Howard Messing is president and CEO of Meditech of Westwood, MA.

Tell me about yourself and the company.
I’m CEO of Meditech, one of the founders of the EHR industry. I’ve been here for almost the entire history of Meditech. I have a very strong technical background. I think if you looked in the dictionary under “computer nerd,” you’d see my picture there. I’ve been here since 1974.
Combined with my computer nerd background, I’ve also dedicated my life to the healthcare industry and making sure that we can proceed and use our systems and electronic health records — although we didn’t call them that back in the early 1970s — to improve care, improve productivity, and hopefully control costs, though we know that’s been a continuing challenge for the entire industry.
I always like looking at those black and white 1960s pictures on your site, like seeing Neil Pappalardo up to his waist in water trying to save the data center.
Believe it or not, that was actually in Phoenix. People don’t think of floods in Phoenix, but that was a water main break.
How many hospitals run full-blown Meditech hospital-wide?
We actually have very few customers any more who have just one or two products. The vast majority of our customers are dedicated to our entire portfolio. We have somewhere around 2,300 or 2,400 hospital sites worldwide running our systems.
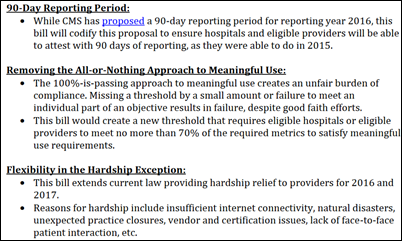
When we last spoke a few years ago, you priority was to move customers off older product versions like Magic. How is that progressing?
That was the priority then, and to be honest, it’s still a priority. The staying power of our older platform has surprised us. We still have approximately 800 customers on our oldest Magic platform and a similar number, perhaps even a few, more on our Client/Server platform. We have close to 600 on our 6.x platform.
We have a brand new platform. 6.x is the underlying technology, but we’ve redone the entire front end of our products to be Web- and mobile-based for the ambulatory solution and for the clinicians on the inpatient side. It’s really quite a brand new system.
Unfortunately, when many people think of Meditech, they think of our systems that were introduced 20 or 30 years ago because that’s still the bulk of our customers. Keep watching us, because we’re introducing brand new products that are quite different than the rest of the marketplace.
Do you still have to make the argument that customers should value the benefits of software rather than having the latest, coolest underlying technology?
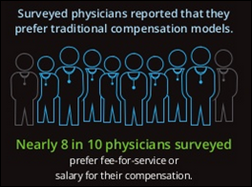
I agree with that in general. One of the main issues right now in EHR, maybe the main issue, is while keeping patients safe, we want to make sure that clinician productivity is not hurt. For the last 10 or 15 years, the entire industry has been saying, “Go to our systems and you won’t lose any productivity.”
We think that’s the wrong message. We want to say, “Go to our systems and we’ll improve productivity.” We think by adopting modern user interfaces — we’ve achieved that and have some numbers to back it up — that’s going to differentiate us moving forward as these products get adopted.
Articles that blame EHRs for physician dissatisfaction usually fail to differentiate between community-based providers who have occasional interaction with one or more hospitals and those physicians who work full time in a hospital. How did your studies measure productivity?
I’ll first add that the other issue we see with physician dissatisfaction is the change in what is required of physicians over the same period of time that we’ve been adopting EHRs over the last five to 10 years. It’s sometimes difficult for physicians — and it’s difficult for us — to understand how much of their dissatisfaction is due to poor implementations of software from vendors and how much of it is due to the fact that they are required to document more, provide more statistics, and do more inspection of data. Maybe some will view that as an excuse, and perhaps it has been.
When we look at productivity, what we look at is the very standard kinds of measures. How long does it take a physician or clinician to get through an encounter? One good measure of that is clicks or taps. We have a customer who has done a study looking at the older systems and then looking at our new Web-based product. They found there’s about half the number of taps or swipes than there were with the older systems’ clicks. The amount of time it takes them to get through an encounter is approximately half.
We don’t have the firm data to back it up yet because it’s a new system for us. We only have four or five Web-based ambulatory systems up and running. Our Web-based acute care system is actually just being delivered this summer. We’re pretty excited about the implications that will have for productivity of clinicians, of course while maintaining safety of the patients and providing the best possible care. Maybe as importantly, keeping costs within a reasonable realm.
How well is Meditech competing with Cerner and Epic in getting new customers and keeping existing ones?
We’re certainly keeping our old customers pretty well. We have a lot of old customers. Our maintenance revenue keeps going up.
