Top News
HL7 launches the Argonaut Project to address the standards recommendations of the federal government’s JASON group, including HL7’s FHIR (fast healthcare interoperability resources). Working with HL7 will be athenahealth, Beth Israel Deaconess Medical Center, Cerner, Epic, Intermountain, Mayo, Meditech, McKesson, Partners HealthCare, SMART from Boston Children’s, and The Advisory Board Company. HL7 says the group will create FHIR-based EHR data sharing API specification by the spring of 2015. The big news here: (a) the second JASON report called for a big vendor to propose an open API standard instead of waiting around for the government to do it; (b) FHIR and APIs are a heck of a lot better than today’s document-based interoperability standards and probably better than the customized jungle that the HL7 standard has become; and (c) getting Epic, Cerner, Meditech, and McKesson together at the same table covers nearly all of the hospital EHR market and Epic, particularly, is a key member given its non-participation in CommonWell (and Epic and Cerner already have customers using APIs).
I asked an expert who shall remain unnamed to summarize Project Argonaut:
Project Argonaut is beginning the hard work of not only formalizing the API calling sequence (the easy part and something most vendors already do), but to formalize a set of vocabulary objects – Problems, Allergies, Notes, etc. with controlled vocabularies and predictability. To make FHIR really work, both must be done well. If FHIR succeeds, it will allow third parties to create an “app” and be able to run it in any FHIR-compatible system without the meet and map exercise with each implementation. What we’ll need to do with FHIR is to ensure people don’t get ahead of themselves and customize the “resources,” otherwise we’ll be back in the same boat as HL7 v2. FHIR is at the peak of inflated expectations. It will be great as a minor plug-in where there’s a UI or visualization, but not so great for machine-to-machine communication where one of the endpoints might not always be reliable for high-volume transfers at scale – some of the simpler web service configurations can be horribly inefficient, like making separate grocery store trips for each item on your list. There may be audit and security issues as well.
I asked another expert how the Argonaut Project might relate to CommonWell:
There is no immediate connection, but over time, CommonWell could add services that are based on the FHIR standard that the Argonauts are trying to speed up. For example, CommonWell today uses XCA to move CDA documents around, but that can be cumbersome if all the doctor wants is to get a list of known allergies from some other site. FHIR makes the later query much easier than using XCA to move a "fake" document that contains only allergies. So, CommonWell will benefit from the success of the Argonaut work (assuming it’s successful!) But otherwise, there is no direct connection, though some of the same people are involved with both.
Reader Comments

From Ken L. Ration: “Re: HIMSS. Our designer got a good laugh from this HIMSS15 promotional graphic. One thought it was an attempt to be edgy, but the general consensus is that it’s a marketing fail.” I think it’s an insightful graphic: those benzene ring-shaped items are probably snowflakes burying HIMSS attendees who would much rather be almost anywhere else — Chicago came in seventh of 11 desired HIMSS cities last time I surveyed, with the clear winners being San Diego, Las Vegas, and Orlando.
From Roy G. Biv: “Re: physician billing services. Do health systems keep using them after implementing Epic? Could you ask your readers if, for instance, the keep using athenahealth’s PM and billing service post-Epic?” Readers have been duly notified – responses are welcome.
From HIT5982: “Re: Medhost. Let 71 people go Wednesday all at once. HR cleaned out their desks while they were being told. I was one of them – I worked in the department division (EDIS, Patient Flow, perioperative) and was told the emphasis will shift to Enterprise (clinicals, financials, patient access, revenue cycle). Departmental sales were down this year.” Reported by two readers. I reached out to the company for a response but didn’t receive one. Nothing says Christmas like being laid off.

