Blake Walker is co-founder and CEO of Inbox Health.

Tell me about yourself and the company.
Inbox Health is a software platform that fully automates patient billing, payment collection, and patient support for medical practices and billing companies. We try to make bills clear, help them get to patients faster, and make them more convenient and affordable for patients to pay. Alongside that, and an important part of that process, is to make sure that patients get fast and empathetic support via phone, text, and real-time chat to get their questions about their bills answered while we’re doing that.
I started in the healthcare space right out of college. I worked on a patient financing startup and quickly learned how problematic the patient AR problem was becoming for medical practices, especially smaller medical practices. I then spent a couple of years working on another patient billing startup and then ultimately founded Inbox Health 11 years ago. I have been with the company ever since, growing it from zero to where it is today, with about 3,500 medical practices using the platform nationwide.
How does the patient’s payment experience influence their satisfaction with the provider?
It’s a huge factor. It’s so intertwined today, the way the clinical experience then carries over into the billing experience. The patient can leave that visit feeling good about the clinical care, but then have such a bad billing experience that their entire perception of that provider is dragged down.
If there are mistakes in the way their insurance was billed, the provider may end up getting into an argument with them on the phone after the fact. Or even worse, it’s not even the provider, it’s the provider’s billing service provider. The patient may feel that the clinician provided a worse clinical experience because of how the billing went.
Having a great billing experience is critical to making sure that the entire clinical visit is perceived as positive. So much more frequently than ever, that billing experience is a negative one. Patients owe more money. High-deductible health plans are common now, and patients are surprised by the bills they get and are frustrated by them.
As providers, we owe it to the patients to do everything we possibly can to make sure that the billing is done accurately and clearly and that the experience that they have is convenient. Often it’s paper checks only and poor patient support to answer their questions. That will obviously leave the patient with a bad outcome.
How do practices prevent those awkward financial moments that can start or finish a visit, especially when the practice may not know what services the patient will need ahead of time?
Educating the patient about their coverage at the time of the visit, and how that visit is likely to be billed to the patient, is an important starting point. You don’t necessarily need to have it down to the dollar, just that the patient understands that a bill is likely. If they come in to a nutritionist’s office, their child is sick, and you see that they have a high-deductible plan, give them a sense of expectations, such as that it usually takes about two weeks for us to send bills out. Or after your insurance is adjudicated and we know that you’re on a high-deductible plan, I want to make sure to flag that for you. That’s realistic for most practices with just their standard processes for eligibility checks prior to visit and understanding a little bit about the patient’s insurance. The patient can fill in the rest.
Then, whatever you can do to get the bill to the patient as quickly as possible. You don’t want situations where it’s months and then the patient’s getting a bill 90 or 120 days after they came in to see you. I understand that there’s often trouble getting it through the adjudication process with insurance, but getting that timeline as fast as possible so that the patient is in that same frame of mind as when they came in to see the clinician in the first place. Having that be an easy, convenient digital-native experience as much as possible helps to streamline that whole experience.
How does the method and timing of presenting the bill to the patient affect getting paid?
Most patients want to have both the digital presentment and also the tactile patient statement in the mailbox to know that it’s legitimate. Sending a text message or an email captures their attention, but it doesn’t feel real to them. Once they get the statement in the mail, then it feels more real and they are more likely to pay from the email or text that follows up after the statement. It’s a combination of demographics and who’s more likely to pay from email or text message than a paper statement. But for most patients, email is the most likely way to drive payment.
No method on its own works particularly well. Everyone pays attention to text messages, but are hesitant to click on them and pay because texts are often used for scams. It has to be a holistic approach, where at least in our case, we’re using artificial intelligence to identify what will probably work best for most patients. It’s all dynamic. It has to be an omni-channel, holistic approach to trying to reach the patient in the way that will work best for them and meeting them where they are at any particular time through a process over several weeks and sometimes months.
How common is it for the patient to need or want to contact someone at the practice once they’ve received a bill?
About a quarter of the bills that go out create a question. That’s obviously a huge factor in terms of how you’re running a practice now. If you’re sending these bills out without anticipating and being prepared to answer those questions, it’s going to pull down your collection rates. It’s going to negatively impact the consumer experience with those bills. Most of us aren’t well prepared to do it, but it’s a high proportion that are coming back to the practice with questions.
