News 10/31/14
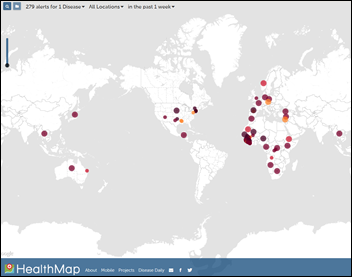
Booz Allen Hamilton acquires Boston-based Epidemico, stating its intention to delve deeper into population health analytics and following the recent trend of consulting companies getting into the software business. The company – a 2007 spinoff of Boston Children’s Hospital, Harvard Medical School, and MIT – analyzes large population health datasets to look for problems such as disease outbreaks, drug safety problems, and supply chain vulnerabilities. The company’s HealthMap shows disease outbreaks and alerts, which surely caught the Ebola interest of suitors. One of the founders, Clark Freifeld, is a PhD candidate and was a software developer at Boston Children’s, now apparently working for MIT Media Lab.
Reader Comments
From Capezio: “Re: CMS MU request website. Any idea why they took it down? We used it to get MU clarification until a week or two ago. A message says to use CMS’s main site instead, which has been improved but is infrequently updated and doesn’t cover emerging issues. Can you find out if this is a temporary hold or whether it’s gone for good?”

From The PACS Designer: “Re: end of Windows Server 2003 support. Just eight months away — migration planning should already be in the works.”
From Blue Hawaiian: “Re: service management best practice. Would love to see more. Healthcare seems slow to move in that direction, just as it was for quality management best practice (aka patient safety) for so many years.” It would be fun if a CIO with expertise on this topic would write something up about what they’re doing.

From See Sh*t: “Re: CCHIT. Funny that they’re leaving their minimal assets to the HIMSS Foundation.” My macro view is that HITECH money is losing impact and the hangers-on created to tap into it (certification bodies, HIEs, RECs, even ONC itself) are finding it tough to pay the bills as the taxpayer trough dries up. As I said in reacting to CCHIT’s bizarre January 2014 announcement that it would exit the certification business and turn into a thought-leader non-profit with unstated revenue streams, “The most recent Form 990 I could find was from 2011, at which time it was paying Chairman Karen Bell $409K, Executive Director Alisa Ray $250K, and five other employees over $100K. It would seem to me that given CCHIT’s genesis, mission, and name, it should just go away rather than trying to morph itself into the already overcrowded thought leadership business. It probably would if HIMSS wasn’t riding in on a white horse to save it, not surprising given that HIMSS formed CCHIT (along with partners AHIMA and NAHIT) in 2004.” Consulting firms and software vendors have already moved on from MU to the next government-incented shiny object: analytics and population health management, emboldened by the continued willingness of providers to focus their entire agenda on whatever Uncle Sam is writing checks for at the moment.
From Sponsor President: “Re: your site. You mentioned our company in a post that just went out a few minutes ago at 10 at night Eastern time. I’ve received 12 emails in the past 15 minutes. You are the best marketing value in all of HIT.” I appreciate that, although all I’m doing is putting out concise, factual information that I think is relevant and readers are free to use it however they like. Their response means the company has interesting offerings.

