Monday Morning Update 9/29/25
Top News

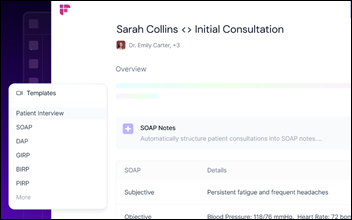
KLAS interviews 35 Epic customers at UGM following the company’s AI announcements. Most said that Epic’s move into ambient speech was expected.
Customers generally expect Epic’s product to be cheaper and better integrated than those of competitors.
Some respondents worry that Epic’s expanding footprint will stifle competition and innovation, although more than half expect to implement Epic’s ambient speech offering within two years.
Reader Comments
From Skeptical CIO: “Re: Epic’s ambient speech. Everyone assumes it will be cheaper than Nuance or Abridge, but Epic add-ons haven’t exactly reduced overall costs. The Epic tax keeps going up while reducing competitor innovation. I don’t buy the argument that Epic will run this as a loss leader.”
From Grizzled Analyst: “Re: federal telehealth coverage. Ending with a shutdown and turning off a decade of progress with the stroke of a Congressional pen. Hospitals spent millions on virtual care platforms, patients got used to access, and now it’s all at risk because of political brinkmanship.”
HIStalk Announcements and Requests

Most poll respondents don’t expect personal financial improvement next year, with federal government volatility most often cited as the cause.
New poll to your right or here: Would you change doctors over non-clinical problems such as staff behavior, billing errors, bad tech, or scheduling headaches? It probably depends on how much you rely on continuity of care, whether you perceive your physician as better than the alternatives, or who takes your insurance. Medical practices are odd that much of the management and public-facing behavior is left to unqualified or unmotivated employees because doctors are poor managers.
Pondering:
- Would outcomes differ if health system C-level executives, especially those who are going all-in on AI, were themselves replaced by AI that was trained on hospital data? That might be even more relevant to for-profit company C-level folks, who seem to misfire often enough that maybe AI can’t do worse while saving huge annual salaries.
- With the raft of upcoming MyChart enhancements, should it work like Uber where doctors and patients rate each other for future consideration in booking appointments?
- Were you really “promoted” if your new job is higher on the org chart but comes with no increase in pay? I admit that I accepted an offer like that once, and would do so again, because (a) the office view was killer; and (b) the alternative was to hope they didn’t hire an insufferable idiot as my new boss. The health system claimed that they couldn’t afford to pay me more, which wasn’t the strongest argument since I had IT access to its salaries and financials.
Listening: The Favors, a collaboration between apparently popular (judging from Spotify stream counts) Finneas O’Connell (“Finneas,” a 10-time Grammy winner and Billie Eilish’s brother and collaborator) and Ashley Willson (“Ashe”). They wrote all the songs on their new release. It’s not usually my kind of genre, but I’ve played the album several times and can’t get enough. My painfully obvious prediction is that they will soon approach household name status, probably both individually and collectively.
Meanwhile, I’m cooling on podcasts just as quickly as I embraced them. I tried all the reader suggestions, but endless commercials are so jarring and distracting that I can’t focus on the story.
Sponsored Events and Resources
Survey: “What’s your take on the value of IT Managed Services?” Sponsor: CTG. Due to recent legislative changes, Healthcare organizations are under growing pressure to balance cost, performance, and innovation. CTG wants to hear from leaders like you on how IT managed services can help — or hinder — those goals in this quick, 5-minute survey. Your insights will help inform industry understanding and provide a clear picture of how IT managed services is currently being used.
Contact Lorre to have your resource listed.
Acquisitions, Funding, Business, and Stock
Veradigm will provide a business update after Tuesday’s market close, raising speculation that it will make an announcement about Nasdaq relisting.
Bonsai Health, whose AI agents automate the front-office workflows of medical practices, raises $7 million in seed funding. Founders Travis Schneider and Luke Kervin have launched three previous companies together, most recently PatientPop, which merged with Kareo in late 2021 to form Tebra.
People

