HIStalk Interviews Victoria Tiase, RN, Director of Informatics Strategy, NewYork-Presbyterian Hospital
Victoria Tiase RN, MSN is director of informatics strategy of NewYork-Presbyterian Hospital of New York, NY.

Tell me about yourself and the hospital.
I work as the director of informatics strategy at NewYork-Presbyterian Hospital. The position reports directly to our CIO, Aurelia Boyer.
My background is a nurse. I’ve been at the institution for almost 20 years. I did my graduate work in informatics at Columbia University.
My role in the IT department consists of consulting from an informatics point on various projects and initiatives throughout the department and organization. I also serve as the liaison to state and federal initiatives that pertain to health IT, which as you know over the past seven or eight years have really expanded. I work very closely with Greater New York Hospital Association and HANYS and other organizations as well as our internal government affairs department as it relates to health IT.
Is the hospital still using both Epic and Allscripts?
The hospital uses Allscripts. One of the physician organizations that is affiliated with the hospital uses Epic, but not the hospital.
Are you using other Allscripts products?
We use Allscripts SCM and Allscripts Pharmacy. In addition, we have a couple of their care coordination products, Allscripts Care Management and Allscripts Care Director. In addition, our ambulatory areas use the ambulatory SCM product. We also use their ED product in our emergency rooms.
You’ll be presenting on care coordination at the Digital Health Conference in November. What’s the role of technology?
I see it playing a huge role. It remains to be seen how the technology will be used in the care coordination arena. I think we’re basically sticking our toe in the water at this point.
Most specifically, what I’m going to be speaking about is our involvement in the New York Digital Health Accelerator program last year. It was a partnership between New York eHealth Collaborative and the Partnership Fund for New York City. They initiated a program last year where they find health IT startups that might already have some involvement in New York City and/or are interested in relocating and moving to New York City. They partner them with area hospitals for a mentoring perspective and the hospital has the ability to pilot that company’s technology if interested.
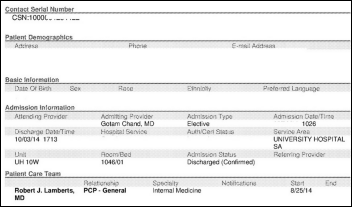
We participated last year and we just kicked off this year’s program, so we’re now in Year 2, but I’m mostly going to be speaking to our experience last year. We were paired with a company called ActualMeds. They have a loosely called medication reconciliation solution. However, the use that we found in speaking with the company and working and mentoring with them last year was that we have community health workers in a number of our programs up here in our Washington Heights area. They go into the home, they have a close relationship with the patients, and are helping us with that care coordination aspect in the community.
Prior to working with ActualMeds, we had the community health workers collecting information on paper while they’re in the home with the patients. They’re bringing that information back to our clinics and our program coordinators. It’s our way of gathering that information about the patient, which is so important for the continuity of their care once they leave our inpatient or outpatient clinics — what goes on at that point in time and how can we collect that information.
Using the ActualMeds technology, we had our community health workers for the first time using a tablet device to collect medication information from the patients in their homes. They are looking at the medications, talking with the patient, and entering the information in an electronic fashion. It is easier for our clinicians to look at that and then integrate that into the care of the patient when they are seen for their next visit.
It was a great learning experience for us because there’s this idea that health IT is going to help us do all of this care coordination. How do we break that down? How do we test and pilot and ensure that that will definitely make a difference? How do we do it in the best way possible?
We had a lot of learning experiences from just even understanding if our community health workers can use a tablet. There were so many things that we assumed and a number of assumptions that were proved wrong. It’s just some of the basic mechanisms of just operating a tablet. Then there’s understanding the operating system, understanding how to use a browser, understanding how to use an app. So many interesting findings came out of that work. I think it’s important for us to work with our players in the community and understand how technology can best meet those needs.
Are the startups you’re working with connecting to your Allscripts system?
They are not connecting. I assume you mean interfacing. No, they are not interfacing at this time. These are really just usability pilots. We’re continuing to work with ActualMeds. I think eventually down the road, we would love to have some use cases for patient-generated data in electronic medical records. We are certainly not there yet. That is a big topic in HIT.
Are you doing anything to allow patients to be more involved in the process?
We have a homegrown portal in which our patients have the ability to see the information on their visit. We have also just started some pilots on the inpatient side, where we are working with patients to see the medications that they are to be given and have been ordered for them on the inpatient side. We’re allowing them to document their pain level.
We are definitely doing some pilots in that area. We’re very interested in how that would work. Then as I mentioned, I think the trick is how you legally incorporate and safely incorporate patient-generated data into the electronic medical record.
I always wondered why hospitals don’t give patients their own version of the medication administration record so they can follow their therapies. What did you learn from the experience of patients seeing their medication schedules? Did they find opportunities to correct what otherwise would have been a mistake?