From Tipper: “Re: Epic. This week, Judy Faulkner said, ‘We do not like to participate with organizations that are going to sell the data because we’ve always felt the data is confidential. That’s another thing that has always bothered us about CommonWell.’ This seems to be CommonWell’s response.” A CommonWell blog post says the notion that it would sell data is “absurd” and “especially inaccurate,” adding that it will never sell personal health data and in fact as a broker doesn’t even have access to clinical data. The post adds that CommonWell will charge fees of 0.1 percent of each member’s annual revenue above and beyond membership dues.
HIStalk Announcements and Requests
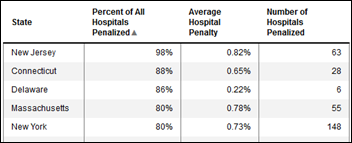
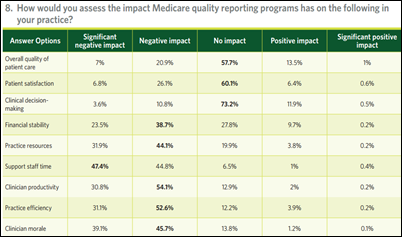
This week on HIStalk Practice: Day 1, 2, and 3 show updates from MGMA. Dr. Gregg takes healthcare IT to the land of Oz. MGMA members show no love for Medicare’s quality reporting programs. Spring Creek Family Medicine goes live on its eCW patient portal. HHS announces the four-year, $840 million “Transforming Clinical Practice Initiative” incentive grant program. Thanks for reading.
This week on HIStalk Connect: Dr. Travis covers Chicago’s newest digital health accelerator, Matter, and its first class of startups. Google unveils its newest X Labs project: a nanoparticle-filled smart pill programmed to enter the blood stream and search for early-stage cancer tumors. Fitbit releases two new activity trackers and a full blown smartwatch with a focus on health metrics. Salesforce is rumored to be optimizing its customer relationship management platform as an outreach and population health tool.
Welcome to new HIStalk Gold Sponsor Clockwise.MD, which is also sponsoring HIStalk Practice. The Atlanta-based company’s online reservation system lets patients skip the wait – they make an appointment (online or mobile), show up on time knowing their place is reserved, and then watch the wait times and queue order in real time on an iPad (I really like that idea – nothing is worse that fuming in a crowded waiting room wondering if you’ve been forgotten). Providers users gain interesting benefits: they can fill in their less-busy schedule times, keep patients informed about wait times via automatic text messages, and target delayed patients via a real-time dashboard so that appropriate customer service actions can be taken (like furtively slipping a slowly fuming Mr. H a current-issue Popular Science magazine that will otherwise age for months in the practice’s climate-controlled magazine cellar until it’s ripened enough for the waiting room coffee table). Here’s a fun idea: when a patient cancels their appointment, the open slot is broadcast by text message and whoever jumps on it first can take that appointment. The company’s founder and CEO is Mike Burke, who founded informed consent system Dialog Medical and sold it to Standard Register in 2011. Thanks to Clockwise.MD for supporting HIStalk and HIStalk Practice.
A quick YouTube search turned up this brand new Clockwise.MD explainer video.
My task following Dim-Sum’s amazing HIStalk webinar “DHMSM 101: The Hopes, Politics, and Players of the DoD’s $11 Billion EHR Project” (over 1,000 people have watched the YouTube recording) was to see if there’s interest in the sub-topic of military theater medicine, and if so, to enlist experts from Epic, Cerner, and Allscripts to join Dim-Sum in a follow-up webinar panel discussion. He doesn’t have a horse in the DoD’s EHR race, but is passionate about the topic as a military health advocate and veteran. Your thoughts are welcome.
Webinars
November 5 (Wednesday) 1:00 ET. Keeping it Clean: How Data Profiling Leads to Trusted Data. Sponsored by Encore, A Quintiles Company. Presenters: Lori Yackanicz, administrator of clinical informatics, Lehigh Valley Health Network; Randy L. Thomas, associate partner of performance analytics, Encore, A Quintiles Company; Joy Ales, MHA, BSN, RN, senior consultant, Encore, A Quintiles Company. Data dictionaries, organizational standards, and pick lists for data entry fields may describe the intent of a particular data field, but don’t guarantee that the data captured in the source system actually reflects that intent. Data profiling is the statistical analysis and assessment of the data values in source systems for consistency, uniqueness, and logic to ensure that the data landing in a data warehouse or analytic application is as expected. Attendees will learn which projects benefit from data profiling and the resources needed to accomplish it.
November 12 (Wednesday) 1:00 ET. Three Ways to Improve Care Transitions Using an HIE Encounter Notification Service. Sponsored by Audacious Inquiry. Presenters: Steven Kravet, MD, MBA, FACP, president, Johns Hopkins Community Physicians; Jennifer Bailey, senior director of quality and transformation, Johns Hopkins Community Physicians; Robert Horst, principal, Audacious Inquiry. Johns Hopkins Community Physicians reduced readmissions and improved quality by implementing a real-time, ADT-based encounter notification service (ENS) to keep the member’s healthcare team informed during transitions in care. Johns Hopkins presenters will describe the clinical, operational, and financial value of the ENS for care coordination along with its technology underpinnings.
Acquisitions, Funding, Business, and Stock

Lockheed Martin will acquire privately held government health IT provider Systems Made Simple for an undisclosed sum. The company does a lot of work for the VA and had $278 million of revenue in 2013.

