Top News

President-elect Trump meets with the CEOs of Mayo, Hopkins, Partners, and Cleveland Clinic, with the topic speculated to be changing the VA to allow veterans to seek care at any hospital.
There’s also the strong possibility that the group tried to convince Trump to leave intact those parts of the Affordable Care Act that boosted the profits of big health systems by insuring people to whom they would otherwise be required to treat free.
Cleveland Clinic CEO Toby Cosgrove, MD, who is a Vietnam War veteran, is rumored to be on Trump’s short list to run the VA.
Also among the pod of rich, white males was facial plastic surgeon Bruce Moskowitz, MD (who founded the non-profit Medical Device Registry for reporting problems with surgically implanted devices) and the reclusive CEO of Marvel Entertainment, who had previously donated $50 million to the cancer center of NYU Langone Medical Center that is now unsurprisingly named after him and his wife.
Reader Comments

From Meltoots: “Re: readmissions article. It ignored the data showing that hospitals simply shifted readmissions to observation beds. Plus, the CHF death rate actually increased over the past several years as hospitals are penalized less for a death than a re-admit. It’s silly talk that the ACA reduced readmissions.” The readmissions penalty was too specific to have a predictably positive impact on patient care, being a primarily financial, incidentally clinical carrot (like other major payment methods that are driven by the patient’s midnight location). Providers have learned to play the Medicare shell game well, always finding a new way to preserve profits when the government removes one. Here’s one I was involved with at my health system. We quietly bought up some oncology practices, then made their patients come to the hospital to get their chemo infusions because it paid us better and we could milk the government’s 340B program to wildly increase drug margins. The patient, however, had to drive to our hospital (which had the usual stress-inducing lack of parking), pay a co-pay since they were now reclassified as hospital outpatients, deal with our often-indifferent registration people and financial counselors, and endure the bustle created when we funneled all those folks into hastily created infusion rooms that resembled happy ending-type massage rooms rather than places of healing. I would not have liked it as a patient — just being in a hospital would make me feel sicker and less hopeful than getting treatments in a quiet, pleasant doctor’s office. Our execs loved the idea, though, since it swelled our bottom line, which is the biggest ego stroke (other than erecting phallic, lavish buildings) that a C-level hospital executive can get.

From The Truth: “Re: Mercy Hospital in Des Moines. Fined over a million dollars for patient safety scores and that doesn’t make HIStalk? C’mon man.” I’m constantly surprised when readers complain that I haven’t mentioned some story that is unrelated to health IT and thus amply covered elsewhere. I guess I should be honored that folks expect or encourage me to write about other topics. The hospital gets three stars from CMS, a D from Leapfrog, and poor patient satisfaction scores, so naturally they announce that all of those measures use flawed data that underreport its medical pre-eminence.

