Najib Jai, MD, MBA is co-founder and CEO of Conduce Health.

I trained as an MD, MBA but did not practice clinically and did not do a residency. Instead, I went directly to Oak Street Health. My entire career has been in value-based care. Conduce is focused on incorporating specialists into value-based care models through personalized referrals and contracting specialists under aligned value-based arrangements.
What does the primary care physician see when they refer a patient to a specialist?
It depends whether the PCP is in a hospital system versus an independent primary care organization.
At a high level, the way a referral typically works is that at the point of care, a primary care provider determines for a given patient that they need some sort of specialized care, whether it’s for their heart, their kidneys, or whatever that may be. After that is where there are a lot of heterogeneous workflows. The provider typically inputs into some system, whether that’s an EMR or some sort of separate referral management organization system, that the patient needs to see a specialist. Let’s call it a cardiologist.
From that point, either the patient is given information to go out and schedule that appointment with the specialist directly, or there’s some sort of care team that’s affiliated with the hospital system or practice that makes that schedule available for the patient on the patient’s behalf.
From the specialist standpoint, their reception of that referral largely is the same. They receive some sort of electronic record that a patient has been referred to see them. Then either that specialty practice or the patient gets a visit scheduled.
Compensation is a question that comes up a lot when we think about value-based care for specialists. Part of what made value-based care work well for primary care providers was that, relatively speaking, they weren’t compensated particularly highly. This idea of being able to create additional financial incentives to boost their income was particularly attractive, and we saw the results of it. There were a lot of PCPs who were willing to participate in these models.
Your average specialist is making three to five times more than a primary care provider, so you have to think about it less purely from a financial dynamic and more through a matter of practicing clinical medicine. The average specialist isn’t necessarily interacting with patients who are aligned with their specialty, which can be incredibly frustrating when you’ve spent 10-plus years of your life training to manage some of the more complex disease states that are out there.
Value-based arrangements enable these specialists to practice top of license to provide more comprehensive care to patients who need that specialist involvement in their clinical outcomes, which is a subjective or qualitative improvement in what they’re seeing where the more quantitative or financial dynamic may matter a little bit less.
Is the referring PCP notified when their patient has been scheduled to see the specialist, when their visit is completed, and what decisions were made?
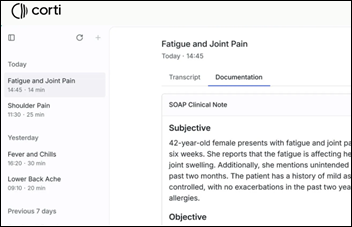
They don’t know any of those things. Anything that happens out of a primary care office, particularly as it relates to specialty care, is a black box. You don’t know when the patient shows up. You don’t necessarily know what care was administered or what tests were taken.
For the primary care provider, you don’t necessarily know how to adjust your care plan for that patient. When the patient comes back to see you in two to three weeks, particularly if they’re a Medicare patient 65 and older with some sort of comorbidity, you’re relying on that patient to tell you what happened with their specialist, if they actually saw a specialist.
In the most ideal outcome, they’ve got a great memory and maybe took notes, so they can essentially relay to that primary care provider everything that occurred. But more often than not, that doesn’t happen. Perhaps you don’t see the patient in three weeks, or perhaps it’s three months, and you really don’t understand whether or not that patient showed up with a specialist and what actually occurred in that visit.
That is part of the problem that we are solving. How do you make that black box a little bit more translucent so there is is more clinical co-management between these two integral providers for any given patient who needs to see both of them?
Is technology the reason that patient information isn’t shared in what could be an urgent or critical handoff?
It still is a technology challenge. Every specialty practice looks dramatically different. Believe it or not, some groups are still dependent on paper charts even if they do have some sort of EMR. If you are the primary care group sending patients out, how you actually receive data and information can be incredibly strained. Whether you’re trying to get someone from the specialist office to return your phone call, or more likely than, not return a fax, it can be incredibly challenging.
The crux of the issue is just how heterogeneous every single specialist or specialty office is within a given geography within the United States. It’s largely a technological problem. Given the fact that a lot of these primary care offices are already strained with managing complex patients when we think about value-based care and Medicare populations, there isn’t a whole lot of time to make sure that that works out particularly well.
From the specialist’s vantage point, there’s not a whole lot of incentive. Ultimately you can still manage and take care of your patients, absent of needing to take that additional step of going through all the complexity of reaching back out to that primary care provider.
But the one thing I’ll call out here, and maybe this is me putting on my clinician hat for a second, is that the stakeholder who suffers the most in that paradigm is the patient. Because ultimately, they’re having a series of disjointed clinical interactions, whether it be in a hospital system or a series of private practices, where no one is really speaking to one another. The patient isn’t well equipped to manage their care through that paradigm either.
Does the specialist expect or want to see the PCP’s information, or do they just assume that they will start from scratch, redo any tests or imaging, and trust the patient to tell them the rest?
