News 1/30/26
Top News
Sword Health acquires Germany-based digital MSK and pulmonary care company Kaia Health for $285 million. Sword will sunset Kaia’s MSK product in the US in favor of its own platform.
Sword plans to raise $500 million in Q1 for expansion and acquisitions.
HIStalk Announcements and Requests
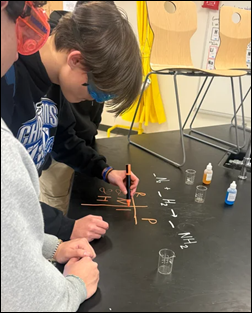
Reader donations funded the Donors Choose teacher grant request of Mr. S, who teaches high school in Greenwood, DE and asked for help buying chemistry lab supplies and learning tools. He reports, “My students and I were able to experience chemical reactions like never before with a hands on approach rather than watch a video of someone on the internet … This experience allowed me to see the spark for learning that my classroom has been missing. By me engaging the students in the classroom this one time might create the next great chemist or inventor, and for that I cannot thank you enough.”
Amazon will lay off 16,000 employees while “reducing layers, increasing ownership, and removing bureaucracy,” which translates to firing rank-and-filers because of an org chart that executives built, tolerated, and now blame. How about starting with the belatedly enlightened suits who created those layers and bureaucracy in the first place? Our industry is littered with “Now we get it” announcements in which so-called rightsizing that somehow always spares the people who did the wrongsizing. Pro tip: ignore anyone quoted in statements like these who has been with the company for two or more years and thus helped create the mess that we are now supposed to believe they have magically fixed by jettisoning worker bees. It is a useful reminder that feel-good Kumbaya capitalism about being a family and valuing associates is performative BS that is touted when times are good and then dumped emotionlessly when knee-jerk cost cutting is required to line the pockets of investors and executives.
Sponsored Events and Resources
Live Webinar: February 18 (Wednesday) 2 ET. “From Blind Spots to Insights: Gaining Real-Time Visibility into Healthcare Risk.” Sponsor: CloudWave. Presenters: Jacob Wheeler, MBA, director of sales engineering, CloudWave; Mike Donahue, chief operating officer, CloudWave. Resilience starts with the ability to see clearly, across every endpoint, cloud workload, user, and clinical system. Join CloudWave’s cybersecurity leaders for an in-depth session on how real-time visibility transforms your ability to detect threats early, respond decisively, and strengthen resilience across the care ecosystem. Attendees will learn the practical steps that hospitals can take to move from reactive defense to resilient action.
Publication: HIStalk’s Guide to ViVE 2026 lists the activities of sponsors at the conference.
Contact Lorre to have your resource listed.
Acquisitions, Funding, Business, and Stock
Virtual OCD provider NOCD acquires trauma self-help platform vendor Rebound Health and renames itself to Noto.
Premise Health and Crossover Health, which offer primary care and occupational health services, will merge. Crossover was co-founded in 2010 by ED physician Scott Shreeve, MD, who had co-founded Medsphere and will remain with the merged organization.
An investment firm speculates that Oracle may undertake mass layoffs and sell its Oracle Health business unit to fund the $156 billion in capital that it needs to build data centers for OpenAi.
People

Woman’s Hospital hires Glynis Cowart, MPA (Montefiore St. Luke’s Cornwall) as SVP/CIO.

CloudWave promotes Brian Pruitt to CTO.



Clearwater announces the hiring of Davis Chaffin, MBA (Load One) as CFO and Krissy Safi, MBA (Protiviti) as SVP of consulting services, and the promotion of Dave Bailey, MBA to VP of consulting solutions and strategy.