From the McKesson earnings call:
- The company’s quarterly revenue was $45 billion.
- John Hammergren says he’s pleased with improved margins in Technology Solutions business, although revenue was down 6 percent in the quarter.
- Hammergren says CommonWell Health Alliance is demonstrating real-world interoperability progress in adding new members, and running four successful pilots.
- Hammergren said of the Technology Solutions business that “We’ve had the biggest challenge with in the EMR kind of space,” repeated that growth won’t return to previous levels until the transition from Horizon to Paragon is complete, and says that McKesson’s imaging business has been hurt as customers focused on buying products to meet Meaningful Use requirements.
In an apparent admission that CommonWell’s work will be commercialized as he hinted in the last earnings call, Hammergren said in the McKesson earnings call that CommonWell has signed “a multiyear agreement for nationwide commercialization of the services, with the core services being provided by RelayHealth.” I don’t know if CommonWell is the altruistic, non-profit, vendor-driven interoperability project it claims to be or a way for McKesson to sell RelayHealth services through Epic-scared EHR competitors anxious to launch a pay service for interoperability. The fact that it came up in McKesson’s earnings call suggests that the company is looking forward to new RelayHealth revenue.

BIP Capital sells its original fund’s stake in Ingenious Med to another private equity firm for a nine-fold gross return, but will continue to hold company equity in a second Fund.

Merge Healthcare posts Q3 results: revenue down 6 percent, adjusted EPS $0.05 vs. $0.02, beating expectations for both.

MedAssets turns in Q3 results: revenue up 5.6 percent, adjusted EPS $0.34 vs. $0.31.
IBM and Twitter, both desperately seeking new revenue sources, announce a partnership in which IBM will analyze tweet data for “business decision-making.” I don’t have access to big data that would support my theory that this project will go nowhere – tweets are such a uncategorized, free-text mess that surely no sane business would pay IBM to sell it Twitter-powered business advice.

MedStar Health (MD) expands its Cerner relationship with a seven-year agreement.
North Shore-LIJ Health System (NY) chooses Explorys for Hadoop-based analytics and risk models.

St. Luke’s University Health Network (PA) picks Nuvon for medical device integration.
People

Member engagement software vendor Healthx names Michael Gordon (iTriage) as chief product and strategy officer.

Voalte hires Suzanne Shifflet (ONR, Inc.) as CFO.

Randy K. Hawkins, MD (Glytec) joins Connance as chief medical officer.

Eric Johnson (Informatica) joins DocuSign as SVP/CIO.
Announcements and Implementations
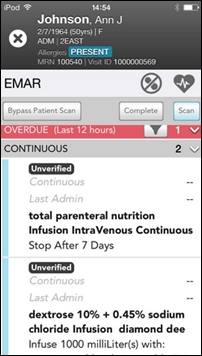
Allscripts introduces Sunrise Mobile Care, an iPhone/iPad app that lets nurses review and input patient information (allergies, vitals, I&O) with alerts and bi-directional updates from Sunrise. It’s curious that the vendor claiming to be the most “open” (whatever that means) supports only Apple devices.
Kaiser Permanente adds what it calls “medical selfie” capability to its patient portal, which allows patients to securely send digital pictures to their doctor for review. A copy also goes into their patient record. Patients can also send PDF files, such as scans of work-related forms that require the doctor’s signature.
RazorInsights will offer its laboratory information system customers instrument interfaces and workflow tools from Data Innovations.

In India, the renovated Sir HN Reliance Foundation Hospital will deploy Google Glass to its ED doctors, who will be able to review the patient’s history (including images) without looking away. SAP connected Glass to the hospital information system for two-way information exchange. According to SAP, “With the help of the Google Glass, doctors can attend to multiple patients, engage with them and see almost twice as many patients during the rounds. Doctors can take accurate notes on the Google Glass itself. The data is stored automatically and can be accessed when required.” Another hospital in India is creating a Glass-powered telemedicine application.
EClinicalWorks chooses Exostar’s ProviderPass SaaS-based identity proofing and second-factor credential authentication to meet the DEA’s e-prescribing requirements for controlled drugs. The company uses Experian-provided identity challenge questions or live webcam video.
In Canada, Nova Scotia’s Meditech hospital information system will go down next Tuesday and Wednesday for a software upgrade, with hospitals and clinics shutting down all non-emergency services, including surgeries, lab work, and diagnostic imaging.
Audacious Inquiry and Johns Hopkins Community Physicians sign a collaboration agreement to enhance the company’s encounter notification service.
Government and Politics