From AnonTip: “Re: Deborah Heart and Lung RFP. I worked on it as a vendor. Some of the RFPs ran 800 pages as they demanded extensive screen shots of workflows and details, then required three days of on-site demos and then site visits. [Vendor’s name omitted] bid $40 million for the 89-bed hospital. They ended up choosing Meditech Web Ambulatory and 6.1, so they will probably dump Allscripts Touchworks at some point.” Unverified. They must have hired consultants to lead their search since it seems like overkill for a tiny hospital that has been using Meditech for decades, although maybe the threat of bolting gave them a stronger negotiating position. The hospital’s 2015 financials show patient service revenue of $163 million and expenses of $166 million, so I can understand passing on the one vendor’s $40 million bid.
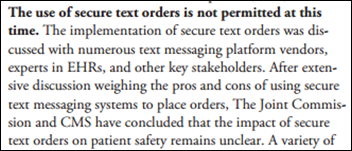
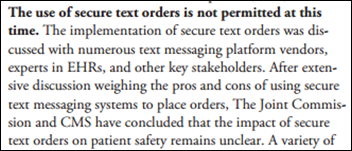
From State-Sponsored Actor: “Re: Joint Commission. They’ve flip-flopped again, now declaring that providers can’t send patient orders via secure messaging.” Joint Commission first banned sending orders via secure text messaging in 2011, then decided in May 2016 that it was OK as long as the messaging system met specific requirements. Since then, Joint Commission met with CMS and now declares, “The use of secure text orders is not permitted at this time” because its impact on patient care is unknown, specifically:
- How much nurse work is required to transcribe those orders into the EHR.
- The asynchronous nature of orders sent via text message requires extra steps to clarify and confirm.
- The transcribing nurse has to deal with any clinical decision support messages and relay them to the ordering provider.
From Kilt-Lifter: “Re: DonorsChoose. Do you personally fund the projects you mention?” Not usually. I mention projects in which readers decide to donate through me to enjoy the collective good will created when I share the stories of how the projects I funded with their money (and matching funds) turned out. There’s nothing in it for me and my personal donations are separate.
From Lookie Here Now: “Re: HIStalk email updates. I’m no longer receiving them.” This happens all the time as companies ramp up their protective defenses against spam and my email system cancels the recipient as “bounced.” Just sign up again since that often works.
HIStalk Announcements and Requests
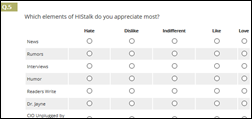
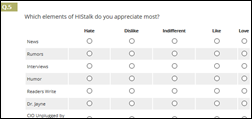
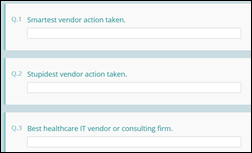
I’ve opened my once-yearly HIStalk Reader Survey. Like last year, I’ll randomly draw respondents for a $50 Amazon gift card. I was surprised in looking over last year’s responses how many reader-suggested changes I have since put in place, although some were just too ambitious for my energy level and capabilities and the #1 response by far is always “don’t change anything.” Some good suggestions from last year and my comments:
- Improve the site search. That’s always a challenge since Google Site Search doesn’t allow date filters, which would be really cool.
- Find an inside-the-Beltway anonymous writer. I’m not super-interested in government and politics, but I’m open to the idea if someone is interested.
- Write less about HIMSS (which is for vendors) and get provider input from AMIA. I don’t really have contacts in AMIA other than I was a member for a while, so I don’t have much to add there except occasionally mentioning something published in JAMIA that someone sends me.
- Get more input from “small people” like analysts or support desk people. I would love to, but vendor executives are paid to write guest articles and otherwise contribute visibly, while those in the trenches don’t have the time or the approval of their employer to participate. I wish that weren’t the case since I suspect they are at least equally interesting.
- Get more contributors. As in the item above, it sounds great, but even well-intentioned contributors quickly drop off as they realize the time required. One of my favorite sayings is, “I hate writing, but I love having written.”
- Do more polls. I will consider that.
- Send the morning headlines via an email update. I keep thinking I should do some sort of daily email update, perhaps using a separate mailing list so that it doesn’t bug those readers who aren’t interested. Given the previous suggestion, here’s a poll: Would you regularly read a daily email containing expanded HIStalk headlines? Last year, the most-loved HIStalk element was news, but clustered tightly in the next three spots were humor, rumors, and the morning headlines.
- Cover more conferences like CHIME’s spring and fall forums, ACHE, AMDIS, RSNA, and JP Morgan. Sounds good on paper, but I don’t get invited to these meetings and I don’t really enjoy attending conferences. The only one that’s appealing is JP Morgan and I’m pretty sure my low BS threshold would be overwhelmed by all the besuited money guys running around leaving an olfactory wake of expensive cologne and self-importance.