Randall Sanborn, MS (MyMichigan Health) joins Aspirus Health as VP of system IT process and emerging technologies.
Announcements and Implementations
A Black Book Research poll of physician practice managers finds rapid growth in digital tool use and stronger EHR/RCM vendor ties, but half worry that collections will drop with medical debt removed from credit reports, while 81% don’t trust their system’s AI prompts due to lack of transparency and auditability. The report notes that practice managers often don’t recognize or use the capabilities of their current systems.
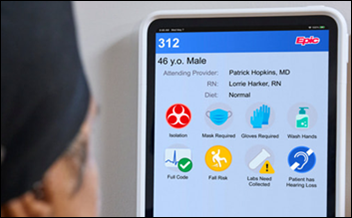
A sponsored 9to5 Mac article highlights 100-bed Emory Hallandale Hospital’s deployment of Macs, IPads, IPhones, and Apple Watches that run Epic Hyperspace, including its native MacOS app.
A Canadian news network warns patients that Epic MyChart’s new user agreement requires arbitration and a class action waiver, though such clauses aren’t enforceable under the consumer protection laws of some provinces. It also notes that patients can instead use hospital-specific web version of MyChart, which doesn’t include those terms.
Yale School of Medicine researchers validate that consumer prices increase when hospitals acquire medical practices. Interesting facts:
- States do not enforce antitrust laws.
- Healthcare quality doesn’t usually improve post-acquisition because “doctors are rather good at providing care across corporate boundaries” due to experience navigating insurance and referrals.
- Hospitals aren’t required to report practice acquisitions to regulators, so the authors had to develop an AI algorithm that probed available records to find doctors who changed employment from private practices to hospitals.
- Prices go up because hospitals press employed doctors to keep referrals in-house, insurers are reluctant to remove practices from their networks when that would mean removing the hospital as well, and consolidation increases market power.
Government and Politics
Politico reports that a looming federal shutdown, which can be avoided only if Congress passes a funding bill by Tuesday night, would end Medicare’s coverage of telehealth visits this week.
The UK government creates a National Commission on the Regulation of AI in Healthcare, which will accelerate NHS adoption of AI by advising on regulation and reviewing technology such as ambient voice that falls into a regulatory gray area. The group’s chair is University of Birmingham medical professor Alastair Denniston, MBBChir, MA, PhD.
Other

My favorite headline of the week calls Oprah an influential “woo-woo wellness” aficionado, only lightly mentioning that she gave our Medicare leader an early, scrub-wearing medutainment platform to peddle miracle cures and fad diets.
Sponsor Updates

- PerfectServe sponsors the American Heart Association’s Greater Washington Golf Tournament.
- RLDatix launches its new Hello from RLD campaign, reintroducing the company in the wake of its major transformations over the last few years.
- Arcadia, MRO, Healthmonix, and Navina will exhibit at the NAACOS Fall 2025 Conference October 8-10 in Washington, DC.
- Redox releases a new episode of its “Shut the backdoor” podcast titled “The Link Between Disney Imagineering and Healthcare Security Teams – Making the Impossible Possible with guest Bob Weis.”
- Waystar will exhibit at the KPCA Annual Conference October 1-3 in Covington, KY.
Blog Posts
- How Kern Medical Closed a $963K Gap and Gained $3M in 60 Days (Inovalon)
- Prioritizing Mental Health: 67% of Medical Groups Have a Behavioral Health Specialist on Staff (AdvancedMD)
- Reimagine trust for today’s healthcare with UpToDate Expert AI (Wolters Kluwer Health)
- How Autonomous Coding Keeps Pace with AMA/CMS and Simplifies Update Season (Nym)
- Demystifying Healthcare Payments: Complexity, Change, and What’s Next (TrustCommerce a Sphere company)
- And the 2025 Surescripts White Coat Award Winners Are… (Surescripts)
- Confronting the Crisis of Workplace Violence in Healthcare (Symplr)
- 4 Key Takeaways From Meditech Live 2025 (Tegria)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Follow on X, Bluesky, and LinkedIn.
Sponsorship information.
Contact us.





































Today's post contains the phoenixes rising from the ashes of the post COVID telehealth era. There's two things that destroy…