I shall digress and pontificate on the topic of layoffs. I’ve seen both sides over the years: (a) I was literally on my way out the door before getting a last-minute reprieve in my one and only vendor job many years ago, where layoffs every quarter were a given as executive bonuses became threatened by poor financial numbers mostly due to their own poor decisions; and (b) I have personally marched at least 20 people out of the hospital IT department through a gauntlet of their peers as I served as judge, jury, and executioner for high-level decisions that I neither made nor agreed with. Both situations were largely created by clueless, spreadsheet-circulating executives who were shockingly indifferent to the havoc they were wreaking on the lives of people and their families. While some of the folks who get axed deserved it and should have been canned a lot sooner, many of them had been given perfectly fine performance evaluations but were singled out for factors beyond their control: changing organizational strategy, their own demographics, higher salaries that they had been voluntarily offered to them, and doing their jobs every day instead of kissing executive butt and backstabbing their co-workers. Readers regularly send me personal stories about being cut loose and I always provide the same response: you’ll be better off in the long term because who wants to work for a company that lays people off? To people all over the industry who have to face the holidays (and their families) with uncertainty, fear, and feelings of personal inadequacy for whatever reason, I am truly sorry. It will get better.
From Pierre Dukane: “Re: slimy companies. This site [URL omitted] charges consultants $300 per quarter to be on the ‘elite’ list for go-live job notifications, using information it gathers from other members and online job postings (duh). The ‘About’ page doesn’t say who runs it and the domain registration information is blocked. I can’t believe people pay for this garbage. Also, an HIT consulting firm’s recruiter is sending emails offering entry into a gift certification drawing if they ‘forward any email you receive from another recruiter or company regarding current opportunities or referral incentives.’ What happened to working the old-fashioned, honest way? No wonder clients and consultants feel so negatively about consulting firms.” It wasn’t hard for me to track down the operator of site you mentioned, which doesn’t seem to be offering much for $1,200 per year. But hey, it’s a free country, and he’ll either get business or he won’t depending on the value he provides. I’ve had both good and bad experiences with recruiters that I’ve either hired or been placed by, but I agree that quite a few questionably motivated people see it as nothing more than making easy money by matching Resume A to Job Posting B. Nearly everything in life can be explained by supply vs. demand.
From Elsa: “Re: BJC’s core clinicals replacement. Vendors were to have been notified Friday. I was shocked that it wasn’t Cerner – my source says it’s Epic. Not sure how they’ll justify the cost when they laid off staff, cut charity care, and froze raises.” Unverified.
From Not Quite: “Re: JASON report. ONC is putting a lot of stock in it, but it’s a fake that is partially plagiarized from Wikipedia. The report lists many references, but fails to list Wikipedia, from which many things were copied. ONC should ask for our money back!” No report should ever reference Wikipedia since it’s not a vetted reference, but hopefully the JASON folks cited their primary references properly, at least where a source contained something that isn’t common knowledge.
HIStalk Announcements and Requests
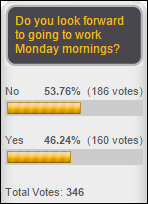
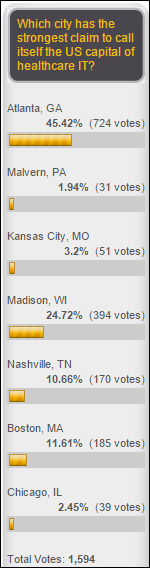
Voting for the US capital of healthcare IT has been heavy, with Madison leading the pack and Nashville and Boston pulling up as a distant second and third. Voting ends this weekend – my poll is here.
This week on HIStalk Connect: Data scientists with athenahealth are monitoring the onset of the 2014-2015 flu season and note an early uptick in flu-related visits. Google is said to be revamping the internal components of Google Glass in an effort to boost battery life. Personal genome testing startup 23andMe will begin selling genetic tests in Canada and the UK after a year of trying and failing to secure FDA approval for US sales.
This week on HIStalk Practice: Payers in Colorado build online claims data-sharing tool for physicians. HIPAA compliance at physician practices is found to be woefully lacking. Gila River Health Care goes with NextGen, while Advocate Community Partners selects eClinicalWorks. Practice Fusion VP argues for net neutrality, while Amazon takes advantage of lightning-fast consumer Internet connections. AMA winner Nancy Adams asks, “Interoperability? How about achieving operability first?” Thanks for reading.
Webinars
December 17 (Wednesday) 1:00 ET. There Is A 90% Probability That Your Son Is Pregnant: Predicting the Future of Predictive Analytics in Healthcare. Sponsored by Health Catalyst. Presenter: Dale Sanders, SVP of strategy, Health Catalyst. Predictive analytics is more than simple risk stratification. Once you identify an individual’s risk, what are the odds that you can change their behavior and what will it cost to do so? This presentation, geared towards managers and executives, addresses scenarios in which predictive models may or not be effective given that 80 percent of outcomes are driven by socioeconomic factors rather than healthcare delivery.
Acquisitions, Funding, Business, and Stock

Integrated payments network vendor InstaMed raises $17 million in a private placement, $2 million more than it was seeking.
Sales

Rio Grande Valley Health Alliance (TX) and Lakewood Health System (MN) choose Lightbeam Health Solutions for population health management. I interviewed CEO Pat Cline a few months ago.

Western New York’s HEALTHeLINK HIE chooses Stella Technology’s clinical data access technology for analytics and reporting.
Children’s Hospitals and Clinics of Minnesota chooses Strata Decision’s StrataJazz for decision support and cost accounting.

