six Wisconsin health systems that cover 90 percent of the state create a network to share resources, manage populations, and attract the business of employers, insurance companies, and individual insurance holders. All of the 44 hospitals owned by the unnamed network’s members use Epic and will share their Epic EHR information to manage populations and deliver care across facilities. The systems are Aspirus, Aurora, Bellin Health, Gundersen, ThedaCare, and UW Health. The board chair of the network says the members chose a virtual affiliation because working out the financial and administrative details of a merger would have taken too long.
Reader Comments
From Pink Slip: “Re: hospital IT department layoffs. Do you agree that the number seems to be increasing, or am I just noticing the announcements more?” That’s a good question to pose to readers, who are welcome to provide their thoughts. I asked the Advisory Panel about layoffs recently and few reported any, so I’m skewing toward it being perception more than reality.

From Frazzled CIO: “Re: Cerner. Our hospital announced the same day of the Cerner-Siemens announcement that we’re in discussions to acquire another hospital. We’re Cerner and they are Siemens. The announcement may have sent me over the edge if I hadn’t already been alerted through HIStalk of the potential deal and pondered the potential impacts ahead of time. Awesome work and thank you.” I will pass those thanks along to the readers who alerted me months before it happened and then provided thoughtful analysis Tuesday when it was announced. The “analysis” run by other sites was generally lame and dull, showing a remarkable lack of insight in gravely pontificating that Cerner should keep Millennium as its showcase platform (were they seriously thinking that Cerner would be tempted to lead with Soarian?) or that Cerner paid too much (they bought the Siemens IT business at the fire sale price of one year’s revenue, most of it probably recurring since Siemens isn’t selling much, and those customers can’t bolt short term.) The financial risk to Cerner is low as long as they don’t let the Siemens mess distract them.

The Siemens business needed to be bought because they had trashed it in the 10 years they owned it, as is often the case when a big company jumps into healthcare IT because it seems like easy money and because it makes their executives fell Silicon Valley-ish. I will repeat my mantra: only three companies (Epic, Cerner, and Meditech, although CPSI might logically be included) are serious competitors in the hospital core systems market and all three (a) built most or all of their products on a single platform; (b) sell and support one core system; (c) rarely acquire companies; and (d) haven’t themselves been acquired. Cerner breaks what would have been my fifth rule since they aren’t privately held, and now that they are buying the Siemens business, they will violate my third rule as well and we’ll see how that goes. Siemens was waiting to fall – events of similar importance that may happen one of these days that would put the industry into a similar frenzy are (a) Judy Faulkner retires and hands off Epic to her successors; (b) the retirement-age owners of Meditech decide to sell it given lagging market performance and the chance to cash out at the top; (c) Allscripts throws in the Sunrise towel because of infrequent sales, poor ambulatory integration, and a missed DoD contract if that happens; and (d) DoD’s selection makes Cerner, Epic, or Allscripts a household word but threatens to suck the energy out of them with endless government bureaucracy and implementation challenges.

From Brian Yeaman, MD: “Re: Cerner acquires Siemens. In my longstanding history with Cerner as a major client in interoperability and around HIE an population health for nearly a decade, we’ve seen Cerner commit and engage deeply around interoperability. We’ve had great success with Cerner native solutions as well as acquired solutions and their ability to support all platforms while integrating the best of both worlds regarding the front and and back end for HIE, Long Term Care, reporting, Direct and other EHR integration have empowered tremendous success in our efforts in Oklahoma. I’m very confident that this will be a big win for existing and new Cerner clients via Siemens alike. Cerner’s efforts to enhance interoperability and the entire care continuum and care regions like Coordinated Care Oklahoma just took a quantum leap, in my opinion, to the good.” Brian is chief administrative officer of Coordinated Care Oklahoma. I think it’s a good deal all around. Siemens was not that great of a vendor, hoarding its legacy system recurring revenue and pretending the world hadn’t changed since the swinging SMS 1980s. Its customers would have been faced with abandoning the company’s antiquated core systems at some point anyway since Siemens did little beyond half-heartedly dangling the unattractive Soarian bait in front of them with no bites. Cerner will force Siemens customers to finally make a long-term choice, hopefully soothing the pain of the ripped-off Band-Aid with attractive Millennium pricing and conversion assistance.