Meditech founder, chairman, and former CEO Neil Pappalardo died Tuesday. He was 83. Pappalardo and four MIT-educated co-founders launched Meditech in 1969 to create hospital software using the MUMPS program language that he and fellow founder Curt Marble developed at Massachusetts General Hospital.
Announcements and Implementations
Humana’s healthcare services business CenterWell goes live on Athenahealth’s AthenaOne at 350 senior primary care locations in 15 states.
Virtual primary care and healthcare navigation company Included Health creates a health plan and provider network that it will offer to employers.
AEYE Health, which offers fully autonomous AI-based diabetic eye exams, integrates its product with Epic.
EMurmur earns FDA clearance for its telehealth-capable heart murmur detection software for digital stethoscopes. Companies can integrate the technology with their own software and hardware without requiring additional FDA clearance.
A UK study reports that use of Eko’s AI stethoscope failed to improve detection of heart failure, atrial fibrillation, or valvular heart disease in primary care as adoption fell steadily, with 40% of practices dropping it within a year despite its effectiveness because of workflow friction that was driven by poor EHR integration. The AI stethoscopes whose use physicians resisted increased detection of heart failure by 2.3 times, atrial fibrillation 3.5 times, and VHD 1.9 times.
Government and Politics
The VA will spend $1 billion in FY2026 to maintain its EHRs and to prepare for implementing Oracle Health in new facilities.
ASTP/ONC posts an RFI that seeks public input on accessing and exchanging diagnostic images to inform possible rulemaking.
Privacy and Security

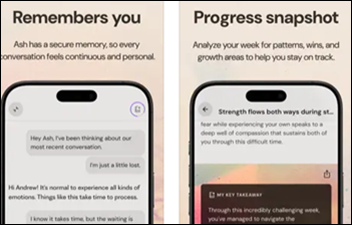
DataBreaches.net reports that “digital helper” AI care coordination vendor Lena Health stored audio recordings that contain patient information, most of it from Houston Methodist, on unsecured web servers. A security group that is working with law firms to coordinate a class action lawsuit summarizes:
Listening to these confused patients talking to Lena, this company’s “digital helper,” about their private medical issues is a deeply disturbing and uncanny experience. They repeatedly ask Lena what’s wrong with her, why she sounds so weird, but even worse somehow are the patients who do not seem to notice they are not speaking with a human. It is deeply dehumanizing, and profoundly depressing to hear these elderly people … discussing their most personal medical issues with what they think is a compassionate human coordinator, but is actually an LLM trained to extract information so a hospital can save a few pennies on hiring a real human.
Sponsor Updates
- Altera Digital Health announces GA of Sunrise Medical Photography documentation tools, powered by True-See, within its Sunrise platform.
- Clearwater names Davis Chaffin (Load One) CFO.
- WellSky announces new AI-powered referral management workflows aimed at helping home health and hospice providers.
- Findhelp welcomes new partners Colorado Access and Wauwatosa Neighborhood Association Council.
- Healthcare Growth Partners releases its “January 2026 Health IT Market Review.”
- Health Data Movers releases a new episode of its “Quick HITs” podcast featuring Scott Becker.
- Healthmonix’s MIPSpro and ACO Impact receive 2026 CMS Qualified Registry approval.
- Meditech offers a new customer success story titled “Palo Pinto General Hospital Increases Google Reviews, Reduces No-Shows With Expanse Patient Connect.”
- Judi Health releases a new episode of “The Astonishing Healthcare Podcast” titled “A Quick Government Programs Update: The IRA & MPPP, Managing D-SNPs, and More, with Jason Barretto.”
Blog Posts
- The Smarter, Faster Way to Bring Clinical Intelligence to Life (Medicomp Systems)
- Performance to empower confidence: Why responsive technology makes all the difference (Altera Digital Health)
- Impact and challenges of large language models in healthcare (Arcadia)
- Begin Your NextGen AWS Migration Early With MTS (Med Tech Solutions)
- 2026 Healthcare & Health IT Predictions (First Databank)
- How Midsize Healthcare Orgs. Are Cutting Costs with AI-Powered RCM Solutions (FinThrive)
- Healthcare Data Privacy: What Industry Signals Reveal About Deeper Cybersecurity Risk (Fortified Health Security)
- OBBBA Compliance: What Healthcare Providers Need to Know About Qualified Overtime Reporting (Healthcare IT Leaders)
- The CEO Playbook: Medical Group Growth in a Hyper-Competitive Environment (Impact Advisors)
- Are you still charting like it’s 2010? What’s changed with ambient AI (Navina)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Follow on X, Bluesky, and LinkedIn.
Sponsorship information.
Contact us.






























There was a time when my company went through multiple rebrands. These were relatively minor shifts, but completely unnecessary. It…