Former Massachusetts “Obamacare czar” Sarah Iselin, who in February was drafted to try to save the failed Massachusetts Health Connector health insurance exchange, quits to become executive-in-residence at Optum, which was awarded a no-bid contract to fix the exchange. She says there’s no conflict of interest since she hasn’t been involved in the project for the past six months, she was hired before Optum got the business, and technically she worked for the governor rather than Health Connector.
FCW covers the odd open source pitch of PricewaterhouseCoopers and General Dynamics in bidding on the $11 billion DoD EHR contract by offering up VistA, the very mention of which probably causes Pentagon brass to make mock retching sounds given that the VA developed it. They wouldn’t even interface to it, so the odds they’ll implement it surely are near zero, especially when they want a commercial system whose single vendor is committed to supporting and enhancing it. PwC and GD obviously were late to the taxpayer-funded party and found all the available EHR dance cards filled (those bidders that chose Meditech and Siemens later pulled out of the running). If the bid were being handicapped as a Presidential election, it would be Epic (Democrat), Cerner (Republican), Allscripts (Libertarian) and VistA (Green Party).
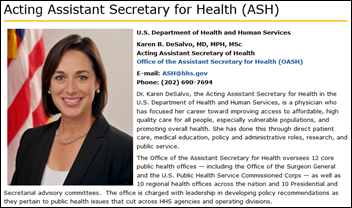
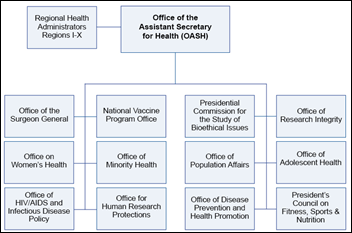
The AMA should probably just call up Sylvia Burwell instead of issuing a daily statement about ONC, but for what it’s worth (not much), AMA says it’s happy (or at least as happy as AMA can get) that Karen DeSalvo will still lead ONC in whatever fashion HHS decides is necessary to prevent pundits from predicting ONC’s impending irrelevance. It feels like HHS panicked at the ONC-negative response to her transfer and came up with a lame “she’ll do both jobs” excuse.
The House Science Committee on Science, Space, and Technology subpoenas former US CTO Todd Park to describe the security capabilities of Healthcare.gov.
The United States sues New York City and CSC for Medicaid billing fraud, claiming that the city used the default settings of CSC’s billing system to bypass Medicaid’s secondary payor requirement and used generic ICD-9 codes that they knew Medicaid would pay more quickly.
Technology

The 100-researcher team of Google X Life Sciences is developing a Tricorder-like early warning disease detection system in which patient-swallowed sensors send notice of tracked nanoparticles to a wristband. The project is being run by a renowned molecular biologist who used to work for LabCorp, in partnership with MIT, Stanford, and Duke. He says that healthcare is reactive and transactional, with diagnosis – especially for cancer – coming too late once symptoms are apparent (he calls this the “wait until you feel a big lump in your chest before you go to the doctor” approach). He also suggests that the big data possibilities could be enormous as therapies can be targeted to molecular profiles. This is tied into the company’s Baseline Study, in which it is attempting to quantify the measurements that signify good health. The technology is nearly ready for human testing, a flurry of new patents will come out in the next month, and the company expects widespread usage in 5-10 years. Google will license the technology as they did for their smart contact lens. Another Google group, Calico, is attempting to extend longevity, which he explains as, “We’re helping you live long enough so Calico can make you live longer.”
A Canada-based startup receives approval to sell its on-demand DNA testing device in that country, where frontline providers in any care setting (including pharmacies) can instantly determine whether a patient should receive the anticoagulant drug Plavix based on a known genetic problem that renders it less effective. More test types will follow. The company has earned FDA approval to sell its product in the US, but only to hospitals. The device costs $9,000 and each test is $225, but the company says it will tweak the price to make it affordable.
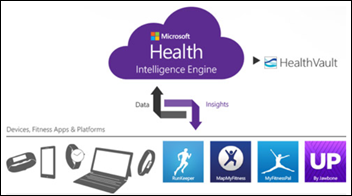
Microsoft announces Microsoft Health, a platform and app for collecting information from fitness wearables, planning to eventually add connectivity to share the information with providers via HealthVault. It claims its Intelligence Engine will provide insights such as fitness performance by time of day and after meals. In other words, it’s Microsoft’s answer to Apple’s Health and HealthKit with equally limited capabilities given that the information it can collect isn’t worth a whole lot except to quantified self fitness fanatics –your doctor doesn’t really have the time to monitor your step count or sleep patterns that have minimal immediate effect on the current problem list.