From Holly Mathews: “Re: Epic. Putting the health back in healthcare—that’s been a big initiative of mine at Epic for the past three years. It finally seems like preventative care is coming to the forefront of EMR attention or at least it’s slowly being pieced together. There is absolutely more emphasis on what folks are to doing to maintain a healthy lifestyle. To a new Epic customer today I responded, ‘Yes, we do integrate with Fitbit.’ There is a genuine desire to promote and manage not just the patients who are sick. I work at Epic as a project manager, but I also race bikes on a professional cycling team. Last week I won a stage at the Prairie State Cycling Series in Chicago. I thought it was pretty cool. 🙂 Epic will ultimately help drive the shift of medical practice paradigms to focus on and manage active lifestyle choices.” My favorite part of Epic is the youthful, idealistic enthusiasm of its mostly 20-something very smart employees with no pre-Epic healthcare experience who jump in with both feet, have fun, and work hard. My stock in trade is jaded, world-weary cynicism formed by many years of being ground down by clueless executives, dysfunctional vendors, and healthcare decisions made by everybody except patients and clinicians, so it’s fun to see new optimistic new blood who think they can change the world and who in fact just might, no matter who they work for.
From OGMD: “Re: Practice Fusion. Don’t even mention their name on HIStalk – cover them on HIStalk Practice. The only docs I know that use it are one-doc practices too cheap to purchase a best-of-breed EMR. They still use paper charts because Practice Fusion comes with no training and is not robust enough to go entirely paperless.”
From LFI Masuka: “Re: patient portals. The government mandates them, but patients will go online when it’s convenient or necessary. Kaiser’s success didn’t come from government mandate – they have things set up where it’s a bigger hassle to not use the portal than to use it. Most healthcare organizations don’t have such comprehensive control of the patient experience. My PCP is on Centricity, my specialist in the same clinic is on paper, and the local hospital is on an old version of Meditech. There’s a rudimentary RHIO trying to aggregate everything. As a patient, what compelling reason do I have to use a portal on any of these systems? I might trend some vitals or use it more if I had emergent health issues, but that won’t push the mandated numbers. We are throwing millions of dollars at technology in search of a problem.”
From Curious and Curiouser: “Re: patient portal opt-in. People are building the field to plug into the CCD format, but not actually placing the question anywhere it can be answered, essentially making every patient opt-in. What is your readers’ experience with opting in/out of portals? Are they asking the question or just opting everybody in to meet their numbers? It bothers me that the patients’ wishes aren’t being taken into consideration.”

From The PACS Designer: “Re: Apple. Reports suggest that the iPhone 6 could be announced on September 9.”
HIStalk Announcements and Requests
This week on HIStalk Practice: Dr. Andy rants about the review of systems and checklist solutions. Telemedicine’s future in small practices comes into question. Big-box retailers continue to encroach on the business of primary care. Patients go the Priceline route for non-emergency care. Over 100 medical groups call for delay of the Open Payments system. Physician and EP Stage 2 MU attestations continue to underwhelm. Mark Gettleman, MD leaves brick and mortar for mobile and online at Goofy Gettwell Pediatrics.
This week on HIStalk Connect: Dr. Travis discusses the overlooked direct primary care segment of digital health and why he’s excited to see what new technologies it spawns. The FDA publishes draft guidance reducing its regulatory oversight on a large segment of Class I and II medical devices. Doctors On Demand raises a $21 million Series A to expand its national telehealth platform. Researchers at the Medical College of Wisconsin link text message-based reminders with improved preoperative instruction adherence.
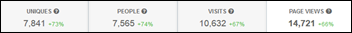
I almost never look at HIStalk readership stats, but May always starts the summer slowdown that runs through September. Surprisingly, the numbers jumped sharply up this past May despite mostly routine news and the rise has continued through June and July to record levels. Tuesday’s Cerner-Siemens announcement drove record single-day traffic with 10,600 visits from 7,800 unique people – I run HIStalk on a high-powered dedicated, rack-mounted server (geek alert: Xeon E3 four-core CPU, dual 7,200 RPM primary disks, 120GB SSD for MySQL databases, 16GB DDR3 memory, CentOS 64-bit Linux) and the page still took forever to load on Tuesday afternoon when the site was slammed. Visits in the past 30 days exceeded 150,000 and the number of unique people reading is 38,000, more than double the July 2013 total. I get an amazing amount of support from readers, sponsors, and contributors and I’m glad to see the numbers reflect that.
Listening: new from Mary Lambert, an eloquent and empowering 25-year-old Seattle singer-songwriter with a heartbreaking history of sexual abuse, body image problems, and bipolar disorder whose dark and emotional live performances often elicit tears from her audience. Lyrics: “Girls like us are hardly ever wanted, you know. We’re used up and we’re sad and drunk and perpetually waiting by the phone for someone to pick up and tell us that we did good. Well, you did good. I know I am because I said I am. My body is home.” If that’s not your thing, the new Godsmack rocks – my hand is tired but happy from desk-drumming.
Acquisitions, Funding, Business, and Stock

