Laura McCrary, EdD is president and CEO of the Kansas Health Information Network and KONZA National Network.

Tell me about yourself and the company.
The KONZA National Network was started in 2010 as part of the HITECH and the American Recovery and Reinvestment Act funding that was made available to each of the states. KONZA is a 501(c)(3) not-for-profit organization that is incorporated in Kansas under the name of the Kansas Health Information Network — KONZA is actually a DBA. The organization provides services not only in Kansas, but across the nation. The KONZA National Network provides health information exchange services as well as analytics services.
Kansas managed the process of establishing a health information exchange a little bit different from other states. That is relevant to the way that the KONZA National Network has developed. For example, Kansas didn’t stand up its own state-sponsored health information exchange like most other states did. Instead, Kansas established a process to certify the exchanges that did business in the state. Kansas didn’t give an allocation of state or federal funds to the health information exchanges. Instead, those funds went to the provider community to purchase interfaces and connect to the health information exchange. That was a key component of the development of KONZA and the health information exchange framework in Kansas.
The state then established specific criteria that all of the exchanges that did business in Kansas had to meet. You had to run a viable business that had providers and payers paying for the services that you provided. It was a subscription model, and everybody paid.
Also, you had to participate in supporting public health. You had to be involved in building the public health infrastructure. It was a partnership. The HIEs all agreed to send data for electronic lab reporting, syndromic surveillance, and immunizations. Kansas was well prepared for the pandemic because we had been working on that for 10 years.
The other thing that was interesting is that Kansas said that all data that was brought into the exchange also needed to be provided to the patients through a personal health record. Early on, all of the health information exchange data was provided to patients at no cost. That allowed us to be one of the early participants in the Harvard Open Notes model, where all of the data that we had available in the exchange was provided to patients.
It was a very different and unique model of certifying exchanges. One piece that was important was that all the exchanges that did business in Kansas had to connect to each other. While we may have been competitive, we also had to cooperate. That was a basis for how we were able to spread this exchange across the country. We had a commitment to all of the things that I just mentioned because of the way the initial Kansas HIE infrastructure was set up.
What are the implications of creating a national network?
Most of your readers will be familiar with the QHIN model under TEFCA that is beginning to come into fruition. The QHIN model is the Qualified Health Information Network model, sponsored by ONC and The Sequoia Project. KONZA has applied to be a QHIN and is working through that process now with ONC and the RCE. That will be an important development in interoperability across our nation, because we will see a number of QHINs that will have responsibilities to connect to each other and share data to establish that nationwide context.
The fact that KONZA already does business with exchanges in 11 states gives us an opportunity to be at the forefront of that. We run exchanges in Connecticut, New Jersey, Georgia, South Carolina, Mississippi, Louisiana, the Dallas-Fort Worth area, and obviously Kansas and Missouri. We also support an exchange in Northern California. That gives us a pretty broad national scope in terms of leveraging the QHIN model. We are excited about the possibilities of what the future looks like for health information exchange as we move forward into the later part of 2023 and 2024 and we have the QHIN model operational.
What challenges remain to giving patients the full benefit of interoperability?
There will continue to be issues with interoperability until we resolve the issues around standards in data sharing, the actual semantic interoperability of using a variety of different code sets. For example, it is still difficult to make sure that labs are being mapped properly to the LOINC codes and that SNOMED codes are being used properly. We often find that there’s still a lot of challenges in being able to do all of the proper coding and mapping.
We work hard at KONZA on data quality. We are part of the NCQA Data Aggregator Validation, or DAV project, where we take all of our practices and hospitals through DAV accreditation with NCQA to ensure that they have the highest quality of data that can be delivered. We check those things, like has the hospital mapped their labs properly to the LOINC codes? And are we seeing the proper procedure codes coming through? Are we seeing duplicates in data?
All of these things are still challenges for us. The data is still messy, so it’s important for us to focus on data quality. We have a couple of key vendors that are instrumental in helping us do that. But it is a core focus for us on data quality.
If you can’t get the data quality in the place that you need it to be, you are not going to be able to provide a complete and correct longitudinal record at the point of care for a patient. If a patient shows up in an emergency room and the doctor doesn’t know who he or she is, the doctor is dependent upon getting a longitudinal medical record from the health information exchanged to make sure that the physician knows all of the information about the patient before they begin providing care.
We are getting closer. Let me say that I feel enthusiastic about the future of health information exchange, particularly with the QHIN model that is coming into place. I think that we will see continued improvements in the data quality and the data completeness. But it’s still a work in progress.