A big factor is the amount of money owed. The average family has a $4,000 deductible and it’s not uncommon to end up with a $500 or $600 bill from a standard medical visit. That’s a huge number for most families. You shouldn’t expect that someone who gets a $500 or $600 bill will just blindly pay it from all of this wording that’s on the bill, and why it was billed that way. It’s unlikely that someone will just pay without asking a question.
What is the outcome of those billing calls to the practice? Are patients looking for reassurance that the number is correct or perhaps wanting more details that could have been provided on the bill initially?
I would say that about half could have been addressed upfront. Better setting expectations, providing better information on the bill itself, is often a root cause of the questions that come through. But a significant number of them are related to how the billing was done. It’s often somehow related to coordination of benefits, meaning what insurance was billed and in what order was it billed, particularly for patients who have multiple insurances like Medicare or Medicare Advantage plans or multiple commercial plans. A lot of those cases have legitimate issues that feed back to it, and ultimately, that could be prevented to some degree upstream just by collecting better information at the front desk.
I’m just isolating the patient billing itself. It’s a little difficult to control what problems land on the lap of your patient support team because something wasn’t done well up front.
How often does the patient get frustrated by trying to coordinate the practice’s billing, the insurance payment, and their own financial responsibility?
It’s frustrating for everyone. The provider obviously wants the procedures to be covered to whatever extent they possibly could be. The patient is stuck in this loop where they’re asking the provider questions, the providers are deferring to the payer, and the payer defers to the provider. All sides don’t have a full picture.
The patient is the one who’s left holding the bag with a bill that someone is demanding to be paid and the frustration of two parties that aren’t seeing eye to eye. It’s common for the provider’s answer to be “ask your payer” and for the payer’s answer to be “ask your provider.” The patient may finally give up and pay the bill or ignore it and see what happens. Patients are seeking that alternative more and more.
What are some best practices for reducing how long it takes to receive payment for patient responsibility?
Optimizing the number of touch points and the channels that you are able to reach a patient on in that first 15 days is critical. That’s the first thing.
Second is meeting patients, from an affordability perspective, where they are. Understanding where a patient’s threshold is for when they might need payment plan options and making those payment plans available to a patient readily. You don’t want the patient waiting 45 or 60 days, getting three bills from you, and then picking calling you and saying, “I know you keep asking, but I don’t have $1,500. I just don’t.” Then you tell them that you can take $50 a month and that’s fine. You need to be proactive about how you engage the patient, which channels you engage them on, and then offering the payment plans when it’s applicable to that particular patient.
We do predicted payment plan offers, where we’re looking at various data points about a patient, their bill, and their past history with the practice and then determining which ones to offer payment plans to and what kind to offer.
But if you can do those two things well, that will get you the best possible result. Some of this comes back to the more that you do at the front desk to educate the patient and collect cards on the file, the more you can accelerate that back end as well. But if you can’t influence that or change that for whatever reason, then obviously on the back side, that approach makes the most sense.
How are you using AI now and how will you use it in the next year or two?
AI has always played a role in how we manage the outgoing patient billing process. The biggest changes in how we’re using AI, and how AI will be used in the patient experience moving forward as it relates to patient billing, is on patient support. We are investing heavily in making the patient support experience better by training large language models to answer the patient questions that come back, feeding it data from the patient record to be able to help it answer patient questions, and letting it actually take action, such as the patient didn’t get a paper bill and wants one, so AI sends it. Or creating a payment plan.
Over the next two to three years, you will see a transformational change in how patient phone calls are answered and how patient chats are answered relative to where we were a couple of years ago, or a year ago. Or even right now, where most of that is either going to the practice staff in the office or it’s being outsourced to the Philippines or India to lower-cost resources. The quality of AI for patient support is rapidly improving and will play a cool role in improving the patient experience in many ways, but in particular, around patient billing.
What factors will drive the company’s strategy over the next three or four years?
Investing heavily in the role of artificial intelligence in the patient experience is a main focus for us over the next few years. And in general, partnering as closely as we can with the best-in-class EHRs and practice management systems to make the experience as seamless as possible for patients where their providers are using different EHR platforms is really important to us. Those are the areas we’re investing heavily in. We believe there’s a lot of opportunity to improve the front desk experience. That’s another area where we’re focused on trying to build technology to improve how the front desk experience connects back to the patient billing experience post-visit.
Comments Off on HIStalk Interviews Blake Walker, CEO, Inbox Health


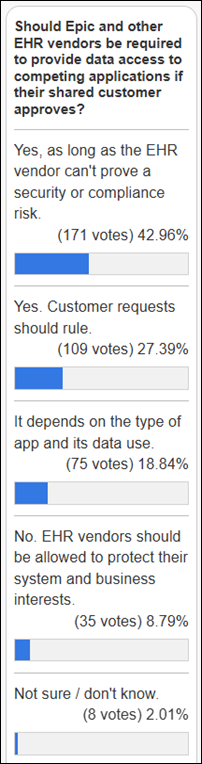

























That, or we see if Judy will announce Epic's new Aviation module (probably called Kitty Hawk) that has integrated Cruise…