Peter Smith is CEO and co-founder of Impact Advisors of Naperville, IL.

Tell me about yourself and about the company.
I’m the CEO of Impact Advisors. We are a consultancy that’s dedicated to healthcare process improvement and technology consulting. That’s pretty concise, right? [laughs]
Many people say there’s flux in healthcare IT consulting as firms that are focused on staff augmentation and implementation work are are finding reduced demand for their services. How would you characterize the industry?
That observation is absolutely true. The market has shifted over the last year, and for reasons you don’t suspect. We went from an environment where the industry was doing large, foundational projects, particularly EMR replacements and revenue cycle replacements. The market shifted over the last year as those projects wound down. It’s now moving towards post-implementation optimization and scrappier, more nimble projects. Things like optimization, back to advisory services.
The quick answer is that observation is exactly what I think the market’s feeling. It’s hurt a lot of consulting firms.
What’s the future for those companies that are scrambling to find something new to keep their people busy?
Their evolution will go something like this. They’re going to try to weather this market to the best they can. They’ll probably downsize. They’re going to explore alternative channels through subcontracting relationships and things like that. They’ll try to hold on to their business as best as they can. But at the end of the day, I think it’s going to diminish for them.
The ones that can transform themselves from single, staff augmentation kinds of services into the next generation firm will survive, but it’s not going to be easy for them. I would suspect that the next year or two is going to be challenging for a lot of those firms.
Everyone who has been in healthcare IT for a while knows that the pendulum always swings back. Will it swing back from EHR implementation and Meaningful Use to something else?
Yes. The pendulum is definitely swinging. There will still be an EMR replacement market out there, but it’s just not going to be as robust as it was. The core business will still be there, but the market is going to shrink. There’s going to be a lot of merger and acquisition activity.
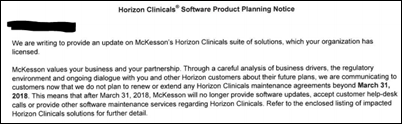
There are replacements of a number of systems out there. The dominance of core players – Cerner, Epic, and Meditech – is fueling potentially a replacement of some other vendors. That dynamic will continue — it’s just not going to be as crazy as it’s been the last couple years. That’s one component of the market.
The other one is the shift to optimization services, although that’s a wide definition. Basically optimizing the EMRs and clinical systems already put in is going to be a continued emphasis for a lot of organizations and a continued business for a lot of consulting firms. Rev cycle replacements will be another key driver.
Those are things that will continue to fuel the consulting market. But I don’t think we’re going to see the kind of growth we have in the last couple of years. It will be slow and steady. That’s healthy for the market and for the industry. We’re looking forward to that.
Impact Advisors is an Epic partner. Does Epic have weaknesses it needs to fix or that other vendors can exploit?
Epic’s a really strong company. They’re doing a lot of things right, as are a number of other companies such as Cerner. I don’t see necessarily any weaknesses.
Our clients are typically concerned about Epic’s tremendous growth over the last couple of years. It’s both an asset and something to watch as you think about implementation with Epic, but they’ve been able to mitigate that risk pretty well. For the services that they typically provide and implementation, they still do a very good job.
Clients still have to be focused on their side of the work in terms of understanding the process and the operations of a hospital. Those are things that any vendor is not going to bring to the table. That’s a void that the client has to step up and fill as well as the third-party consulting marketplace, and that’s where a lot of folks have spent their time.
I don’t know if I necessarily see any weaknesses. I think you’re seeing the emergence of a couple of players in the vendor space that are going to continue to be very successful, Epic being one of them.
Are clients happy that they invested what it costs to implement those expensive systems from Epic and Cerner, especially with the ongoing maintenance costs?
The basic answer is yes, although it’s certainly a topic of conversation in the C-suite about the level of investment that they’ve made and the level of expense. Given the dollars and the prominence of these decisions in the executive and board level, it is clearly top of mind.
But at the end of the day, if you look at the last five years, the clients that have been through the implementations and are in steady state and now reaping the benefits of that investment are extremely happy. In fact, I think there’s even a sense of appreciation that they’ve been through it already.
It’s the clients now that are looking to just start that journey. There’s a lot of anxiety because they know they have the investment ahead of them. They know they’re getting to the tail end of the curve. Their competitors in the market have gone before them and they’re a little bit on the outside of the bell curve. That’s where the anxiety is right now, not necessarily on the people that have already done it.
It seemed a few years ago that we had nearly figured out interoperability, but it’s probably more contentious and more frustrating to people now than it was then. Where does it stand and where is it going?
It’s one of my personal disappointments. I had expected this industry to mature a lot faster, particularly around the technology associated with interoperability.