I’m not excited about Microsoft Health, but Microsoft also announces its $199 Microsoft Band, which is immediately available (kudos for not pre-announcing stuff that won’t be out for months – looking at you, Apple Watch). Kudos, too, that Band works with Android and iOS devices in addition to Windows-based mobiles and includes a GPS, heart rate monitor, and a two-day battery life vs. the imaginary Apple Watch’s one-day charge. It also uses a Bluetooth phone connection to display text messages, emails, and social media updates. It looks like a winner to me, with the only real competition being Apple (its fanboys are both loyal and patient) and Android Wear. I haven’t been tempted by any fitness tracker since my Fitbit Force was recalled, but Microsoft Band seems worth a look for those willing to pay for extra capabilities beyond the usual tarted-up pedometer.
Other
A piece in Madison’s hippie weekly (as I always call those left-leaning papers that feature mostly music reviews, sex-related ads, and pathetically predictable anti-establishment rants) covers Epic without saying anything new or insightful except one thing: the company confirms that it has built a data center in Verona for client hosting. That’s a pretty big deal: Cerner has gained many small or remotely located customers (and made a lot of money) from its remote hosting services, while Epic, like Meditech that inspired it early on, has stubbornly avoided the obviously smart move of making its systems available as a service to let hospitals avoid the capital costs and personnel requirements of running it from their own data centers. That policy made sense when Epic sold only to academic medical centers with big IT budgets and big IT egos, but now that it’s moving down-market, hosted systems are likely to be a hit. I’ll follow up for more information.
The iMDsoft Metavision software bug that was characterized in a risk assessment as being potentially lethal to ICU patients in Australia turns into a political issue. Opposing political parties in Queensland debate the extent to which patients have been warned and invoke unpleasant memories of Queensland Health’s 2010 payroll system implementation, in which IBM turned a $5 million fixed-price bid into a billion-dollar project with a little help from company-friendly bureaucrats (which got the company banned from future Queensland work). It’s one of three health-related examples that come to mind when enumerating the biggest IT debacles in government IT history, along with England’s NPfIT and Healthcare.gov. Meanwhile, iMDsoft says Queensland Health is testing a fix it provided, explaining somewhat mysteriously that the problem came up during testing, perhaps tactfully declining to throw its client under the bus for their role in going live with a known problem.
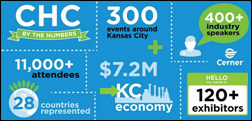
Cerner expects 11,000 participants from 26 countries at its annual conference in Kansas City, MO next week, with attendance up 20 percent over last year.
Columbiana Family Care Center (OH) closes temporarily after the computer system of its owner, Salem Regional Medical Center, goes down after an unspecified software problem.
The Chinese engineer charged with stealing proprietary MRI programming information from his former employer GE Healthcare and sending it back to China will plead guilty to stealing trade secrets, facing 10 years in prison, a $250,000 fine, and deportation.
It’s not completely health IT related, but Genentech angers hospitals by changing the way it distributes three cancer drugs – Avastin, Herceptin, and Rituxan – to six regional distribution centers rather than the usual drug wholesaler, citing the need to increase drug supply chain security. Hospitals say they won’t be able to get those meds daily as they always have so they’ll have to stockpile the expensive drugs, they’ll have to rely on overnight shipping companies in emergencies, they will lose traditional discounts, and on the data side won’t get wholesaler-provided benchmarking information and convenient 340B accounting. Similar events have happened on the consumer side, where drug companies declare an expensive item a specialty drug, meaning patients have to get their supply from mail-order pharmacies that focus on expensive drugs for chronic conditions.
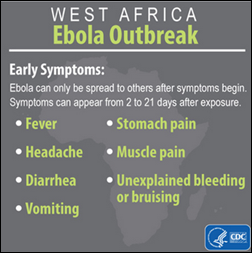
Louisiana state health officials tell doctors planning to attend a New Orleans tropical medicine conference this weekend to stay home if they have visited Liberia, Guinea, or Sierra Leone within the past 21 days. The conference, ironically, was to feature presenters talking about their work in fighting Ebola in Africa, but now those experts won’t be allowed to attend. The letter admits that even infected people don’t spread the disease if they aren’t showing symptoms, but adds that, “We see no utility in you traveling to New Orleans to simply be confined to your room.” Science and politics just don’t mix.
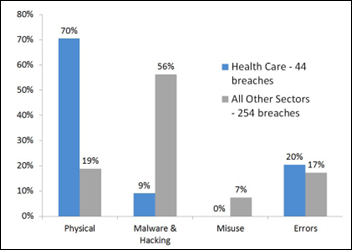
California’s attorney general issues her 2014 data breach report, which finds that the number of records exposed in healthcare breaches was higher than in all other sectors except retail. The AG points out nicely that healthcare is an outlier because most of its breaches involved stolen hardware that wouldn’t have been a breach at all had their owners simply encrypted the devices. Here is my advice to healthcare CIOs: if you aren’t encrypting all laptops because you haven’t asked for the money, you should be fired. If you aren’t encrypting all laptops because administration won’t give you the money, you should quit. Either way your name is going to be up in quite embarrassing lights when someone loses a laptop (probably after violating a hospital policy in taking it home after storing PHI on the local drive) and your boss has to sheepishly admit to the local community that it wasn’t encrypted. On the bright side, that one exposure usually results in the board coming up with encryption project money, albeit after the fact.
Sponsor Updates
- Forward Health Group will participate in the IHI National Forum on Quality Improvement in Healthcare December 7-10 in Orlando.
- Clinovations shares Dennis Glidewell’s thoughts on areas of opportunity in the revenue cycle in Ask the Expert.
- IHT2 announces the speakers and topics for Health IT Summit Houston December 10-11.
- EClinicalWorks signs an additional 37 CHCs and FQHCs.
- Washington Business Journal names GetWellNetwork to its “50 Fastest Growing Companies of 2014.”
- CareTech Solutions will discuss hospital website security threats at the 18th Annual Greystone.Net Healthcare Internet Conference November 3-5 in Scottsdale, AZ.
EPtalk by Dr. Jayne
Cleveland Clinic announces its list of top medical innovations of 2015. Since the list was compiled by people in the patient care trenches, it’s not surprising that it was heavy on drug and treatment technologies and light on health IT.
We hear a lot about alarm fatigue, so I was interested to see this article on “decision fatigue” as showing that physicians prescribe more antibiotics later in their workdays, even when the drugs may not be appropriate. It’s a research letter that doesn’t have the same weight as some other studies, but it is interesting nevertheless. I know I get tired at the end of a full day of seeing patients and definitely don’t feel as sharp as when I start. I’d be interested to see an analysis of allergy and interaction alerts stratified by time of day and how our physicians reacted to them.

