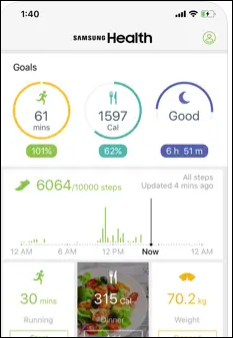
There’s always a lot of buzz around wearables. The majority of US adults have a smartphone in their pocket or purse, so a treasure trove of data can be collected without adding a secondary device.
Most of the people I talk to have no idea how much information is being captured by the apps on their phones, let alone the types of entities to which vendors are selling their personal data. Nearly everyone I know leaves their location services on 24×7. About half the people I interact with, along with their families, use tracking apps to keep up with each other’s location.
An article in JAMA Network Open this week caught my eye with its title, “Passive Smartphone Sensors for Detecting Psychopathology.” The authors analyzed two weeks of smartphone data from 550 adult users see if “passively-sensed behavior” could identify particular psychopathology domains. They noted that this is important work because smartphones can continuously detect behavioral data in a relatively unobtrusive way.
They had two main objectives. First, to determine which domains of psychopathology can be identified using smartphone sensors. Second, to look for markers for general impairment and specific transdiagnostic dimensions such as internalizing, detachment, disinhibition, antagonism, and thought disorder.
Data were pulled from global positioning systems, accelerometers, motion detection, battery status, call logs, and whether the screen was on or off.
The authors were able to link nearly all the domains with specific sensor-captured behaviors, creating “behavioral signatures” by measuring things like call volume, mobility, bedtime, and time at home. Specifically, they were able to link disinhibition with battery charge level and antagonism with call volume.
Based on the phone-related behaviors I observe, it would be interesting to see if my gut feeling about a user’s psychopathologic situation is accurate. I would also be curious to know if there is a difference in the data looking at other age groups that weren’t studied, such as teens or the elderly. Although the study was done on adults, the mean age was 38 with a standard deviation of 8.8, so there is certainly some opportunity to look in detail at other groups.
I was recently with a large group of individuals in their 70s. Their visible phone behavior would rank them right up there with the teenagers I know.
Reading about this made me think about all the data that companies are collecting now that they’re focusing on potentially eliminating remote work and ensuring high levels of productivity. There are plenty of stories out there about people using so-called “mouse jigglers” to make it look like they’re working so that their computers don’t go to sleep. Of course, companies that restrict what kinds of USB devices can be plugged in might be attuned to that, and there are also more sophisticated monitoring tools that also look at keyboard usage patterns and can detect if something shady is going on.
Remote work isn’t the only place people might be slacking off. I see plenty of people who have in-person jobs who constantly use their phones for potentially non-work activities. Many apps might be adjunctive to job role and responsibilities, but I see a lot of online shopping and social media use as well.
I’d love to see some robust research that looks at communication and collaboration strategies within an organization to see which workers might thrive with one style more than another. I’ve worked in organizations that have documented communication plans that make it clear what kinds of work should be conducted using meetings, phone calls, email, instant messaging, and texting, but those kinds of policies are few and far between these days.
Even without a written policy, workplace culture defines how things get done, but when you’re a new person, a consultant, or a contractor, it can be difficult to try to figure that out unless someone clearly explains the rules of engagement.
I worked in one organization that basically used Slack as the connective tissue of the organization. I have to admit that I struggled there. Every time I asked where to find a resource, the answer was, “It’s in Slack,” but it didn’t seem like there was any rhyme or reason to how things were organized. More often than not, important documents were accessed through links within a message thread rather than being in a “files” area or in specific channels that made sense to those of us who were new.
A tremendous amount of work seemed to get done via direct messages rather than channels, making it even more difficult to find things. At one point, during a critical issue with a release, I had a separate cheat sheet of which conversations to look through when I needed certain kinds of information, since I had an endless list of direct message conversations with various combinations of the same group of people.
When I asked if there was any team- or company-level documentation on how it was all supposed to work, I felt like I was revealing myself as someone who simply couldn’t keep up. As a consultant, I had multiple conversations with leaders at the company about how this was working and how I had seen it contribute to process defect rates and rework. I also knew of plenty of examples at that company where people downloaded documents to their own hard drives so they could find things later, but who then ended up working off of outdated specifications since they were using local copies rather than shared ones. Not to mention that if people can’t find clear information, they are more likely to improvise or otherwise wing it, which is generally a bad idea when you’re building healthcare software.
If you could use data to find scenarios where someone was working on a deliverable – say, a slide deck or a document — and then spent 10 minutes rapidly flicking through various file structures or messaging platforms, opening and closing multiple documents, and doing web searches before finally returning to the document, it could be an indicator of disordered work patterns that might benefit from some kind of intervention.
If you see multiple people on a team with these work habits, that may be indicative of the need for a different kind of organizational structure for work product and other materials. I think those patterns are much more important to explore than knowing whether someone’s mouse is moving
What do you think about looking at smartphone or other device data to learn more about people’s behavior and the potential for psychopathology? Would having more information make things better or potentially make things worse? Leave a comment or email me.

Email Dr. Jayne.
























Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…