Readers Write: To Douse the Flames of Physician Burnout, Target the Four Biggest Time-Wasters in the EHR
To Douse the Flames of Physician Burnout, Target the Four Biggest Time-Wasters in the EHR
By David Butler, MD
David Butler, MD, is principal at Calyx Partners and interim CMIO at Guthrie Health in Sayre, PA.

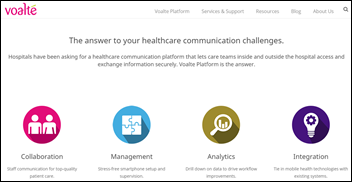
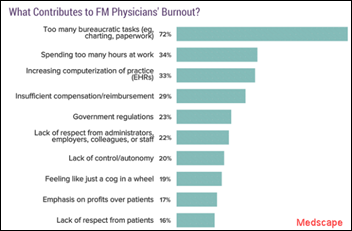
There’s no question that physician burnout is one of healthcare’s most pressing problems: Forty-four percent of physicians report feeling burned out. It affects everyone to varying degrees: specialties, employed vs. self-employed, men and women.
The Number 1 contributor? Too many bureaucratic tasks such as charting and paperwork. The bottom line, according to Mayo Clinic Proceedings, is that physicians who aren’t comfortable using EHRs are more likely to reduce their working hours or leave the profession altogether.
We all agree on the challenge, but what’s not as obvious is the solution. Many hospitals are investing in scribes and assistants like they’re a sustainable solution. Individual providers have stated they have higher satisfaction, but the evidence isn’t showing that this is always the case.
Other organizations are placing the burden on other docs, creating physician-led training teams to improve EHR efficiency in their facilities. This can provide some level of peer-to-peer efficiency when thoroughly implemented with the correct support staff, in-room support, and focused curriculum based on user specific metrics. Otherwise, instead of slowing one doc down, you’ve merely doubled your inefficiency.
Mindfulness, yoga, and other self-care strategies are problematic. They take time—of which physicians are already short – but more importantly as this recent whitepaper on burnout points out, they fail to address the root cause and put the responsibility of burnout on individual physicians.
We’re all responsible for burnout. In my experience as a CMIO and EHR implementation and optimization strategic advisor to various healthcare delivery systems, the key to reducing frustration with the EHR and physician burnout is practical tactics that actually give doctors time back in their day.
These are the four biggest time wasters in the EHR and how to address them.
1. Searching for Clinical Data
When you think about search in the consumer world, companies like Netflix and Amazon may come to mind. They use various degrees of artificial intelligence (AI) to serve up what you’re likely to be interested in based on your past searches to streamline what you see.
Unfortunately, EHR search isn’t quite that intuitive yet. Searching for clinical data will happen during every patient visit, making it one of the biggest EHR pain points for physicians. Until the leading vendors incorporate focused AI and machine learning, the average physician should use these tips to filter through the sea of patient data more easily:
- Default to search over navigation. I just described that EHR search is far from perfect. However, it is infinitely better than browsing and clicking your way through the interface. Sure, I know how to navigate to a WebEx site to join the meeting. Do I ever do that? No. Not when typing “Join WebEx Meeting” into Google gets me there much faster. Similarly, I always tell docs to search the chart. Let the system look for you by using the search bar. Once the page loads, typically Ctrl+F will open another more specific search box to find keywords within long patient reports of clinical data. Remember to use quotation marks around words that you want an exact match, i.e. “chest pain” versus just typing chest pain. Most EHRs will not suggest a correction like Google and ask, “Did you mean: chest pain” (correct spelling). So, learn your search tricks like: quotations, NOT, OR, AND, parentheses around multiple terms, etc.
- Save your filters. When you listen to music on your app of choice via your phone or in the car, in order to rapidly get to what you want to listen to, you still have to either download albums, bookmark your favorite playlists, and/or save your top radio stations as presets. If you’re looking for the same type of data over and over again, be certain to treat the EHR in the same manner by saving your most common searches as a filter in chart review (labs, notes, imaging, etc.). Treat the filters like playlists. Create a cardiac playlist for all lipids, cardiac enzymes, and any other labs that brings the patient’s cardiac status into full view for the way you practice medicine based on your specialty and training.
- Create disease- and symptom-specific reports. The majority of physicians in the U.S. are specialists and routinely need to zero in on the same disease, condition, or symptoms. Your EHR teams can easily create elegant patient summary reports that will pull data to you, i.e. all diabetes-related meds, labs, studies, referrals, etc. Most of the time you will have to agree on this with a group of clinicians within the same department, but roughly 20 percent are customizable at the individual level. Remember, just use newly created Maroon 5 “Sugar” playlist for the rest.
2. Managing the Inbox
Have a full Outlook inbox or an IMessage app with a permanent notification icon or badge? The EHR inbox is like that for physicians, but on steroids. InBasket is the name for the inbox for Epic users, but regardless of your EHR vendor, managing the flood of messages can be a struggle, and with greater interoperability, it will only get worse. Here’s what I tell physicians (and IT folks who want to help them) to personalize the InBasket to their workflow and get it under control:
- Rearrange and sort. Many docs don’t realize that there are filters and sort logic available to always keep their most critical messages at the top (for example, abnormal test results, patient calls, refills, etc.). Fight your OCD and move to the top only the folders that you need to address to get the heck out of the office: results, patient messages, billable chart co-signs, refills, etc. Deal with the rest later, as they likely are not important and are just automatically sent to you because they always have been.