Allscripts announces Q2 results: revenue up 2 percent, adjusted EPS $0.09 vs. $0.05, meeting analyst expectations for both.
Practice Fusion acquires Ringadoc, which it calls a “telemedicine platform” and “next generation patient-doctor communication tools” vs. Ringadoc’s self-description as “medical answering service software.” The appeal to Practice Fusion — other than the fact that its CEO is an investor and mentor to the now-acquired company — is that Ringadoc is testing a doctor consultation service for consumers, although it seems to be phone-based rather than online.
The private equity firm that has owned healthcare product research vendor MD Buyline since 2011 sells the company to contract management solutions vendor TractManager.

Valence Health says its first-half revenues are up 51 percent year over year and it has added 10 clients so far in 2014. Headcount has risen 150 percent in three years to 470 and the company just leased 125,000 square feet of new office space in Chicago.
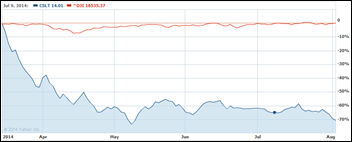
Walgreens announces that it will spend $15 billion to complete its acquisition of a European pharmacy and beauty company, but will surprisingly decline the resulting opportunity to declare its headquarters offshore to save a fortune in US taxes because of expected protracted IRS challenges and consumer backlash. The stock market’s reaction: shares dropped 14 percent. Meanwhile, the CIO of Walgreens hopes to leverage IT to meet the company’s goal of cutting operating expenses by $1 billion annually as it expects annual revenue to jump to $130 billion in the next two years.
Doctor on Demand, which offers $40 video visits, raises $21 million in a Series A round, with Sir Richard Branson as one of its investors. The company is recruiting doctors to staff its service, touting flexible shifts, $200K income for full-time work, no overhead, malpractice coverage, the ability to work from anywhere with Internet access, and easy-to-use paperless technology that is “more like applications they use personally than traditional medical software.” Sounds like the job-frustrated Dr. Jayne should work some shifts and report back.

Optum-owned QSSI, which was called in to save Healthcare.gov, will be the lead office tenant at a new Columbia, MD downtown office project scheduled for completion in July 2016.

CoverMyMeds will lease 64,000 square feet of office space in Columbus, OH to handle its expected growth from 70 to 180 employees in the next few years.

DrFirst secures $10 million in debt financing, which it will use to expand its development resources and prepare for international expansion.
People

Peter Csapo (VHA Inc. and McKesson before that) joins Accretive Health as SVP/CFO as the struggling company prepares to restate its financials.

CompuGroup Medical US promotes Werner Rodorff as CEO/SVP, replacing Norbert Fischl.
Announcements and Implementations
MModal joins athenahealth’s More Disruption Please program, adding its Fluency Direct and Fluency Flex mobile solutions to the MDP Marketplace.
Medicity and athenahealth will improve interoperability between their systems.