The early days of RHIOs involved creating centrally administered platforms that left providers to figure out how to connect. How has that transitioned into a more services-oriented approach?
Health information exchanges flew under the radar from about 2010, when they were funded, up until about 2019 and early 2020 when the pandemic hit. Then it became clear to the entire nation that the health information exchanges had been developing products and services using the data that they were receiving through the health information exchange and aggregating that data and being able to turn it into meaningful information that could help to inform public health and others regarding the progress of the pandemic as well as the vaccination status of the population. Health information exchange quietly built that capacity over the years.
KONZA has 4,500 organizations that contribute data into the KONZA enterprise data warehouse. When we need to aggregate data across the nation and be able to track disease surveillance, the health information exchanges were well prepared to serve as that public health data utility to step into that space and provide information. For example, they provided COVID registries to the state of Kansas before they had the ability to get a registry set up. We set one up quickly for the state of Kansas in about 30 days, because we were already tracking the data and had it coming in for health information exchange purposes.
KONZA also has the ability to aggregate data across practices and across states to be able to look at quality measures. One of the things that KONZA does is calculate and compute quality measures, not only for physicians and hospitals, but across populations, whether it’s an independent physician association, an accountable care organization, or a Medicaid health plan that needs to be able to look at how they’re doing across their Medicaid population.
The health information exchanges have built that capacity and have been certified as having the highest quality data that’s available. It can be counted upon by payers, providers, and others as it relates to quality metrics. We see imminently on the horizon that quality measures will not just be calculated out of an individual EHR system. They will be calculated across all of the locations where the patient received care. That way, you have a holistic view of how a hospital or a physician practice is actually doing in providing quality care to a patient across the patient’s entire care team, as opposed to just looking at what happened at their facility.
How will you participate in clinical research?
We regularly get requests for de-identified data to be able to be used for clinical research. When KONZA, executes agreements with our participants, we have a secondary data use agreements that allows the data to be able to be used for purposes that advance medicine. Now, it can’t be used for purposes that would be used for marketing or for financial gain. But for clinical research that actually improves the practice of medicine, we have a team of doctors that meets to review each request that comes in to us.
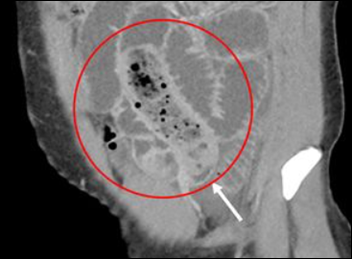
In the past years, we have focused on delivering data individually as each request came in. But we are building a product, which is being tested with a children’s hospital, that will provide de-identified data to the researchers at a hospital so that they can look into being able to use the data themselves, configure the data, and manage the actual research without us having to be involved. We are excited about our pilot project. I’m hesitant to name the children’s hospital, but it’s around how chemotherapy has affected children’s cardiovascular systems over time. Because we gather longitudinal records over time, we can often look across an individual’s life. We have, in many cases, 15 or 20 years worth of data that we can look at. Researchers are going to be able to take the data, model it themselves, and start using it for some amazing research that we haven’t been able to do before.
What strategies or tactics do you think will be important for the organization over the next three or four years?
Our work with the payer community is becoming more important. Many of your readers are all too familiar with payers having to send individuals out to pull records or asking practices or hospitals to send medical records so they can do their quality reporting around HEDIS and risk adjustment. That business is starting to become less and less because these records are all digitized. There is no reason to go out and make a copy of a medical record on the copy machine, ask someone to fax a medical record in, or have individuals spend time and precious resources doing things that are no longer going to be necessary as all of these records have become digitized.
More and more, we find that our business is moving towards providing data to the payers so that they can meet their quality goals around HEDIS and risk adjustment, which is one of the reasons that we are so focused on having the highest quality of data. We want to make sure that the data that we provide to providers is correct and complete, and to our payer customers is correct and complete. That is becoming an increased focus for us, to spend time working with payers, understanding the data that they need, the timeframes that they need it in, the format that they need it in, and to be able to deliver that payers. Our goal ultimately is that we can provide the products and services to the provider community in return for the data that we receive from them. We can provide that to the payers and eventually be able to reduce the overall cost to providers in our community to be involved in a health information exchange to a minimal amount. The providers are contributing their data, and we see that as being extremely valuable and we want to continue to build upon that perspective.
Comments Off on HIStalk Interviews Laura McCrary, CEO, KONZA































There was a time when my company went through multiple rebrands. These were relatively minor shifts, but completely unnecessary. It…