Reader Ed donated generously to my DonorsChoose project, allowing me to fully fund these teacher grant requests with double impact from matching funds provided by my anonymous vendor executive:
- Two Chromebooks for Mr. B’s middle school class in Phoenix, AZ
- A Chromebook and supplies for Mrs. I’s high school class in Orangeburg, SC
- Math kits for Mrs. V’s elementary school class in Norfolk, VA
- A library of 45 science and environment books for Ms. H’s third grade class in Anchorage, AK
- Two Chromebooks for the high school health education classes of Mr. S in Bay Shore, NY
- Two Chromebooks for Mr. B’s middle school class in Phoenix, AZ
- Shot puts and relay batons for the track team at Mr. H’s middle school in Las Vegas, NV
- Five sets of headphones, an electric pencil sharpener, and a programmable robot for Ms. S’s second grade class in Gladstone, MO
Ms. S replied this morning to the news that her project was funded with, “Thank you for kicking off our return from break in a great way! I can’t wait to share with the class that, because of generous people like you, we will now have some much-needed tools in our classroom. It is an amazing thing to be supported! It reminds us how valuable we are and impacts student motivation for reaching their unique potential.”
All the recent celebrity deaths made me envious of artists whose work lives on forever and finds new fans year after year, unlike the rest of us charge-leading foot soldiers who are simply replaced by the next warm body when we fall without leaving much of a non-family trace. I suppose the consolation is that it doesn’t really matter anyway once you’re dead.
Webinars
January 18 (Wednesday) 1:00 ET. “Modernizing Quality Improvement Through Clinical Process Measurement.” Sponsored by LogicStream Health. Presenters: Peter Chang, MD, CMIO, Tampa General Hospital; Brita Hansen, MD, CHIO, Hennepin County Medical Center. The presenters will describe how they implemented successful quality governance programs, engaged with their health system stakeholders, and delivered actionable information to clinical leadership and front-line clinicians. Q&A will follow.
January 26 (Thursday) 1:00 ET. “Jump Start Your Care Coordination Program: 6 Strategies for Delivering Efficient, Effective Care.” Sponsored by Healthwise. Presenters: Jim Rogers, RN, RPSGT, director of healthcare solutions, Persistent Systems; Charlotte Brien, MBA, solutions consultant, Healthwise. This webinar will explain how to implement a patient-centered care coordination program that will increase quality as well as margins. It will provide real-world examples of how organizations used care coordination to decrease readmission rates, ED visits, and costs.
Government and Politics
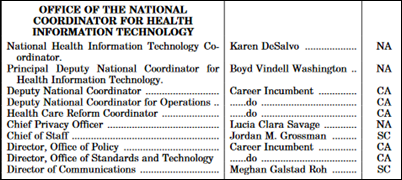
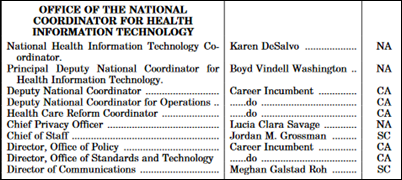
@Cascadia notes the existence of the Plum Book, which identifies presidentially appointed federal positions. Those marked NA are non-career appointment, CA is career appointment, and SC is a Schedule C listed appointment. Obviously it’s not quite up to date with correct names despite a December 1 publication date. Former National Coordinator Karen DeSalvo, MD, MPH, MSC is Acting Assistant Secretary for Health, which is noted as a PAS (presidential appointment with Senate confirmation) and she was never confirmed by the Senate, but I haven’t seen her officially say she’ll be leaving by January 20.
Privacy and Security
From DataBreaches.net:
- Brandywine Pediatrics (DE) is hit by ransomware, but recovers from backups.
- Desert Care Family & Sports Medicine (AZ) remains down from a ransomware infection that occurred in August.
- The Dark Overlord hacker who breached several healthcare systems earlier this year penetrates a precast concrete vendor and releases information that includes contracts, a dump of a manager’s cell phone that includes photos of his children, and video of an apparently fatal workplace accident. He or she is demanding extortion payments to leave the remaining information private.
- A hospitalized psychiatric patient breaches systems run by New Hampshire’s Department of Health and Human Services using a computer in the hospital’s library and posts some information of 15,000 people to social media.
- A hacker breaches the paging system of Providence Health & Services, posting some of the organization’s pager messages on the hacker’s website.
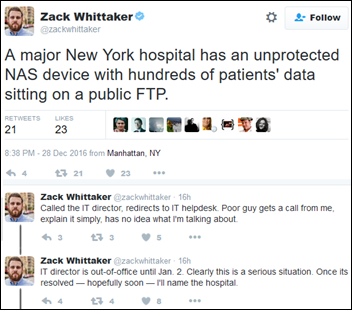
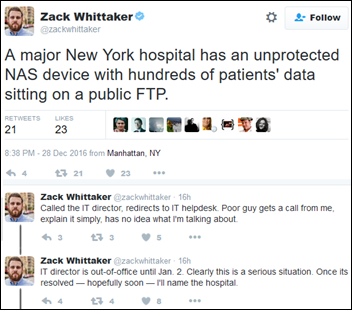
This ZDNet security editor is trying to contact a New York hospital to tell them that a network-attached storage device is open to public FTP, with no luck so far. Update: Saint Joseph’s Medical Center has taken the device offline, he reports.
Technology
A journal article describes how scientists use the workplace messaging tool Slack, which a geneticist user says is better than email that is “disastrous for group communication.” They’re using it to work on research papers, discuss conferences, monitor experiments via device integration plug-ins, create custom apps, award points for collaborative activity, create to-do lists, and train new members. Slack offers a free, endless trial, with regular packages priced at either $7 or $13 per user, per month. There’s also an open source, self-hosted alternative that offers a free team edition or an enterprise version for $20 per user, per year.
Other
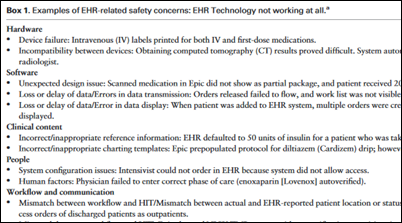
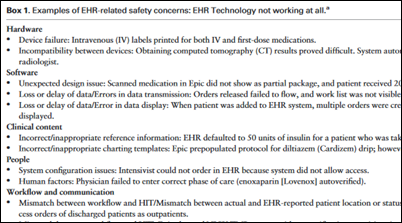
A JAMIA-published study describes the hospital-reported benefits of adding an EHR topic to daily executive safety huddles. EHR safety issues made up 7 percent of the safety concerns discussed in one year.