Specialists would love to not have to rework every single patient they see from scratch. The cardiologist didn’t necessarily specialize in taking all the labs for a patient that relates to their electrolyte function for their kidney. They have no real interest in that, but when a patient comes without any sort of notes or information from the PCP, you’re starting from zero. That can be incredibly frustrating clinically. But again, there’s not a convenient or scalable way for that specialist to then go back to the primary care provider and obtain that type of data unless you’re in some sort of closed loop system.
As an example, hospital systems in some cases can do this particularly well because they’re all operating under a single EMR. Even if you can’t reach the primary care provider or the care team, you can go back to that EMR and evaluate what notes were taken and what images may have resulted. That streamlines your process as a specialist in theory, because they’re going through the pain of not knowing what is going on clinically with that patient when they arrive for their visit. You would think that would incentivize them to then go back after their visit with the patient and provide it to the PCP, but again, that connectivity isn’t there. Unfortunately, even if there were to be a desire to more clearly communicate with the primary care provider, there just isn’t a technological chassis in place to make that seamless.
Anyone in the health tech space will tell you that it’s oftentimes less about the technology, less about how efficacious that technology is, and more about the workflow. How can you make this easier for any provider who is managing patients to use this tool or to manage this particular action? Unfortunately, while there’s a lot of technology in some cases, there aren’t really a lot of great workflows that seem to embed well with what either a primary care provider or a specialist is doing to ensure more of that streamlined back and forth communication.
Isn’t doctors using patients as a data mule for potentially critical information a malpractice lawsuit waiting to happen?
It’s sad. It’s unfortunate. I go back to some of my clinical training on the south side of Chicago. There is a lot of onus on the patient to be this historian of everything that has happened to them. The more complex these patients get, the more history you have to keep track of.
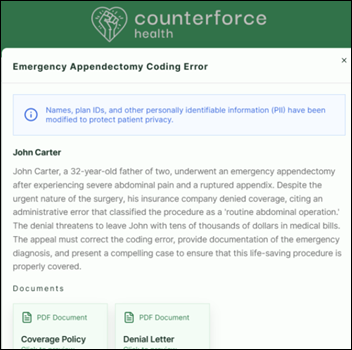
Most of the patients who are benefiting from value-based arrangements in Medicare don’t have great health literacy, so not only are we asking them to be historians, they’re not really equipped to do that particularly well. The result is meaningful delays in care or an absence of care that cause poor patient outcomes that are incredibly expensive, whether that’s a series of hospitalizations or the progression of a chronic disease to a point in which the morbidity and mortality rates rise meaningfully. We see that all the time in nephrology care.
That, unfortunately, is the current state. That is essentially what we’re trying to address, and more broadly, what value-based care is trying to address. How do we create the systems in place to prevent these types of outcomes? Discontinuous care is a big part of it.
How extensively are value-based care models being used that involve specialist referrals?
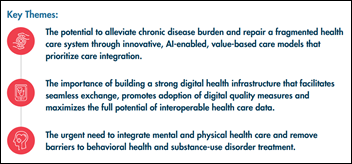
Value-based care is perhaps one of the more frustrating terms because it’s an umbrella term. It means a variety of different things. But most concisely, you’re essentially seeking to compensate certain doctors in these value-based care arrangements for the quality of care they provide versus the quantity of care they provide. That quantity dynamic is more akin to what we see in a fee-for-service paradigm.
To make it even more specific, what does that actually mean? How are you compensating quality? You put the financial responsibility on a single physician for the outcomes of their patient. If a patient gets hospitalized and it’s particularly costly, that actually impacts the financial well-being of the provider taking care of them, i.e., how much they get paid or not paid.
Prototypically in value-based care, for the past 15 to 20 years that it’s been around in its various iterations, that financial responsibility has been largely weighted on primary care providers, which intuitively made a lot of sense. Primary care is one thing. Theoretically, every Medicare patient should have a primary care provider, but in reality, it introduces a challenging dynamic, which is that 75% of typical medical spend, for primarily Medicare patients, is weighted in specialty care. We’ve put a lot of financial responsibility on a consistent stakeholder in a given patient’s experience, the PCP. But that stakeholder doesn’t necessarily have the influence to materially improve or impact finances for some of these patients, and put differently, the clinical outcome for some of these patients.
To go to the heart of your question of the implications of referrals, the moment you refer out to a specialist is not only that data and technological black box that I described before, but it introduces an unalignment when it comes to incentives. That initial primary care provider is highly incentivized when in value-based care to make sure that patient’s healthy, that they’re not being hospitalized, that they’re not costing a lot of money. That doesn’t mean an absence of care, because if you don’t do certain things, that also results in a hospitalization. It means in theory, trying to provide as holistic care as possible, inclusive of maybe wraparound services and nursing and whatever that might look like, particularly if you’re a hospital system and well equipped to do that.
