News 8/12/22
Top News

Cerner will pay $1.9 million in back pay and interest to 1,870 job applicants after the Department of Labor compliance evaluation found that the company had discriminated against Asian and black job seekers.
The affected applicants were seeking employment as medical billing specialists, system engineers, software interns, and technical solution analysts at the company’s Kansas City, MO and Kansas City, KS offices.
The review found that Cerner violated an executive order that prohibits federal contractors from discriminating in employment based on race, color, religion, sex, sexual orientation, gender identity, and national origin.
Reader Comments
From Outsider Trading: “Re: Change Healthcare’s ClaimsXten. The rumored acquisition by Availity this spring didn’t end up happening – TPG signed a definitive agreement to acquire it if UnitedHealth Group’s acquisition of Change Healthcare is approved by the federal government.” The initial media reports named Availity as the buyer of the payment integrity business, but TPG Capital signed a deal in April to buy it or $2.2 billion in cash, contingent on the UHG-Change merger being cleared by regulators. I removed that mention from Tuesday’s news post about Availity acquiring Diameter Health.
HIStalk Announcements and Requests
Welcome to new HIStalk Gold Sponsor Direct Recruiters, Inc. The Solon, OH-based company has been recognized since 1983 as the relationship-focused search firm specializing in building customized employment solutions. Our Healthcare IT and Digital Health teams partner with clients to help them strategically build high-performing teams from the C-Suite through the contributor level across each area of the organization. DRI offers contingency search, contract staffing and retained “Direct Retention” search to source, identify, acquire, and retain top-performing professionals to elevate the success of our client organizations. Recognized for over 17 national awards, DRI has a proven record of success in recruiting top talent for leading companies. Thanks to Direct Recruiters, Inc. for supporting HIStalk.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Virtual care and digital medicine vendor Biofourmis adds additional funding from Intel that increases its Series D round to $320 million.
Bloomberg reports that CVS offered $18 per share to acquire One Medical months before Amazon bought the primary care chain for the same price. The detailed timeline laid out in SEC filings is fascinating — CVS is reportedly Party A in the document.
TikTok’s parent company, China-based ByteDance, buys women and children’s hospital chain Amcare Healthcare for a reported $1.5 billion.
People

Tower Health (PA) promotes CIO Michelle Trupp, RN, MSN to SVP and COO of Reading Hospital.

Motient hires Brian Miller, MBA (Signify Health) as VP of business development.

Digital Diagnostics hires Chris Meenan (Philips) as CTO.
Announcements and Implementations
A study finds that patients who tested positive for COVID-19 and used Get Well’s remote patient monitoring technology to track their symptoms and vital signs had a 32% lower hospitalization rate, stays that were 2.7 days shorter, and fewer ICU days
Global Healthcare Exchange (GHX) Lumere launches a consulting service to help hospitals with their cost-saving and clinical variation programs. GHX acquired Lumere, which helped health systems align their drug and device purchasing decisions with evidence, in January 2020.
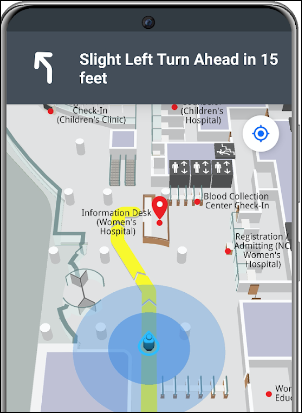
UNC Health and partners Gozio Health and Well Health enhance the health systems mobile platform to include a map of closest urgent care centers and EDs, a link to download the UNC Health app directly from text-based appointment reminders, and the option to save appointments to the mobile device’s calendar with a link to way-finding instructions. I noticed that the app also allows visitors to save their parking location so the app can route them back to their cars.
Government and Politics
The VA publishes a Digital Healthcare Playbook that describes how it works with contractors to develop software and lays out the kinds of solutions it needs.
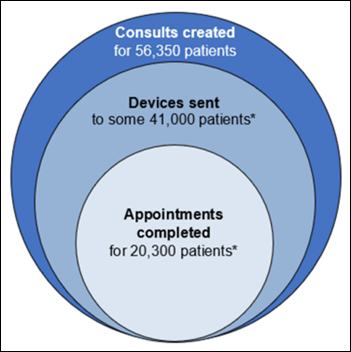
VA OIG finds that the VA loaned IPads to 41,000 patients last year for use in virtual appointments, but only half of them completed an appointment. The VA also failed to collect 11,000 devices that had never been used for virtual appointments, which cost $6.3 million for devices and another $78,000 in cellular data fees.
Connecticut spent $20 million of mostly federal money to fund a University of Connecticut project to build HIE software that was ultimately discarded in favor of buying a system from Maryland’s CRISP HIE for $1 million per year. The group that developed the system, UConn Analytics and Information Management Solutions, has shut down and dismissed its 20 employees.
The Defense Health Agency’s Military Health System awards a subsidiary of government contractor Peraton a 10-year, $2 billion contract for digital transformation services.
Sponsor Updates

- CoverMyMeds staff raise funds for cancer research organization Pelotonia during its annual live and silent auction, and by participating in Pelotonia’s ride weekend.
- Biofourmis appoints former Trevor Fetter (The Hartford) and Sachin Jain, MD (Scan Group) to its board.
- EClinicalWorks releases a new podcast, “How Payer Data in Healow Insights Can Help Improve Care.”
- CloudWave reports that over 50 of its customers have been with the company for five years or more, and that 92 have been customers for three years or longer.
- The Veterans Data Integration and Federation Enterprise Platform, which leverages technologies from InterSystems, receives the 2022 FedHealthIT Innovation Award.
- Lyniate launches version 11.2 of its Lyniate EMPI by NextGate.
- NTT Data announces the winners of the NTT Data AI Hackathon for innovations in healthcare.
Blog Posts
- Optimum CareerPath Spotlight – Meet Trevor MacGinitie (Optimum Healthcare IT)
- Hazelden Betty Ford Taps Oracle Cerner and Xealth to Simplify Access to Addiction Treatment and Recovery Content (Cerner)
- A Different Point of View: EHRs Must Evolve into Platforms for Communities of Care (Medicomp Systems)
- The Healthcare Technology World is Becoming Flat (Get-to-Market Health)
- Pharmacists Will Rise to the Occasion with Paxlovid Prescribing (First Databank)
- Why Social Determinants are a Growing Priority (Get Well)
- Laying a foundation for the future: How will healthcare suppliers respond to an increasingly complex healthcare supply chain? (GHX)
- Why Digital Health Tools & Training are Key to Improving Community Health (The HCI Group)
- PROs & PROMs 101: An introduction to patient-reported outcome measures (Intelligent Medical Objects)
- Building Connections Through the Lyniate Partner Program (Lyniate)
- How Clinician-Driven EHR Design Improves the Anesthesia Experience (Medhost)
- The Healthcare Technology World Is Fast Becoming Flat (Get-to-Market Health)
- How personalizing Expanse unlocked new opportunities for patient care at Ozarks Healthcare (Meditech)
- How Post-Acute Leaders Are Solving Prior Authorization & Benefits Verification Challenges (Myndshft)
- A Wound Care Provider’s Alaska Adventure Begins (Net Health)
- The Dire Need for Integrated Behavioral Health in Chronic Care Management (NeuroFlow)
- When every second counts, connections matter (Nuance)
- Leveraging AI to Overcome Revenue Cycle Staffing Shortages (Nym)
- Overcoming frozen thinking in healthcare (Nordic)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.




























































Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…