A study published in JAMA finds that US healthcare and public health spending increased significantly from 1996 to 2013 — now accounting for 17 percent of the economy – with the biggest costs involving diabetes, ischemic heart disease, and low back and neck pain. The biggest spending jumps were in emergency care and prescription drugs. The only injury that made the top 20 spending list was falls. Government public health spending accounted for just 2.8 percent of the total. It’s interesting that females incurred significantly higher expense – sometimes more than double – for all age groups over 15 in 2013, with their extended longevity and thus higher numbers incurring $130 million in the 85-plus age group vs. just $51 billion for males (although per-capita spending in that group was also 29 percent higher for females at $31,000 – maybe due to loneliness?). Overall cost ramps up smoothly until ages 65, which the jumps start to get dramatic and the challenges in funding Medicare in a mostly cost-unconstrained model become obvious, although the cost-benefit ratio of applying all those expensive treatments – not only to longevity, but also quality of life – is decidedly less certain. An accompanying editorial notes that the largest public health expense category is HIV – which kills comparatively few people – but little money is spent to address lifestyle conditions, some of which involve consumer products that are backed by massive advertising campaigns.

England’s Secretary of State for Health Jeremy Hunt touts the benefits of barcode-tracking and identifying patients, staff, and equipment that can prevent harm and provide data for studies.
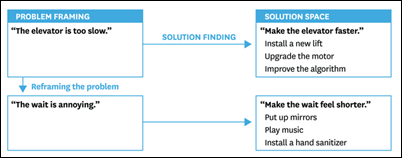
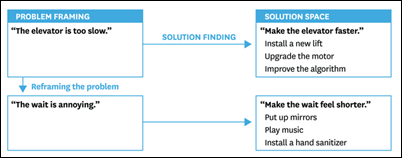
A Harvard Business Review article asks, “Are You Solving the Right Problems?” and questions whether frameworks like Six Sigma and Scrum or even root cause analysis and 5 Whys cause people to “overengineer the diagnostic process.” The answer, it observes, is often not a solution to the stated problem, and problem-defining technology or checklists can be “the subtlest of traps.” Sometimes Disney can’t speed up the ride wait, so it just entertains those waiting.
The Watertown, NY town ambulance service blames a computer upgrade for the inability of crews to open its narcotics lock boxes for several days. Ambulances from the next town over were called in when the drugs were needed. They probably could have just asked around since most towns have plenty of people stockpiling opiates.
A social worker fired by Erlanger Health System (TN) for not knowing how to call a Code Blue sues the health system. A nurse trying to revive an inpatient who had hanged himself in his bathroom asked the social worker to call a code. She says she had not been trained to do so and instead rushed to the nurses station, but found only a clinical documentation improvement employee there who didn’t call the code. She finally found five on-duty nurses in the break room, but they didn’t call the code, either. The hospital fired her for failing to call the code, for spreading rumors that the nurses were goofing off, improperly documenting the incident, and missing a meeting in which the incident was reviewed. The social worker claims racial discrimination since everyone who was involved except her is white and nobody else was fired.

In Germany, an unimaginative (and, much to my surprise, sober) 22-year-old imitates a viral YouTube video in trying to scare a sleeping friend by thrusting a running chainsaw near his head. The 18-year-old victim might want to find smarter friends – the chainsaw prankster missed that part of the video in which the saw’s chain was removed, leaving his unintended victim with a nearly amputated hand.
Odd: the HR director of home health software vendor Axxess Technology Solutions sues a company called Dicks By Mail (whose founder claims to have made millions from the insult-oriented business), seeking to learn the identity of the anonymous individual who sent her a box of penis-shaped candies. She thinks it may be the same unknown person who keyed her car and posted phony Craigslist ads about her. Ordinarily I would suggest that surely she must already know anyone who hates her that much, but then I remembered that she’s in HR.
Sponsor Updates
Blog Posts
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates. Send news or rumors.
Contact us.

















































It's nice when Epic takes on patent trolls and other bad actors in the industry. They do great when they…