- Remove and relocate buttons. Healthcare can take a lesson from the airline industry here. Just like in the cockpit, buttons and alerts should be presented in a logical, easy-to-read, color-coded format. Just like in other programs you use, such as Microsoft Office, you’re able to customize your user interface to increase your focus with no IT team required. Kick the clutter by deleting buttons that are never used and move ones that are frequently used to more convenient locations. Just look for any sort of wrench, bolt, pliers, or other icon on your screen, which typically means you can move things around.
- Maximize your view. Treat your EHR view like you would your physical office and Marie Kondo the heck out of it until it’s most comfortable for you. Adjust the preview panes, sidebar, and the even the order that the report displays in to see as much information as possible at one time. For example, you may have the top half of your screen display your messages and the bottom half display reports about the particular patient to save you time from going to chart review. Maybe the EHR won’t quite spark joy for you, but it will definitely be less painful.
- Create macros / QuickActions. I’ve encountered very few physicians who have created InBasket macros. These are simple, rote tasks / words / clicks that one does over and over based on a specific type of message. These are worth investing in as they offer significant time savings, a 60 to 70 percent time savings per message type for some. For example, you can create a macro that notifies a patient via the patient portal that (1) your labs were abnormal, yet not serious; (2) my office will contact you; (3) route to your nurse/team; (4) add a small note to yourself; and (5) close the lab message–all in ONE CLICK. Spend a few days watching for things that you do over and over, then try one. I suggest refill and normal result labs to start. They’ll give you hours back in your life over time.
3. Entering Orders
Does Amazon have order sets? Sure it does. When you order a new smart TV, it will automatically suggest the recommended HDMI cable, remote keyboard, etc. That’s an order set.
I’ve always wanted an Amazon-oid EHR. When I order the latest back pain (chief complaint) for my patient, I would like for the EHR to then make recommendations based on my patterns, my colleagues’ patterns, and other patients like this one. I’d like to see it display useful information that says something like “other internists like you who have seen patients with similar complaints have done X, Y, and Z.” I’m smart enough to know if I care to follow the pack or click and see what the latest evidence-based data is from the literature.
Until this occurs, here are a few tips you can use today.
- Save your faves. Not saving your favorite orders is like not using bookmarks for your favorite websites when browsing the internet … not cool! Similar to the above macros and filters, these are key to faster ordering common things. Record dosage tapers and save multiple preferences for the same med, lab, or imaging with pre-fills. These are common, especially with chronic diseases, so save yourself from typing it or searching for it an infinite number of times. Some techie docs may already have these saved and may be willing to share with you if you ask nicely. Meds: refills 0, 30, 90 day refills, narcotics. Labs: A1c in three months, A1c in six months, etc. Imaging: CXR – chest pain, CXR – pneumonia.
- Use portions of the name of the order. Google might say, “Did you mean?” when your search isn’t perfect, but the EHR won’t. However, you can use shorthand to look up med, lab, or imaging orders. For example, here’s an Epic trick that’s been around for at least 10 years that many don’t know. When searching for an order or diagnosis, try typing small pieces of the word (in any order), i.e. “CT Abd Con” will return a short list of “CT of Abdomen and Pelvis with Contrast.” Just remember, when it comes to searching for orders in the EHR, less is more! Check with your training team for more tips.
4. Documenting the Encounter
Physicians likely spend the most time here, inputting all of their notes into the EHR. Documentation takes a lot of time, whether it’s documenting visits, sending thank-you notes for referrals, or fielding follow-up questions in the patient portal. If you have to type, then create templates for things you say over and over. There’s no predictive text a la Gmail yet, but we can emulate it until we’re there.
- Leverage SmartText and SmartPhrase templates. These are Epic system-specific names for their tools, but all EHRs I’ve used have the same type of documentation tool. Again, it’s all about making the EHR work for YOU.
- Speak now. In the age of Siri and Alexa, it’s simply bewildering how many physicians don’t leverage speech recognition software like Nuance Dragon or MModal. Add in voice navigation macros and you can rattle off your notes to your computer with incredible speed and accuracy. For example, “Show me last CBC,” or “order amoxicillin 500.” etc. And be concise! Despite what we learned in med school, verbosity doesn’t mean better care.
- Create SmartLinks. One of my favorite tricks to teach is how to pull data into your note for review, then delete (Ctrl+Z is undo). Don’t type values—learn tricks to pull into your note when appropriate (without pulling in too much in creating note bloat). As you look at others‘ notes, you’ll notice that they are pulling these labs, etc. into their note. Just find out from them how they are doing it, get the link, then you do the same yet with no need to leave it in the note. This is faster than search or filters.
Those four areas of the EHR compose about 80 percent of “pajama time.” Anything that you can do in one of those areas that can shave off a little time, you’ll see time come back in the long run—it adds up over many patient visits. Until the EHR vendors incorporate the functionality from consumer technology noted in the above examples, you must do these things to survive and stay optimistic.
By targeting these areas with these tried and true tips and tricks, I guarantee you’ll feel like you have more control over something that once felt like it was uncontrollable. Keep these fire extinguishers handy and you’ll douse some of the flames of burnout and take back your time.



































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…