But at the end of the day, interoperability is a very interesting concept or philosophy because it’s not just technology. You’re getting to the core of whether organizations really want to interoperate. You get into the competitive dynamics in a marketplace. You get into what’s in the best interest of the patient. This is bigger than just technology.
By and large, the technology is starting to work. Arguably, there’s not that set of standards in the industry that’s implementable, and I would agree with that to some extent. But the ability to interoperate is technically feasible, and in some cases, organizations are doing it very well and some regions are doing it very well.
It’s bigger than just technology. It’s bigger than applications. It’s also politics. It’s a competitive aspect between providers and hospitals and having the incentives aligned to really interoperate. It’s a big one. Personally, it’s I think one of the disappointments of the industry that we haven’t been able to do a better job of doing that.
Given that providers have little incentive to share information with competitors and patients don’t have much of a say, should ONC be bolder about dictating interoperability standards or requiring that providers actually practice interoperability?
I generally think the market should dictate some of this more so than the government. The government can certainly give us a good head start, whether it be ONC or any other agency, and set the direction. You’ve obviously seen a lot of indirect influences and incentives by the government just through Meaningful Use and ICD-10 changes and all that that is clearly steering our industry in the right direction.
I think personally as an opinion that the market, our providers, our clients, and our consulting firms have a market-based obligation to take it to the next level. That’s getting it down to the tactics and the technology and the specifics around making it work.
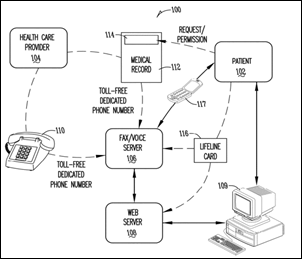
The other dynamic is that patients are getting much more savvy, demanding, and customer-centric. I hope that that side of the market influence will be a catalyst to dictate some change in the industry. You’re already seeing that and it will continue to accelerate as patients are demanding more from their electronic experience with their providers. I think you’re going to continue to see it.
In essence, long-winded answer, but all the dynamics need to converge, whether it’s the government, whether it’s the market, or whether it’s patient and consumer influences that are going to take us in the right direction. The signs are there. Now we’ve just got to finish the journey.
Epic users in specific regions seem to talk a lot about sharing information with each other. Is it really that much different compared to, say, Cerner users?
I really don’t think there’s a difference. Just because the two vendors that you cited, Cerner and Epic, have such a large market share, you can find examples of really good interoperability between not only organizations with the same technical platform — whether it be Cerner or Epic — but even among Cerner and Epic. Just given their percentage of the market share in this country, you find good examples of both. I can’t necessarily say there’s a difference.
I know that there’s a lot of debate on that, certainly in the Epic world. But I think Epic would tell you that they interoperate better than any other vendor just based on the volume of transactions going back and forth. It’s a delicate balance, but you’ll find good examples all over the country. You’re starting to see that the influences that are going to dictate integration are probably less about technology and applications now and more about the competitive climate that you’re in.
Cerner has built an amazing business and is expanding into areas such as health management. The company is so big now that it has to find new ways to keep growing. Where do you see them going?
I give Cerner a tremendous amount of credit for their business strategies over the last couple of years. Not only are they tremendous competitors in their core space of EHR and now emerging revenue cycle and ambulatory products, but they also diversified their service portfolio. They got into consulting. They do a good job with their consulting environment. They also got into remote hosting and application management services. They’ve expanded internationally.
That’s an example of a company that not only is doing what they did well from a core standpoint, but also diversified their service and business model and continued to be very successful. I think you’re going to continue to see the same. I think what you’ll see with Cerner is a continued refinement of some of their core products, particularly around revenue cycle and their ambulatory and physician practice management applications, and that will be part of the next generation.
You’ll also see a tremendous refinement of their business analytics capability. Their partnership with places like Intermountain Health will give them a tremendous opportunity to improve that side of their portfolio. I think all good things ahead for Cerner.
We seem to have an overwhelming number of startups, accelerators, and companies nobody’s ever heard of that suddenly claim they’ve figured something out. Where do you see them being successful in enterprises as opposed to the consumer side?
I see a lot of startups in the area of, obviously, analytics and business intelligence. You’ll see them in patient engagement. You’ll see them in products around revenue cycle. Those seem to be the cottage industries of these pop-up software and consulting firms.
This will follow the same trend as the HIS or EMR markets over the last 20 years. The market will rationalize. There will be winners. It will slowly self-select down to a set of players that will be viable market contenders.