We have seen a little bit of a pause over the last couple years in acquiring new customers as people wait for these newer user interfaces to be delivered. We’ve still managed to convince a fair number of our existing customers and a handful of new customers to join us in pursuit of this new product. We think that will pick up next year.
How do approach the market knowing that you have to displace someone else’s product?
That’s a challenge. It is very much not a new market, it’s a replacement market. We go in making the case that both our products can help increase provider productivity.
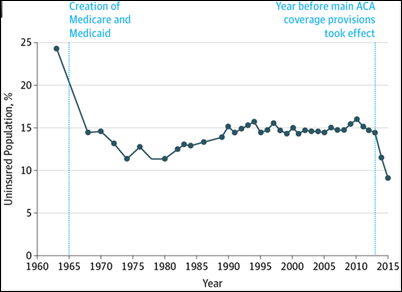
Then we also make the cost-based argument. We think that we are far and away the most reasonable total cost of ownership vendor of the three major vendors. It’s a little bit obscene the amount of money that some of the healthcare industry is spending on some of these systems. We can make a good dollars-and-cents argument that going with Meditech will save them money. Particularly when you consider that no matter who gets elected in the next election, nobody’s expecting our government or payers to be paying more for healthcare episodes and for healthcare in the future. As we move to population health, that’s a way of achieving better health, but also controlling costs.
In general, there needs to be some ceiling placed on what is spent on electronic health records. We think we have the right answer with that and that’s the major argument we make. You can get a new, modern system; a system that will increase your physicians’ productivity; and you can do it for less cost than with the other vendors.
Is it hard to get someone who spent dozens or hundreds of millions of dollars to implement Epic or Cerner to admit that they made a financial mistake and go back and replace it with Meditech?
If they’ve just spent the money, it’s hard. We have to make the argument as these systems age, although we have had some success with people who have made that commitment and then realized what they’ve gotten themselves into.
The company’s product revenue has dropped by around half since 2013, which directly hit net income. What’s the cause and how do you fix it?
Net income is down. On the other hand, we are still strongly profitable, still paying a dividend, and still giving our employees raises and bonuses. We have a very strong balance sheet.
A lot of this was anticipated as we moved towards the new user interface that we’ve provided for our products. We’ve seen a lot of people waiting to buy that. We also have lost a handful of customers to consolidation, where people are acquired. There’s not much we can do if they’ve decided on going with another vendor’s system. We’ve seen a slowdown in that loss.
This year, we’re doing relatively well. We expect that to turn around over the next 12-18 months as people start to see the effects of our new products.
Some of the market change involves hosting of client systems, which Cerner has built into a big business as Epic cautiously tests the waters. What does Meditech offer customers who want to turn over EHR system operations to their vendor?
We’ve actually offered, through third parties, the ability to do that for quite a while. There are a fair number of our customers who already are hosted by a third party, just not by Meditech. We’re also looking at whether we ourselves want to brand the entire system and provide it. We’re looking at some efforts, particularly at the smaller hospitals, and introducing that over the course of the next 6-12 months.
How do you see the potential change of ownership of McKesson’s Paragon product line changing the market?
I’m not sure it changes the market. I think everybody has been anticipating that McKesson was not very interested in pursuing their product line over the last 12 or 18 months. If this new arrangement involves a significant investment in R&D, perhaps they’ll be able to turn that around and become a significant force in the marketplace again. If they don’t do that, then I’m sure it will just be a winding down over time. I have no idea and am not privy to their deal to know what’s involved.
To be honest, we haven’t seen them as a very strong competitive force for two or three or four years. It’s very much a three-horse race on the acute care side among Epic, Cerner, and ourselves. Perhaps if you throw in the ambulatory side, there’s another couple of vendors that are strong and that we know are trying to get into the acute care space. The future clearly is in being able to provide services to the entire spectrum of healthcare — acute care, ambulatory, mental health, long-term care, urgent care, wherever healthcare is being provided. Particularly as population health begins to assert itself over the next few years.
Ambulatory was a perceived weakness of Meditech compared to Epic and Cerner. Is that changing?
Absolutely. I agree — we stayed away from the ambulatory sphere probably for too long. Then about 4-5 years ago, we acquired a long-term partner of ours, LSS Software, with the expectation that that might fill the gap for us. But we quickly began to realize that there were some issues with having a separate system. We bit the bullet, so to speak, and three years ago started developing our own ambulatory system and chose that as the testing ground of our new mobile and Web-based technology.