T-System donates T Sheets to QuestCare Clinic, a Dallas-area non-profit urgent care clinic. It is operated in partnership with Watermark Community Church and sees patients without requiring ID, insurance, or appointment, asking only for a $10 donation.
Children’s National Health System (DC) goes live on MedAptus’ dual-code ICD-10 solution for 600 physicians and 400 nurses.
Government and Politics
A VA hospital social worker and union president who claimed in May that her hospital was keeping secret patient waiting lists says the hospital harassed her after she met with a White House representative in July by taking her desktop PC away for a week to encrypt it.
A review of 2013 AHA hospital survey data finds that only six percent of hospitals met Meaningful Use Stage 2 criteria. The actual number is probably even lower because the authors looked only at EHR capabilities, not actual usage in tricky areas such as sending summaries of care and allowing patients to access their own information. The study also did not take into account where hospitals stood with regard to 2014 Edition criteria.
Other
A former Epic employee posts details of the company’s “cryptic raise/bonus black box,” explaining that the normalized results from ranking each employee against co-workers in the same role are sent to the compensation team that assigns raises. This person was hired right out of college at $60K and earned bonuses of $16K and year-end raises of 18 percent and 10 percent. The annual salary of the employee, who was probably 24 when he or she left Epic two years later, was $84K.
Can Sanjay Gupta, MD please get back to his medical practice and ask CNN to return to its regularly scheduled programming of cute cat videos and celebrity gossip?
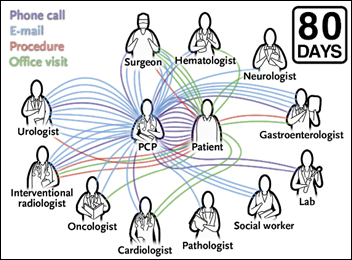
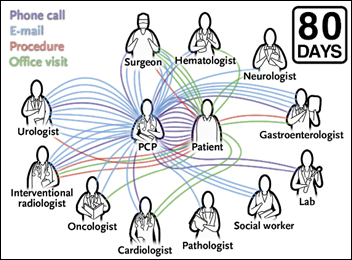
An internist writes in a NEJM article what it’s like coordinating the ambulatory care of a newly diagnosed cancer patient. In the 80 days from the time the internist told the patient about a liver mass until the day it was removed, the patient saw 11 other clinicians, had 11 office visits other than with the internist, and underwent five procedures. The internist communicated with those other clinicians via 32 emails and eight telephone calls, adding another 12 calls with the patient or the patient’s wife. He concludes that such coordination is essential for patient safety, but is difficult since it involves distributed teams of people who don’t know each other and the healthcare system was not designed to support collaboration. The internist was modest enough to not point out that neither he nor his employer (Weill Cornell Medical Center) were paid a penny for all of his efforts.

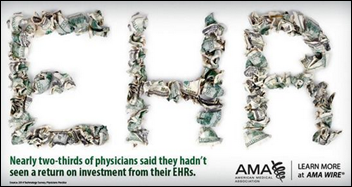
The annual Robert Wood Johnson Foundation report on EHRs finds that:
- Two-thirds of hospitals have received HITECH money, but few of them can meet Meaningful Use Stage 2 criteria.
- 59 percent of hospitals are using at least a basic EHR, quadruple the percentage of just four years ago, but only 26 percent have a comprehensive EHR and that number has increased only 3.6 percent since 2010.
- Of the physician practices that received a Medicare EHR incentive check in 2011, 12 percent didn’t get one in 2012.
- Of the physician practices earned a Medicaid EHR incentive payment in 2011, 61 percent did not in 2012.
- The only hospitals that fell on the wrong side of the “digital divide” are critical access and small rural hospitals.
- Health information exchange is still in its infancy, with barriers being privacy and security, competition concerns, and lack of physician demand.
- Most hospitals use their EHR to create organizational performance dashboards, but only about half use them to identify care gaps and allow doctors to query their data directly. The key barrier is lack of EHR dashboard and query functionality.
Weird News Andy speculates that patent trolls are getting bolder given this newly issued patent for this innovative process: (a) a patient calls a doctor’s office; (b) the receptionist records their information and asks the doctor if they want to talk to the patient; (c) if so, the receptionist calls the patient back, transfers the call to the doctor, and adds the recording of the call to the patient’s file. The article points out the infamous MMRGlobal/MyMedicalRecords, which sent threatening letters to practices who dared speak to their patients by telephone without paying it a license fee.
Sponsor Updates
- Aperek posts highlights of its attendance at the AHRMM conference.
- Blanchard Valley Health System extends its Wellcentive PHM initiative by instituting a Nurse Care Navigation program that nets significant ROI.
- Boston Software Systems publishes a white paper on avoiding five myths of EHR migration and eliminating the chaos.
- MEA|NEA uses the importance of a good website as an example of the importance of technology to growing a business in a recent blog post.
- PerfectServe posts an article titled “The Changing Role of the Physician.”
- Aprima kicks off its user conference in Dallas.
- ADP AdvancedMD spotlights three smaller private practices using its cloud solution to stay clinically and fiscally efficient.
- Kareo suggests six steps to take in hiring the right staff for a medical practice.
- NextGen Healthcare announces a new name for its November user group meeting, NextGen One.
- Premier Health (OH) discusses how it solved the challenges and complexities of payer pre-certification by deploying Passport Health’s OrderRite.
- SRSsoft will participate in the American Society for Surgery of the Hand conference September 18-20 in Boston.
- Allscripts shares what “Open” means for healthcare and why it’s so important.
- IHT2 offers an infographic, “Analytics: The Nervous System of IT-Enabled Healthcare.”
- Susan Niemeier questions whether the new cool thing is always the smart choice when it comes to technology on Capsule’s blog.
EPtalk by Dr. Jayne