Let’s take the business analytics space. I call that the Wild West right now because you have so many of these products out there that are generally focused on solving one component of business analytics. They might be doing Meaningful Use quality indicators or they might be doing patient engagement statistics. They all come into this space at a different place. What they’re trying to do is broaden their portfolio to be a full-service provider of business analytics and analytics capability.
You’re starting to see some winners in that space right now. As they broaden their portfolio, as the market rationalizes, you’ll see a handful of winners in any one of these markets. That’s what I think will happen and I think that’s going to accelerate quickly. The market condensing right now is going to put a tremendous stress on the players that don’t have a viable business model or a viable product and they’ll wash out. You’ll see a rationalization of the market relatively quickly.
People seem less enchanted with Meaningful Use. Is ONC’s influence diminished?
Diminished is probably a strong word. They’re obviously going to be a major player in trying to not only shape policy, but the incentives and dynamics moving forward with subsequent releases of Meaningful Use. Diminished is probably the wrong word.
But market influences will accelerate. ONC’s direction, the government’s direction, and market influences are, I hope, aligned. You’re starting to see that they are aligned. Perfect storm is the wrong word, but you’re going to see a series of influences — whether it’s ONC, market forces, or consumerism — that are going to drive the industry in the same place.
So not necessarily diminished, but you’re going to see the prominence of the consumer side, particularly around employers. Employers are going to take a much bigger stance. Payers are going to take a much bigger stance in influencing the market and certainly the provider side. You’re going to see not so much a diminishing of the government influences, but an increasing of the other influences that are shaping the industry and a consistency on the other influences.
What do you read into the acquisition by pharma services vendor Quintiles of your consulting competitor Encore Health Resources?
It surprised us. We obviously watch the market and we watch our competitors and Encore has always been a great competitor with great leadership and great talent. So quite honestly, it was a surprise to us.
I’ve seen other of our competitors, friends, and colleagues on the consulting side that have taken different directions, which I applaud because there’s synergy in terms of some of their acquisitions and mergers. But quite honestly, the synergy of that acquisition wasn’t as apparent as others, I guess I would say. So yes, it surprised us.
Impact Advisors is part of the Epic-IBM bid for the DoD’s EHR contract. What effect will that project have on the overall industry?
It’s obviously a huge project, so I think it has the ability to be a very big influence.
First of all, it’s going to be a tremendous opportunity to influence healthcare in our country for the patients, the military families, and the military personnel that that system serves day in and day out. We’re excited to be a part of that bid. At the very utmost, it has the opportunity to be transformational for the healthcare service of our armed services. That’s number one.
Number two, on the industry side, I think it’s an $11 billion project, moving probably north of that over the next 10 to 15 years. As I think someone in the military told me, they said it’s going to be the largest government award that doesn’t involve steel or putting something into space. That gives you a sense of the magnitude of the project.
We’re very excited to be part of it. I think it has the opportunity to be a major game changer, certainly for the armed services and the families that they serve. We’re proud to be part of that bid and we’re looking forward to hearing about that award.
What trends are you seeing from your broad exposure that might not be obvious?
The influence of the reimbursement market will have a tremendous impact on what happens in a technology space. What many of my clients call a tipping point or a pivot point is about to happen. That’s the true conversion from volume to value. You hear a lot of buzz terms around that, but basically the concept of being paid for quality rather than volume. That’s going to happen. We’ve been predicting that over the last couple of years, but we’re accelerating towards that.
When that pivot happens, it puts a tremendous premium on two things. One, provider organizational leadership. The leaders of the hospitals, IDNs, academics, and children’s hospitals are going to have to lead in a way they’ve never lead before. They’re also going to have to have a set of partners that they’ve never had before, primarily the payer side as well as other partners in their region and community. It’s going to be very interesting to see how that all manifests itself. Not only will be an organizational change, it will be a structural change. It will require leadership change and ultimately all the way down the line to technology changes.
We’re excited about it. We think that kind of change is good for the industry, it’s good for healthcare, and ultimately it’s good for the firms that are serving that industry.
Do you have any final thoughts?
This is going to be a tremendously fun industry over the next couple of years. I don’t think we’re going to experience more change than we are in the next couple of years. It’s going to be fascinating and fun to be part of that. Healthcare is the most fascinating industry out there because of the dynamics and influences.
























































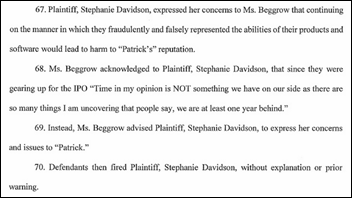














I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…