We’re happy to report that that product is now out in the marketplace. It’s live at four or five sites. We have orders for approximately 15 or 20 more of these systems. We see it as a big improvement on what our competitors offer, both in the functionality it offers specifically in the ambulatory space and also in the ability to integrate completely with the total healthcare enterprise.
Your Boston neighbors Athenahealth and EClinicalWorks are trying to push their way into inpatient from the ambulatory side. How do you see that developing?
Those were the two I was specifically thinking of when I said there are a couple of vendors trying to get into the acute care space. We’ll see what happens. They’re both good companies, both run by able leaders. We’ll see if they’re successful in getting into the marketplace.
Just as we’ve been learning about ambulatory and what it takes to provide an ambulatory system — and honestly there’s more to it than it seems when you first look at it – we think they’ll have the same kinds of experience as they push into acute care and learn that there’s a whole lot to it. We’re welcome to take them on competitively.
Some people think inpatient systems are just EHRs, but Meditech offers complete departmental automation rather than just maintaining a patient record. Will companies like EClinicalWorks and Athenahealth need to get out into the hospital department operations to be successful?
They really have to get out into the departmental operations. They will discover that those are pretty complex and difficult to do.
To be honest, in the future, I believe that with the rise of FHIR and other API technologies, that might not be as important. Certainly as a technologist, I think that eventually that’s the right way to go. I still think we’re several years, if not the better part of a decade, from actually having that kind of capability as standard in the healthcare industry.
When that happens, perhaps it will be easier to provide an EHR that doesn’t also provide departmental systems. For right now, those particular integrations — particularly between pharmacy and the rest of the EHR — are very tightly coupled. It’s difficult to see how you can provide that without going into the departments as well.
How would you assess the interoperability capabilities of Meditech and its two significant competitors and their progress toward offering APIs as ONC is emphasizing?
I don’t like to comment negatively about my competition, so I’ll just say that you couldn’t be more dedicated to interoperability than we are. We’re involved in all the major industry efforts to do that. We are one of the founding members of the FHIR effort.
We currently do, I think, as much if not more interoperability than anyone else. There are hundreds of billions of data transactions a year going through Meditech’s systems interoperably. I think the last time we looked it was 300 billion, with 200,000 different interfaces. We’re well on our way to already supporting interoperability, both because it’s required and actually because it’s the right thing to do.
The CIO of one of your highest-profile clients told me he was shocked at how easy it was to turn on interoperability with Meditech compared to the systems of a couple of your competitors that his health system also uses. Would that surprise people?
I don’t know if that would surprise people. It doesn’t surprise me, although I’d like to know who that is [laughs].
We have from the get-go always had an interest in interoperability. I used to give a talk maybe 10 years ago about how in “Star Trek” they get your medical records on the other side of the galaxy. If we’re going to be able to do that in 200 years, we have to get started now. We’ve been pushing for that.
It’s very pleasing to see that we’ve gotten as far as we have, particularly because the healthcare industry still doesn’t have, from my point of view, the right incentives in place to encourage people to interoperate. For the most part, it’s being done because it’s required as part of government programs. I think that that will change over time.
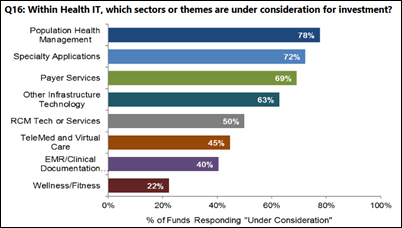
You mentioned the demand from customers for population health management and analytics. That market is pretty frothy, with a lot of companies popping up out of nowhere. How would you characterize the market for population health management and analytics and Meditech’s place in it?
I’m glad you asked that because we think we are a little bit different in our approach to population health.
First of all, it’s obviously currently one of the big buzzwords in our industry. It’s a clear trend to a way to manage patient population-based health. It’s going to become more and more important as our population ages and has multiple conditions and multiple chronic diseases. We think it’s an important thing.
On the other hand, there’s a lot of people playing on the fears of our customers and of the healthcare industry that if they don’t jump on the bandwagon right now with this particular model of population health, they’ll be left behind. We think population health needs to be a lot more integrated with the care delivery system than some of our competitors. Our approach is embedded in everything that we do. We’re taking a holistic approach to it, making sure that our customers can define and then manipulate and understand the various populations, no matter what their definitions are, as they practice their healthcare.
