Top News
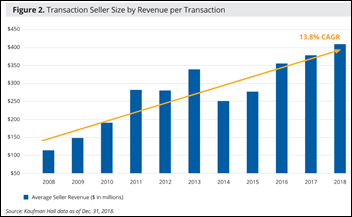
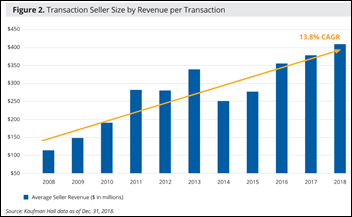
The average acquired health system had annual revenue of $409 million in 2018, according to a new Kaufman Hall report on health system mega-mergers. Seven billion-plus dollar transactions skewed the average upward.
Only 20 percent of the sellers were financially distressed, and 75 percent of the buyers were non-profit health systems that are anxious to grow.
Kaufman Hall lists several reasons that health systems are expanding, all of them involving improving their own business rather than patient care. It notes that the line between for-profit and not-for-profit health systems is blurring, such as HCA’s acquisition of North Carolina-based Mission Health that also involves funding a local non-profit health trust.
The country’s largest health system, HCA, operates 178 hospitals with annual revenue of $43 billion. It is focusing on markets with increasing population and low unemployment.
Kaufman Hall recommends that health systems expand in markets with high growth or strong demographics, seek strong operational or clinical partners, and increase consumer engagement.
Reader Comments

From GuyFromMadna: “Re: Apple. More power to Tim Cook if he can somehow use Apple Watch to solve the crisis of $300 insulin vials or $3,000 out-of-network ED visits. It took me back to Joe Biden’s precision medicine initiative – whatever happened to it?” No technology company or technology itself can solve our mess of a healthcare system and globally underperforming public health. Cook is one of these: (a) naive, which is probable given that companies that have delved much deeper into healthcare than Apple have met their Vietnam after confidently proclaiming themselves disruptors; (b) confusing a narrowly defined view of health that pertains only to a few undiagnosed and often harmless maladies of IPhone-only users; or the most likely answer, (c) desperately trying to feint away from Apple’s rapidly slipping relevance as investors get wary. Claiming that Apple’s best is yet to come and that it involves an industry largely unexplored by Apple is, to me anyway, just silly. Meanwhile, former VP Biden just delivered the keynote address once again at StartUp Health Festival in San Francisco, railing against data silos and most likely thinking about his inevitable presidential run. I haven’t seen any news from his Biden Cancer Initiative, just like I’m still waiting for MD Anderson to justify that “making cancer history” business (no pun intended). At least you know there’s no good treatment for cancer if even rich people are still dying of it.
From AnonymousPlease: “Re: Mid Coast Hospital (ME). Had an extended computer or network outage recently, accordingly to a family member who was told by their lab tech that the computers were down. Sounds like there was an HVAC alarm in the data center that was ignored (reset). By the second time, many servers had overheated.” The hospital’s Twitter account is frozen in mid-2017 and their Facebook doesn’t mention an outage. It seems odd that someone would ignore a data center cooling warning, so I speculate that maybe they shut the alarm off while trying to mobilize an HVAC expert to investigate and then had the temperature get away from them. It would be a tough call to proactively start turning off servers in that situation and they may not have had enough time to activate whatever failover plan they have. Modern servers should be good to at least 110 degrees F, but their individual thermal safeguards can be programmed to take them down at a user-defined temperature. It is, of course, a nightmare trying to recover individual software systems that went down hard even after the server they run on has been brought back online, requiring the enlistment of individual system experts to look at potentially corrupted databases, run disk recovery, free up phantom user sessions, and assess what information was lost.