Absolutely. We’re finding a huge satisfaction from the patients in knowing what medications are being ordered for them and what medications they’ll be receiving. That’s where we’re finding the value.
It gives the patient the ability to ask questions, which I think is important. A lot of times, they don’t have the information in front of them, or they’ve been given the medication at a time that is not during rounds, so then they forget when the physician comes in for rounding or the team comes in for rounding. It’s like, oh my goodness, I wanted to ask you something about the medication — I forget what it was. Here they have it right in front of them. The satisfaction piece is the part that we were most pleased with.
Was that transparency threatening to nurses who might get called out for factors beyond their control for not being on schedule with meds or maybe even missing meds occasionally?
We did not find that. We did not receive pushback from our nurses. I don’t have results that we measured, but I think it takes the opposite effect. That makes me feel like, especially as a nurse, like, the patient knows what they’re going to be getting, when they’re going to be getting it. That way, they’re not going to be calling me every five seconds and saying, “Where’s my med, where’s my med, where’s my med?“
I think it actually would have the opposite effect. That is my hypothesis, but that isn’t something that we’ve measured per se. I’d be surprised if it was the other way around.
What are you doing with population health and analytics?
There’s certainly a lot in those areas. I guess our initiative that is farthest along is in our patient-centered medical home arena. Our ACN clinics have all achieved PCMH status level 3. We have a number of dashboards and tools that our providers use to see which are our diabetic patients — diabetes is one of our PCMH diseases — and how many of them have an A1C that’s of a particular level, when was their last visit, when was their last foot exam, eye exam. We certainly are doing a lot of work in that area — targeting our diabetic patients, our CHF patients, and also our asthmatics. Those are the big diseases we’ve been targeting.
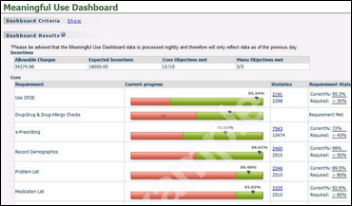
How is the hospital doing with Meaningful Use?
We are doing great with Meaningful Use. That’s one thing that I work on very closely. I’ve spent most of today working on that, in fact.
We’re in a great position with Meaningful Use and have certainly met it in the past few years. We are about to attest for Stage 2. Our learning there is that it certainly is a lot more time-consuming. It takes a lot of thought and it takes a lot of resources. It’s a project to not take lightly to make sure you’re doing it in a meaningful way and not just trying to check the boxes.
How about interoperability?
How about it? [laughs] Our nation is on a 10-year plan. Hopefully we’ll be seeing it soon. [laughs]
Meaningful Use, again, it’s just sticking the toe in the water. It’s a really small piece of what needs to be done. But I think we’re headed in the right direction.
I think for those that are attesting to Meaningful Use, you’ve now got some of the standards in place. A small amount, but you’ve got LOINC and SNOMED, so we’re starting to move in the right direction. I think there’s a lot more work to do. But it’s a place that we need to go. I think the CCD is a start. But as you’re seeing in the Times and other publications, we’ve got a ways to go.
What are the biggest issues and opportunities in nursing informatics?
Patient engagement is the biggest one in my mind. Nurses are in a unique position to be the discipline that leads efforts for patient and family engagement. There are some huge opportunities there. Nurses are already engaging the patients, already educating the patients. I think there’s great opportunities to use nursing and health IT to move that forward. That is one huge opportunity.
The second piece involves mobility and inefficiencies for nursing. We’re already seeing with medication barcoding and handhelds. Finding ways to use health IT and informatics and using the data as well in order to create more efficiencies for the nurses. We’re really looking at that.
We are very passionate at NewYork-Presbyterian about creating efficiencies for our nurses. Creating efficient workflows for them. We know they’re busy. We know there are a lot of tasks. How can we make their lives easier in caring for the patients in the best way possible?
That also includes providing real-time data to both the bedside nurses and the nurse managers. How can we get real-time data to them on their metrics on the number of patient falls and the other metrics that they might be tracking on their particular units? How can we get that data in their hands real time so it’s actionable?
Those are some of the big opportunities for nursing. There’s a lot of opportunity and a lot of work to do.
Do you have any concluding thoughts?
I know it’s an overused term these days, but I think engaging the patient in their care and partnering with the patient is going to be important moving forward. Engagement is not only on the patient side. The patients and family are in a place where they’re ready to participate. We also need to foster that engagement on the clinician side, getting the providers ready for that engagement.
There’s going to be a lot more information flowing from the patients in the near future. Being ready to provide that information to the clinicians in the small snippets or nuggets that will help them to take the best care of the patient is going to be an important area to focus on. I’m envisioning this influx of data from the patients and what are we going to do with it and how we’re going to make it meaningful for the providers to help the patients in the best way possible.



















































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…