With the newly-announced MACRA regulations, it’s not even obvious that a physician can always tell which patients are in the population they’re responsible for and counting towards their statistics versus which ones are outliers that they are not responsible for. Our point of view is to give them that knowledge at the point of care, not on some separate list that someone has to compile and deal with on a different basis. We’re doing that by embedding that in their system. We have patient registries. We have a newly introduced analytics product that enables them to slice and dice the data about populations, but then build that into case management capabilities, build that into their revenue cycle issues, and maybe as importantly also relate to patient portal so that the patient can get involved.
One of the things about population health is figuring out how to get patients much more involved in their care. That’s been a Holy Grail. Nobody’s really achieved it very well yet. We want to make sure that we have all the tools in place to allow our customers to do that as we figure out how to get patients responsible for their own health.
Meditech’s executives all grew up within the company. How is their lack of industry experience outside of Meditech a strength when it comes to innovation?
It’s true that our most senior staff are from within the company, but we certainly do hire a lot of people who have not worked here before. We have a lot of smart people. There’s certainly no lack of outside ideas and influences.
In particular, over the last four or five years, we’ve hired a number of physicians into relatively senior positions here at Meditech. They certainly bring a lot of very interesting perspectives and ideas to us. We think that’s made a very big difference in the way that we approach development, implementation, and ongoing support. It’s been a bit of an eye-opener for a lot of us. That’s been a major factor in doing that.
There are both advantages and disadvantages to having long-term senior staff. We’re quite aware of that and try to capitalize on the advantages and make sure that we don’t get complacent about the things that are disadvantages.
How do you prepare for having executives and board members who have been with the company for 40 or 50 years turning it over to the next generation?
Obviously that’s one of the biggest discussions that our board has. We just appointed a new female board member. I wouldn’t be surprised if there were other board changes over time, looking for other people. We also just recently announced a new chief operating officer at the company, Michelle O’Connor, who is quite a bit younger than me and has not been here quite as long as I’ve been here.
We do talk about succession and the next generation. I’m not quite ready to retire. I don’t know that I’ll ever retire, but I certainly like to surround myself with a bunch of, I’ll say, younger people with good ideas. Talk about the future and make sure that the company traditions that are good are maintained and that the traditions that are not good are not maintained. Always ask the question when we do something. If somebody ever answers to me, “Because we’ve always done it that way,” I get very upset. We want to make sure that we’re justifying anything that we do and it’s not simply based on rote repetition of the past.
There’s quite a bit of overlap in the histories of Meditech and Epic, with one factor being that both companies have steered clear of the limelight with little interest in interacting with anyone other than customers and no real marketing or press presence. Epic seems to be opening up a bit. Is Meditech doing the same?
Absolutely. It’s one of the biggest things I’ve wanted to change in the five or six years I’ve been CEO. We’ve been working hard on it.
You touched on it yourself earlier when you pointed out that it’s a replacement market today, that it’s much more difficult to acquire customers. It’s also that the world in general is a much more marketing-oriented world. To be perfectly honest, we were founded by a bunch of MIT engineers, of which I’m one. I was here from the early days and we used to have the old mentality of, “If you build it, they will come.” Clearly that doesn’t work in the modern world, so we want to get our message out there.
Combine that with what I said early in the interview that we have a lot of older customers that we continue to support, but that means that many people continue to associate Meditech with our 20- and 30-year-old systems. We feel the imperative to get the word out that if you’re buying something new from us today, it is new. You’re not buying that 30-year-old Magic system.
All that has led us to believe we need to spend more time and more money on marketing. Hopefully, though, we’ll still be the relatively laid back, not overly slick vendor in providing that kind of information to the marketplace so they can make their decisions based on functionality and cost.
Where do you see the company going in the next five years?
In some ways, we’ll be doing the same things we do today. We’re dedicated to the healthcare market. We want to provide a complete, sophisticated solution for all the modalities of care.
There’s going to be a lot of challenges in healthcare no matter which direction our government takes. There’s going to be many challenges over the next few years. We want to make sure that our existing and prospective customers are prepared to handle that.
We need to polish off the new systems we have, extend those, then make sure that ancillary markets are also well served. In addition, I’d personally like to see our international share grow. We have close to half of the English-speaking market in Canada. The rest of the world is ripe to see the same kind of advances that we’ve had here in EHRs.
Do you have any final thoughts?
It will be interesting to see how the healthcare marketplace develops. We certainly intend to be a major player in how that transpires.



















































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…