From Sticky Wicket: “Re: [publication name omitted.] How did they get ‘Bret’ Shafer in rewording another site’s story?” Misspelling Brent Shafer’s name and omitting his Chairman title is sloppy, but I won’t call the writer out since just a year ago she was finishing up college and working as an office assistant. That particular clickbait-heavy news aggregation site seems to hire from a single demographic of freshly-graduated, female journalism majors. It has an audience, so there’s not much else to say.
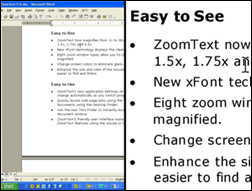
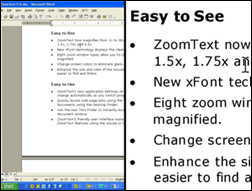
From Visual Acuity: “Re: National Federal of the Blind lawsuit against Epic. One of our residents is legally blind and can use Cerner using ZoomText, which we installed after trying the Cerner option that allows increasing some (but not all) font sizes. The resident has less flexibility since Zoomtext must be installed on individual machines and not through Citrix. I do think Cerner (and it sounds like Epic as well) could do a better job supporting accessibility even for physicians who aren’t legally blind, but who have reduced visual acuity.” Thanks for the tip on ZoomText. It offers a Windows-only screen magnifier, another version that includes reading screen contents and keypresses, and a super-product that provides those capabilities plus keyboard navigation, customization, and more expressive screen reading. It also sells a large-print keyboard with hotkeys that control its software. I agree that clinicians, especially those over 40 when presbyopia kicks in nearly universally, might find that their fatigue level, eye strain, and headaches from frequent computer use could benefit from a screen magnifier. I should also mention that Windows 10 has a screen magnifier built in – just press the Windows logo key plus the plus sign (or navigate through the Settings/Ease of Access menu options) – but I tried it and it seems laggy, although I haven’t tried ZoomText to compare. It’s hard to envision (no pun intended) how well a screen reader would work, however, so I don’t envy someone trying to navigate an EHR as the computer reads its screen contents aloud.
From Informed Consent: “Re: partnering with IBM. I have experience with a healthcare software vendor that entered a joint project with a large client of IBM. ‘Joint project’ means that IBM took full control with their leverage and contacts even though we were providing the core of the solution for which they had no alternative. IBM insisted on ‘handling the paper,’ which means they beat us down to a sub-share of the client revenue, then took 20 percent off the top of our portion for ‘taking the risk.’ They didn’t allow us to talk to the client (‘we have the relationship’). We got sucked into providing a reasonable quote for the work, then midway through, IBM said the client’s budget had changed and, ‘You need to cut your portion to $X for this deal to work.’ This happened three times in this one deal even though they wouldn’t tell us how much they were billing our customer. We were down to 40 percent of the original quote when the client cancelled. IBM’s motto is, ‘Our clients are our clients, and YOUR clients are our clients.’ Their salespeople kept wanting intros into our client base but wouldn’t provide the same. Our CEO was excited to get a call from the IBM sales team wanting a price call for a client with similar need. I warned that even though it was their lead and their paper, by the end of the call, they will demand that we give them a minimum revenue commitment, for which we will be on the hook for THEIR unvetted client. The CEO scoffed, but sure enough, my prediction came true in our first call.” I considered HAL – err, IBM — somewhat evil even before their current financial desperation and Watson missteps. I admire some of the technology developments, especially their inadvertent creation of the modern PC industry and Microsoft by botching the original IBM PC rollout by snapping together off-the-shelf components (the failed, proprietary MicroChannel architecture came after the horse had long departed from the barn). IBM eventually walked away from the now-commoditized business by selling the PC business to China-based Lenovo, which turned out to be a much better vendor.
HIStalk Announcements and Requests
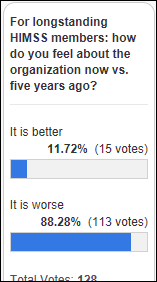
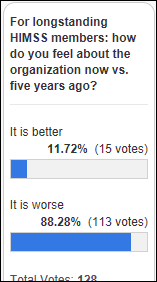
A convincing 88 percent of poll respondents who self-identify as longstanding HIMSS members say their feelings about the organization are less positive now than five years ago.