Of course the big news around the IT corridors today was the announcement of Cerner’s purchase of the Siemens Healthcare IT business. We are using solutions from both parties in at least some fashion. I’m not going to say exactly which ones (or respond to a reader comment asking specifically what systems I use) because I’d like to keep my day job. Let’s just say we have multiple hospitals that we’ve acquired over time and thus have a variety of systems in play.
We’re consolidating, which made the announcement more interesting although it’s not clear at this point how the marriage will impact us. If we decide to chuck everything and move to a different vendor entirely (always possible, but I’m not sure we can scrape up that much cash) it might be a moot point. Unfortunately, so many of our users have grown accustomed leveraging multiple systems to get the work done that the idea of a single vendor isn’t as sexy as it once was.
There was exactly zero discussion of the merger in the physician lounge, which didn’t surprise me. Unless they have stock in a given vendor or were involved in a selection process, some of our providers are oblivious to what system they’re actually using. We’re one of those cutesy organizations that gives every system an acronym used in a branding campaign to assist with user buy-in. I once had a user tell an auditor that our vendor was “SMILE” because we had used that acronym for a go-live.
Coupled with the fact that some of our systems are from vendors that acquired other products that we already owned and morphed them into a suite of quasi-connected pieces under a single name, it’s a wonder we can keep track of everything that’s in place.
For those users who do care that we use multiple systems, one benefit of consolidating our vendors would be a more consistent user experience. We already do a fairly good job of interfacing the data from system to system so that users don’t have to duplicate data entry, but it would be nice to have a more uniform look and feel. I’ve been through several product demos as part of the consolidation effort and have to say that even among vendors purporting to be single system, the look and feel can vary dramatically depending on whether they purchased components or built the system from scratch.
In the same set of comments, Brian Too asked how physicians want technology to reconcile the “tactical” needs of point of care IT support with the “strategic” needs of population health and statistical capabilities. “How do you make the physician interactions with an EMR low-friction while still gathering enough information, of sufficient quality, to support the strategic imperatives?” The answer is a difficult one. The key is in finding an easy way to enter discrete data that physicians don’t perceive as “clicky” or overwhelming.
I’m personally holding out hope for voice-to-data in which narrative can be parsed to identify discrete elements. Physician notes could appear like the dictations they’re accustomed to, but the data could sit underneath, ready for the picking. Technologies are getting closer and closer, but we’re still not to the point where we can pull it off in the way physicians expect.
Even with the slickest user interface, most of our providers still perceive data entry as being something they shouldn’t have to do (even though they did it in the paper world, only with a pen). I think it’s a factor of the volume of data they have to enter now compared to the pre-MU, pre-ACO era.
He also asks: “How much of current physician griping is more about having lost a certain amount of workplace control versus serious mismatches between software capabilities and real workflow needs?” Particularly among ambulatory physicians (and especially among those whose practices have been acquired by a hospital or health system) loss of autonomy may be the majority of the problem. Many organizations do not do a great job with the change management piece of the EHR transition. I see them doing a similarly bad job in transitioning purchased practices from independent to employed models, especially when the organization desires to standardize workflows or centralize certain practice functions.
When we hire new physicians coming out of training, I don’t hear anywhere near the level of complaining that we do when we acquire practices. Most new physicians have used EHRs during training and they’re used to the limitations, so whether they’re using one system or another it doesn’t seem to be as much of a big deal. You’d think we get more complaining from our most tenured physicians, but we actually don’t. The most vocal and unhappy of our providers are in the 45- to 55-year-old range. They’re generally proficient users, but they also have the highest expectations for what the system should be able to do and don’t like it when it doesn’t deliver.
At this point my perspective is so warped, I’m not sure what an ideal EHR would look like. For more and more physicians, the ideal EHR looks like a scribe.
What is in your ideal EHR? Email me.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.













































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…