But to that referred specialist, the specialist that a given patient was just sent to, it’s just being compensated for seeing that particular patient. Therefore, that specialist may very well do all of their typical tests. They might suggest a certain procedure. Let’s remove some of the presumed altruism in healthcare for a moment and think about it purely as a business. In that scenario, every single specialist should be incentivized to do as much as possible, because that’s how they’re going to be compensated particularly well. Now in reality, hopefully that doesn’t happen, but oftentimes it does. The implications of referrals and value-based care is that they typically are very expensive and not great for your bottom line historically in these types of models.
In the example of referring a patient to a cardiologist, the PCP would need to consider administrative factors, such as whether the specialist is taking new patients or whether the patient can get to their office. They would need to think about patient-specific factors, where one cardiologists might be preferred over another. Lastly, they have to think about cost and compensation under value-based care. What does that decision tree look like for the PCP?
I love that question and I’ll answer it in two ways.
The current state is that you are absolutely right in calling out that there are a lot of logistics that should be considered whenever referral is made. First and foremost, who’s available to see this patient in the meaningful amount of time. In the cardiology example, the referral is probably for congestive heart failure, if we think about what’s most prevalent in the 65 and older Medicare population. That’s a meaningful chronic disease in which if you don’t see that cardiologist soon, you might be hospitalized. Availability is really critical.
Coverage in Medicare is important, but in some cases, it’s less of a consideration. It depends on some of the nuances, such as Medicare Advantage versus traditional Medicare, but a little less relevant versus a commercial population where you have to think about who’s in network or out of network, but it’s still a consideration.
Then to your point, perhaps the most critical point is the patient. There’s a presumption even in clinical medicine that every patient with a given disease, let’s say heart failure in this case, is more or less the same. But the reality is that that could not be further from the truth.
I had a really good mentor in medical school who always said that evidence-based medicine is informative, but inherently flawed, because it’s based on the average patient, and no patient is the average patient. It’s a foundation to make decisions upon, but it should not necessarily be used as true.
Going back to your question, there are all of these different variables for a primary care provider to consider when making a referral, but keep in mind that the average primary care provider, even in a value-based arrangement where they’re incentivized to provide holistic comprehensive care, is still pressed for time. They have a variety of different patients. They’re trying to evaluate why this particular patient is there, what medications they have to make adjustments for, what additional appointments the patient needs to see them again. Of course, the patient isn’t just sitting there simply listening to the provider. They have things they want to talk about. Having spent time in clinical medicine, I can tell you that it’s a very focused encounter, but not often with a focused participant.
Saying all that to say that the reality is that when a referral gets made, oftentimes none of those factors are considered because there’s no time to consider them. To contrast that, how we think about it from a Conduce perspective is that we seek to embed ourselves in that workflow. Again, you can develop the best technology in the world, but if it’s not workflow friendly, it’s not going to matter to a given provider. We consider all of these particular elements based on our AI predictive model, and most importantly, understanding the patient.
When we think about what makes a good provider, we think about, is this doctor a good doctor or a bad doctor? That makes a whole lot of sense, but in clinical medicine, it comes down to the patient. We seek to understand patients first. We group them based on shared characteristics. Here are patients that have heart failure, diabetes, they live in this ZIP code, they lack transportation, and they predominantly speak Spanish. Those patients are going to do well with a particular cardiologist and not so well with another cardiologist. If the cardiologist doesn’t speak Spanish, that patient population I described isn’t going to do particularly well with them.
Our first product, the Conduce Referral Engine, incorporates all of those factors — who’s available, who’s within a reasonable driving distance, and then most importantly, who’s going be a really good fit for this particular patient – and provides that recommendation to that primary care provider at the point of care. They don’t have to sit there and manage the 20 different things that are happening in a 10 to 15 minute encounter. Instead, they have a convenient list of providers directly in the EMR in a closed loop hospital system. It can be a printout. It’s whatever that PCP is accustomed to for a workflow to streamline that process and make the best personalized decision for that particular patient.
What are your priorities for the next few years?
What we’re building here at Conduce is these personalized referrals. We’re connecting specialists into value-based care models, but to put it slightly differently, we are ushering in an era of personalized healthcare, this idea that you can understand patients and their unique characteristics to inform where they will get the best medical care possible. Our models right now are about as bad as they’re ever going to be. I don’t think they’re bad, but we can continue to improve them with more data, more patients, and more clinical outcomes.
What the next one, two, or five years looks like for us is that we continue to interact and improve the lives of more and more patients, accumulate more and more data, and become that much more personalized in ensuring that we don’t just find the good doctors and the bad doctors, but we find the best doctors for a given set of patients. That’s personalized medicine. I honestly think that’s both the future of medicine and what value-based care is all about.




































Traditionally Professional Courtesy is something that physicians gave each other - but we had to be careful with it when…