Gerald says that at least HIMSS now acknowledges that the annual conference is a “trade show” (or a “boat show,” as Jonathan Bush always said, although at least boat show attendees are spending their own money instead of someone else’s) instead of claiming that its primary purpose is education. He says he hasn’t attended a provider’s educational session there in the past five conferences, which is about the same as my own record.
A reader asked via a poll question what’s wrong with HIMSS. My answer as a longstanding member, off the top of my head:
- They run their operation like a dues-funded vendor, maximizing revenue at every opportunity.
- In fact, they really are a vendor, having acquired for-profit companies, conferences, and publications while somehow remaining a non-profit.
- They wildly overpay their executives compared to similarly-sized, non-profit member organizations (I researched this thoroughly years ago when Steve Lieber first hit the million-dollar annual compensation milestone).
- They sell access to their provider members to their vendor members in the “ladies drink free” model.
- Its “vendor points” system rewards the big vendors that are most willing to send HIMSS huge checks, giving those vendors the dominant voice over those that can’t or won’t pay more.
- Like most other member organizations, they get involved in government programs that have profit potential for their vendor members.
- They pay lip service at best to patients since there’s no money to be made in supporting better public health, outcomes, or access (much like their provider members, in fairness).
- Their media operation studiously avoids running anything that looks like real news unless it cheerleads the industry, filling the remaining empty space with inexpertly written filler pitching products and services that are always predicted to improve healthcare but somehow never do.
- They aggressively demand to be the voice of the industry even though, as in the case of the American Medical Association, many of the people in that industry aren’t members and those who are may not agree with the positions HIMSS takes on behalf of its vendor members and itself.
New poll to your right or here, as suggested by a reader: for provider IT decision-makers: which service do you consult before buying software or services?
Webinars
January 17 (Thursday) 1:00 ET. “Panel Discussion: Improving Clinician Satisfaction & Driving Outcomes.” Sponsor: Netsmart. Presenters: Denny Morrison, PhD, chief clinical advisor, Netsmart; Mary Gannon, RN, chief nursing officer, Netsmart; Sharon Boesl, deputy director, Sauk County Human Services; and Allen Pendell, SVP of IS and analytics, Lexington Health Network. This panel discussion will cover the state of clinician satisfaction across post-acute and human services communities, turnover trends, strategies that drive clinical engagement and satisfaction, and the use of technology that supports those strategies. Real-world examples will be provided.
Previous webinars are on our YouTube channel. Contact Lorre for information.
Acquisitions, Funding, Business, and Stock
More JP Morgan Healthcare Conference nonsense: the entire hotel area is so packed that the moneyed minions are meeting in public parks, restrooms, and the furniture department of a nearby Macy’s, with one hotel charging $300 per hour for a table and four chairs with no service. I didn’t really need more depressing examples of what America has turned into, but this one’s at least kind of funny as long as you don’t think about who’s paying.
Sales
- University Hospitals Cleveland Medical Center joins the global health research network of TriNetX.
Other

The conservative-learning National Affairs ponders “The Cost of Hospital Protectionism,” with the obviously brilliant Chris Pope (kudos, seriously – it’s a tough industry to understand and explain) making these points as he looks back on recent hospital industry history:
- The government has done little to reduce healthcare costs other than to shift the responsibility for paying them while protecting hospitals and encouraging them to inflate costs.
- Healthcare insurance is becoming increasingly unaffordable, with premiums tripling since 1999 and entitlements expect to consume 40 percent of the federal budget by 2047.
- Hospital overcapacity encourages hospitals to offer tests and procedures whose per-unit cost is high due to small volumes, often with poorer outcomes.
- The American Hospital Association promoted cost-based Blue Cross insurance during the Great Depression purely to fund the growth of the expenses of its members.
- When Medicare Part A was rolled out in 1965, the instant 75 percent payment increase encouraged hospitals to spend more on buildings, staffing, and technology. Within five years, total hospital spending rose 37 percent even though only 7.5 percent of the population gained insurance.
- Cost-based payment created a “medical arms race” in which hospitals built expensive facilities for expensive procedures, shifting themselves from “institutions of last resort” to all-purpose providers whose costs rose 345 percent in 10 years vs. the Consumer Price Index’s 89 percent rise. As one hospital CEO said, “You could be an idiot and make a fortune on Medicare reimbursement. Any mistake you made got reimbursed.”
- Hospitals didn’t worry about the introduction of Medicare DRGs in 1983 because those had a 14.5 percent profit margin built in and excluded capital expenditures, physician fees, and post-acute care services, all of which then started to rise.
- Patients with good insurance don’t care about cost because they aren’t paying, choosing instead based on convenience and amenities.
- Commercial insurers have cut into Blue Cross’s dominance by reducing costs, choosing providers based on quality, and introducing managed care that can exclude expensive providers from their network, require prior authorization for expensive procedures, and give doctors financial incentive to reduce the use of unnecessary services. That, along with the rise of ambulatory surgery centers, has slowed the arms race.
- Hospitals use local political influence, community pride, and vast employment to protect their interests and to have favorable legislation enacted that restricts referral of lucrative patients to lower-cost specialty hospitals that often deliver better outcomes.
- HMOs and heavy-handed employer cost-control efforts in the 1990s caused a consumer backlash that was fueled by lobbyists for hospitals and doctors, which triggered states to limit cost control practices.
- Mergers have left 67 percent of hospitals as members of larger systems and often the owners of many more physician practices, but instead of reducing excess capacity, the now-larger health systems are using their clout to increase prices further.
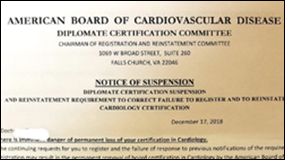

