EPtalk by Dr. Jayne 2/20/25
As someone who has been practicing medicine via telehealth since pre-pandemic days, sometimes I am placed in the wise elder role and asked to explain how things started and how they came to be the way they are. It can be a bit of a journey down memory lane, but then again, everything changed when COVID arrived and telehealth will never be the same.
Although large healthcare delivery organizations see telehealth as an extension of what they are doing in brick and mortar facilities, players in the direct-to-consumer space have dramatically shifted the options that patients can choose from in their quest for prescriptions and other services. In my own practice, I’ve seen it shift from being a partnership between physician and patient to being a transactional consumer activity where an outcome is expected and the patient/consumer becomes irate if they don’t get exactly what they think they need.
This is often frustrating to physicians who are new to third-party telehealth and thought it would be an easy way to pick up some extra money while making use of the medical license they spent hundreds of thousands of dollars in tuition payments to acquire.
I was in an online physician forum the other day and this topic came up. A physician was asking what it’s like to work for one of the direct-to-consumer companies that is well known for prescribing medications for erectile dysfunction. The company has added pre-visit questionnaires to gather information, often with somewhat leading questions that coach for patient answers that will generate a prescription. It’s a win-win for profits since the company is selling the medications as well as the professional services.
In some states, clinicians don’t even have to interact with patients in real time. They can treat them based on the equivalent of a one-way message. The medical board of a neighboring state has disciplined dozens of physicians for this since it’s not allowed in their state, but that doesn’t seem to have dissuaded people from doing it.
It always amazes me to see physicians who have no idea what is going on in their own industry and have little visibility beyond their personal practices. I found a recent article about the phenomenon and shared it to the forum. It was clear based on the comments section that people were having their minds blown.
One of the facts from the piece that drew quite a bit of attention was that together, three well-known telehealth companies spent more than $1.5 billion on advertising, sales, and marketing in 2023. Physicians in the forum also had no idea that direct-to-consumer telehealth companies were getting into clinical conditions that involve more complexity, such as mental health or obesity.
One of the physicians in the forum is the chief medical officer at an online weight management program. It works strictly through payer-based contracts and provides a multidisciplinary care team to address patients’ varying needs. She shared horror stories about patients who came to them after being seen at more commercial enterprises, where patients were basically told to use the medications that were shipped to their doorsteps but weren’t given any other counseling or support.
She made some great points. It’s not just that the treatments are ineffective, but that in some situations, they introduce side effects, including metabolic abnormalities that could have been avoided if a more thorough evaluation were performed prior to treatment.
Patients don’t always understand the knowledge and experience that is behind why physicians do or do not recommend a treatment. That’s especially true when they have seen dozens of influencers and paid spokespersons tell them exactly what they “need.” They don’t know the difference between one obesity management telehealth company that only hires physicians who have extensive formal training and years of experience in weight management versus another that is willing to onboard any licensed provider who willing to sign on the dotted line and accept $20-$30 for writing a prescription and a brief chart note.
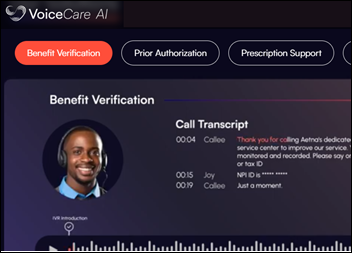
The article has some great comments from Ateev Mehotra, MD, MPH, a public health professor who focuses on telehealth. He describes the transition from patients who work with their physician to make a treatment plan to a situation where the patient makes their own diagnosis and consults a transactional service whose clinician is a screener who is paid only to make sure that the medication is safe for the patient. That’s the lowest possible expectation for healthcare.
Not to mention that “safe” is a relative term. Is it safe because it probably won’t kill you? Or is it safe because you aren’t likely to have complications that dramatically impair your quality of life, whether briefly or for a longer period of time?
The article mentions situations where a screening-type approach might make more sense, with one of them being the provision of reproductive health services. Especially in states where it might be difficult to obtain reversible contraception, those services can be popular.
For medications that are over the counter in many other nations but remain prescription-only in the US, it’s easier to see that the risk/benefit equation for certain drugs might tip in favor of more streamlined access. I don’t have the statistics in front of me, but would bet that for many healthy non-smoking females in their 20s, the risk of morbidity and mortality from oral contraceptives is likely less than that of pregnancy, given the current state of maternal and infant health in the US.
I’m looking forward to seeing how the conversation unfolds over the next couple of days, which is about the typical length of time one of these threads survives. I’ll certainly make note and share if there are any particularly thought-provoking comments.
I enjoyed reading Mr. H’s recap of one of the Donors Choose grants in which reader donations provided microphones and speakers for a classroom in North Carolina. In addition to students being able to hear their teacher and peers clearly, learning how to use a microphone properly is a life skill that everyone should have.
Conferences that I’ve attended usually have microphones distributed throughout the audience to ensure that people can be heard when they ask questions. Invariably, at least one or two people will declare, “I don’t need the microphone.” They try to talk loudly, but don’t succeed, or they inadvertently sabotage the recording or broadcast for attendees who are not in the room. Some hold the microphone too far away from themselves or place it right up against their lips, both of which are never great for the audience or others who actually would like to hear what the speaker is saying. Hopefully incorporating those skills into the school setting will pay dividends for those students down the road.
If your organization expects you to confidently approach the microphone, do they provide any instruction in how to effectively do so or to avoid the dreaded screechy feedback? Or do they just hope you were a member of the A/V club in high school or that you channel your inner rock star? Leave a comment or email me.

Email Dr. Jayne.
























 .
.



There was a time when my company went through multiple rebrands. These were relatively minor shifts, but completely unnecessary. It…