Granite Health Network (NH) selects athenahealth’s athenaCoordinator Enterprise Population Manager.

The Medical Center at Bowling Green (KY) chooses ProVation Medical for its cardiac cath lab.
People
CompuGroup Medical US promotes Navid Asgari to VP of service and support for its ambulatory information services division.
Announcements and Implementations

Lehigh Valley Health Network (PA) announces that its physician group will move to Epic.
Levi, Ray & Shoup announces release of a new user interface for Epic users of its VPSX output management solution.
Imprivata announces OneSign 5.0, a new version of its authentication and access management product.

Children’s National Health System (DC) opens an Innovation and Learning Center to house Bear Institute, its partnership with Cerner. The announcement is confusing, but I think it’s just a new physical space to house the existing project, which was announced just over a year ago.
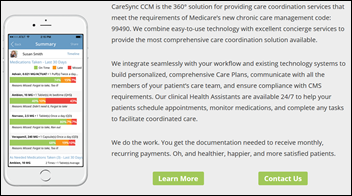
CareSync launches its Chronic Care Management service that allows providers to earn Medicare’s monthly CCM payments.
Perceptive Software launches Perceptive Interact for Google Apps, which allows users to integrate Gmail content into Perceptive Content for review, routing, and collaboration.
Government and Politics

ONC names Jon White, MD from AHRQ as acting deputy national coordinator and acting chief medical officer, taking over for the recently departed Jacob Reider, MD.

Someone tweeted out this fascinating article from March called “Sinkhole of Bureacuracy,” which describes the 600 federal government employees who push paper in the abandoned limestone mine run by Iron Mountain in the middle of nowhere in Pennsylvania at a cost of $56 million per year. Previous federal government automation efforts of the government’s retirement program failed despite spending well over $100 million. A former employee described the manual process as, “I used to chase people for months — literally — for one signature on one piece of paper. You want to talk about an egregious waste of taxpayer money? … On a daily basis, we would get from five to 50 e-mails, asking everybody to take time out of their day to search their desks for case files.” The article says the old mine is legend in the federal government, quoting former CTO Aneesh Chopra as calling it “that crazy cave.”
Massachusetts says it has repaid most of the $2.1 million in Medicaid EHR incentives that were incorrectly given to 19 hospitals that were identified by the HHS OIG. The state blamed requirements that are hard to understand and hospitals that reported incorrect data to the federal government.
Innovation and Research
A small study finds that a computerized symptom questionnaire that was turned into a History of Present Illness narrative using computer algorithms created a better HPI than physicians doing it themselves.
Other
Hospitalists at two Oregon hospitals form a union, hoping to remain as hospital employees rather than being outsourced to a national firm.
A review of a tiny sample of the 100TB (!!) of data hackers took from Sony finds medical information, in the form of doctor letters for medical leaves of absence. The responsible hacker group, possibly from North Korea, has posted some of the information publicly, including salaries, scripts, and video files of unreleased Sony movies. The hackers also released a Word document titled “Passwords” that some idiot Sony executive had used to store all of his computer passwords and credit card information. Sony was burned by hackers in 2011 who stole credit card numbers and took down its PlayStation network for weeks.

New York police arrest radiologist James Kessler, MD, MPH for copying the information of 97,000 patients of his former employer onto a portable hard drive with intention of starting a competing business.
Singer and cancer survivor Melissa Etheridge, just announced as a keynote speaker for GE Healthcare’s Centricity Live user conference, creates a line of prescription-only “cannabis-infused fine wines” that provide “a delicious full body buzz.”
Sponsor Updates
- An Imprivata video provides an overview of electronic prescribing of controlled substances.
- HCS provided 50 tickets to the Los Angeles screening of the overwhelmingly positively reviewed Glen Campbell documentary “I’ll Be Me” in support of Alzheimer’s awareness. The company will be contributing to the Salvation Army through the holidays on behalf of its clients.
- DataMotion earns accreditation as a Certification Authority and Registration Authority from DirectTrust.org and EHNAC, allowing it to issue and manage digital certificates in addition to its role as an accredited Health Information Service Provider.
EPtalk by Dr. Jayne