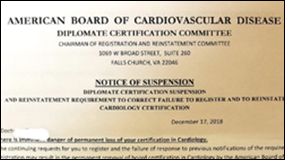
A doctor who received the above “notice” calls out the phony American Board of Cardiovascular Disease, which is hoping that inattentive medical office workers will send a renewal check to the Falls Church, VA edifice in which it conducts its scientific deliberations (photo above – it’s in the UPS Store, not the adjacent UBreak- IFix). It doesn’t even have a website. This would be hilarious if not for Googling, which reveals many cardiologist “diplomates” who actually advertise their fake credential. The Board’s executives apparently live communally in their tiny mailbox along with those of the equally bogus American Academy of Peripheral Vascular Disease, the American Council of Christian Physicians and Surgeons, the American Academy of Surgery, the American Board of Dental Surgery, the American Association of Ethical Physicians, the American Board of Oncology, National Diabetes Institute, and the American Board of Urogenital Gynecologic Surgery. Being a Diplomate in Internet-Primary Sleuthing in Heath IT myself (no acronym, please), I tracked down the apparent owner of all these organizations – Keith Lasko, MD, DDiv, who had his own medical license yanked by three states in 1990, after which he started all these organizations and several more like them as retribution (or perhaps correctly identifying an underserved market in fake credentials by those entrusted with the public’s health). The reverend-doctor lives on the spectacularly porn-worthy named Vivid Violet Avenue in Las Vegas, although a lawsuit I ran across suggests that his house is being foreclosed upon by “allied infidels” who want to “throw him and his children into the street as unclean dogs,” referring to his “Mosque of the Golden Rule” religious organization, where he has commendably attained the rank of Imram. He also wrote a poorly-received 1980 book titled “The Great Billion-Dollar Medical Swindle.” My conclusion – the “diplomates” are the bad guys here since there’s no way they believe their bogus credentials are real, so their only intention in buying them must be to mislead patients. The Imran is simply meeting the demand.

The Hustle interviews the original voice of Siri, voice-over actress Susan Bennett, paid an hourly rate in the summer of 2005 to read seemingly meaningless sentences such as “Militia Oy Hallucinate Buckram Okra Ooze ”for ScanSoft (later acquired by Nuance). She found out only after hearing Siri for the first time that those meaningless syllables – which she had to read precisely as measured by an audio analyzer strapped to her throat – were then chopped up into fragments that could be reassembled to make new words and sentences. Here’s a health IT connection – some of my favorite interviews are with NVoq CEO and speech recognition pioneer Charles Corfield (April 2014, July 2017), who was an early investor in Nuance acquisition BeVocal, widely rumored to have contributed the basics of mobile device speech recognition that became Siri. He’s always amused when I amateurishly try to pin him down on his Siri contribution, chuckling and intoning in his mellifluous British accent, “I think I shall refer you to Nuance to comment on matters of Siri or otherwise.” Corfield also created the precursor to Adobe FrameMaker, the first desktop publishing program, while working on his astrophysics PhD at Columbia after graduating from Cambridge. He’s one of the most interesting people I’ve ever talked to, a lock for my HISsies vote for “industry figure with whom you’d most like to have a few beers.”
Sponsor Updates

- The Nordic team continues its partnership with The River Food Pantry in Madison, WI.
- Lightbeam Health Solutions publishes a new white paper, “Data-Driven Solutions Providers and Payers Need for Value-Based Care Alignment.)
- MDlive publishes a case study featuring Cone Health (NC).
- EClinicalWorks publishes a podcast titled “How Interoperability Fine-tunes a Neurology Network.”
- Netsmart will exhibit at the North Carolina Providers Council Annual Conference January 14 in Greensboro, NC.
- OnPlan Health and Patientco will exhibit at the HFMA Western Region Symposium January 13-16 in Las Vegas.
- Experian Health and Change Healthcare partner to deliver identity management solutions.
- PatientKeeper will exhibit at the HFMA MA-RI Annual Revenue Cycle Conference January 17-18 in Foxborough, MA.
- TheFutureofThings.com includes PatientKeeper in its list of top healthcare apps.
- Huron announces 20 senior-level positions.
- ZeOmega publishes a new case study highlighting how Alliance Behavioral Health is using Jiva to manage care for North Carolinians experiencing mental health challenges, addiction issues, and intellectual disabilities.
Blog Posts

Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates. Send news or rumors.
Contact us.












![image[20] image[20]](https://histalk2.com/wp-content/uploads/2019/01/image20.png)






























I use a wiki and was exploring some of the extended character sets. I was startled to learn that the…