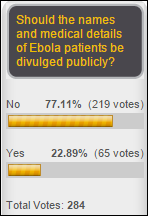
I had the privilege of moderating a hospital community forum last Saturday morning. I posted some of the questions/comments in Twitter, but I can’t say I’m a fan of live tweeting. I was impressed by the level of patient engagement (and the knowledge) around Ebola. To be fair, there were plenty of questions about other key community health priorities, including diabetes and a couple of questions about childhood vaccinations.
Discussing a disease for which there is no vaccine in the same session as diseases for which there are vaccines that people refuse was a bit surreal. A couple of the attendees mentioned the polio scares of the 1950s and hearing the perspective of people who watched their schoolmates become ill and disabled was moving. I found this NPR piece the other day that talked about the polio vaccine trials and why they could never be done today. If nothing else, we live in interesting times.
I finally registered for HIMSS this week. I waited too long last year and am happy to report that there are still plenty of good hotels left. Although I’m not crazy about Chicago as a site for conferences, it’s a fun town. I’m already scheming with a good friend for some potential pre-conference fun and am keeping my eye out for just the right HIStalkapalooza shoes (although this charming Louboutin handbag is a little out of my price range).
In the Breach of the Week, hundreds of medical records were lost when they blew out of the back of a truck in Omaha, NE. Apparently the medical waste disposal company didn’t secure them properly. I was impressed by volunteers that were helping pick them up, even reaching into a storm sewer to gather documents. The news report indicates they were on their way to be “stored” in Lincoln, NE which makes the fact that a waste disposal company was transporting them a bit curious.

I’m off to CME this weekend and have blown my conference budget for the year. I wish I had saved up some cash to attend the mHealthSummit in December and particularly the Gala Reception for Disruptive Women in Healthcare. If nothing else, it would be a great opportunity to pick up swag and take pictures for my desk that would drive my boss crazy. Maybe someday I’ll make the list of Disruptive Women to Watch.
Who are your favorite disruptive women? Email me.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.













































 2
2











I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…