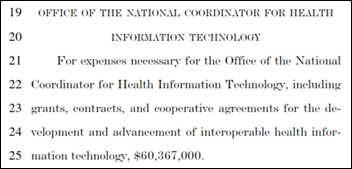
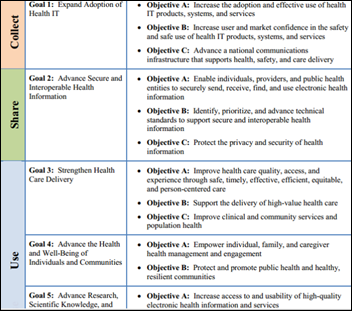
ONC will hold its annual meeting February 2-3, 2015. The email announcement caught my eye in mentioning that “the two-day meeting will gather over 1,200 health IT fans,” but on the registration website, it had been toned down to “health IT partners.” The event includes “an exciting panel of ONC’s former National Coordinators,” according to the email. I’m not sure if that’s enough of a draw to convince me to head to Washington in February. If you’re planning to attend, keep us in mind for rumors and newsy tidbits.
GE Healthcare announces its Centricity Live 2015 meeting April 29-May 2, 2015 at the Walt Disney World Dolphin Resort. Keynote speakers include Atul Gawande, Melissa Etheridge, and LeVar Burton. That lineup looks pretty good compared to some I’ve seen. I stayed at the Dolphin a couple of nights before HIMSS and it’s in a minimally mousey part of the Disney compound. Given the recent weather in my neck of the woods, I’m sure by April I’ll have a complete deficiency of Vitamin D, so if anyone wants a sassy traveling companion, let me know.

My good friend Anjali called last week asking for a favor. The annual Christmas Party at her hospital (it’s a faith-based institution, hence the name) was looming. Her husband had to travel and she didn’t want to go alone. She’s run three half marathons with me and has had my back in countless clinical situations, so how could I say no? She works at a hospital across town where I only know a handful of medical staff members, so I was looking forward to a holiday party where I could have a couple of glasses of wine without being interrogated about our EHR.
We were a little late heading out. She had picked up a dose of flu vaccine from the local retail pharmacy and was planning to vaccinate her daughter. The pediatrician’s office was already out of vaccine and the pharmacy won’t vaccinate children under 8 even with a physician’s order, so she decided to get creative. Unfortunately, she’s a surgeon with few pediatric vaccine skills, so I was persuaded to step in.
It’s a sad commentary when you have to work the system to vaccinate your child. Most parents don’t have that option, but I was happy to help. Needless to say, that vaccine won’t be making it into the state immunization registry, but I did email her the Vaccine Information Statement so I don’t run afoul of the feds.
The tables were packed when we arrived. We grabbed the first open space we found. We were next to a husband/wife physician couple – she’s a radiologist on staff and he’s an internal medicine physician elsewhere in town. The odds of a physician conversation (regardless of setting) eventually turning to EHRs and healthcare IT is nearly 100 percent if you talk long enough, and tonight didn’t disappoint.
The radiologist is pretty happy with the hospital’s system. She appreciates being able to view the entire patient chart when there are questions about what an ordering provider hopes to achieve with a diagnostic test. She also enjoys not having to help the radiology staff decipher cryptic physician handwriting.
Anjali told them she preferred handling patient messages from home after her daughter goes to bed rather than having to stay in the office. A couple of other people chimed in and I thought for a brief moment that the EHR love fest might continue in the spirit of holiday togetherness.
The bubble was burst when the internal medicine physician started complaining about his EHR. He complained of the burden of data entry with little return. He said he didn’t understand why there wasn’t any data exchange with other practices or hospitals or why he doesn’t have access to reports on his patients’ health status.
I asked a couple of questions about his practice and his system and was able to deduce that he is actually on my hospital’s platform, through our affiliate subsidy program. Anj picked up on this as well and gave me a little eyebrow raise. She knows I led deployment of our private HIE more than six years ago and that our users regularly exchange data between owned and affiliate practices as well as our multiple hospitals.
She’s also on the same ambulatory EHR although on a different platform, so was able to provide some positive counterpoints to keep him from going too far. I didn’t want to reveal myself as the owner of the platform due to the potential for turning a holiday gathering into a debate, so I excused myself for another glass of wine.
Most of our providers are satisfied with our system and are seeing the benefits of our patient registries, actionable reports, and interoperability. I’m going to need to get to the bottom of why his practice isn’t having a good experience and figure out what we need to do to get them to the same level satisfaction. I’ve reached out to our affiliate program manager so that I can review his implementation documentation and support tickets to try to identify what might have gone awry. I just wish I had heard about it through or formal processes rather than as an aside at a party.
Anj has never seen me in full Administralian mode and told me she was impressed at how I kept my cool while the physician was ripping apart the system I’ve spent the better part of a decade implementing, optimizing, and personally ensuring that practices receive value for their efforts. I must say I haven’t always been unflappable in these situations, but they have become easier over time. I’ve learned to pick my battles and not let situations get out of control.
We did enjoy some seafood and a nice string quartet, as well as good conversation with other physicians.
Have any strategies for enjoying the company holiday party? Email me.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.








































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…