EPtalk by Dr. Jayne 11/12/20
My inbox has been bountiful this week, with so many good stories that link to healthcare IT that I just kept flagging items to come back and read later, only to find my entire screen full of flagged emails.
My urgent care is swamped with patients wanting COVID testing, and although there are enough supplies to go around, there simply isn’t enough staff. Since most of our payer contracts require patients to see a physician to document medical necessity for testing, and there’s only one of us at a site, it’s just an endless parade of testing visits. That is, until something acute comes in, and then there is an adjustment as we remember how to see “traditional” urgent care patients again.
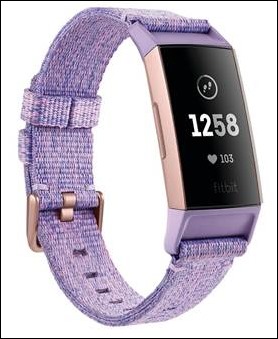
I was excited to see this article in Nature Medicine looking at how fitness trackers might be useful to detect biometric changes associated with COVID-19. I know patients will always want testing “to know for sure” as well as to make sure they can take advantage of workplace policies that require a positive test for paid time off, but it would be nice to have other tools that patients could use to help risk stratify themselves. That way they could figure out if they really need to stand in line for hours for a test at an urgent care center or if they could do a video visit with their primary physician and arrange testing at the health system’s drive through tent in a day or two.
The study Digital Engagement and Tracking for Early Control and Treatment (DETECT) study looked at data from more than 30,000 individuals from all 50 US states. They found that adding sensor data to symptom-based models improved their accuracy. Regional health officials in my area are lamenting the inability for temperature- and symptom-based screeners to identify infected patients, so at this point anything would help. Our schools just went back in person, and within 24 hours, were sending people home to quarantine due to exposure. The idea is that using device data could help identify clusters before infection spreads. That would have been useful in the aftermath of a recent parent-approved Halloween party thrown by some local teens, where over 200 high-schoolers attended.
A recent article in JAMIA looked at the advantages of human scribes compared to other options, particularly looking at patient safety aspects. They used a multidimensional sociotechnical framework to look at how different health systems use scribes. The dimensions were technical, environmental, personal, and organizational; 81 individuals were interviewed, including scribes and clinicians. They were asked about why they chose to use scribes as well as the background and training of scribes, along with pros and cons of their implementations.
One interesting finding was that since many health systems rely on college students for scribing, that geography is a factor in whether a practice can find a good scribe or not. That would definitely underscore why virtual scribe solutions are popular, since not every town has college students, let alone highly-motivated pre-medical or nursing students who would make good candidates.
Respondents did note a preference for real-time scribes versus using voice recognition software after the fact. The turnover in good scribes is an issue that was also validated in the research, and I experience that every year when medical school and physician assistant school acceptances are issued.
Fortunately, our scribe program staffs ahead of those transitions but it’s always a challenge to have the new scribes ramped up prior to flu season. You can bet that with COVID they’ve definitely earned every bit of experience they claim. I’m still waiting to hear from any readers (or friends of readers – come on, help a girl out here) who might be using one of the Ambient Clinical Intelligence solutions offered by Nuance or one of the other voice recognition vendors. There was a great deal of interest in the system at HIMSS a couple of years ago, but I have yet to encounter anyone actually using it in the wild.
The Journal of the American Medical Association tackled a weighty topic recently with its piece on “Science Denial and COVID Conspiracy Theories: Potential Neurological Mechanisms and Possible Responses.” Although this was a “Viewpoint” article rather than a research article, it has some interesting points. The first is the relationship between neurodegenerative disorders such as dementia with the adherence of an individual to false beliefs. Other psychiatric disorders include similar manifestations, such as delusions of grandeur and paranoia. The author proposes that false beliefs form due to faulty sensory information and impairment of brain systems designed to evaluate thoughts and beliefs.
Until reading the article, I had forgotten about Capgras syndrome, where certain dementia patients believe that a loved one has been replaced by an impostor. He explains the mechanisms by which that occurs as well as other delusions associated with dementia. He goes further to discuss the role of social media in amplifying conspiracy theories and other misinformation.
Based on what we know about dopamine and the addictive nature of social media, I can concur with his assertions. Mix in some low science literacy and we wind up where we are, with patients who legitimately believe that COVID is being spread by 5G cellular towers. He calls on the medical community to “mount systematic efforts around science education beginning in childhood and across the lifetime.” It’s a nice idea, but right now many of us are simply too exhausted from treating COVID patients.
From the Hall of Shame: Several towns along the east coast trusted a private physician to set up COVID testing clinics, but he proceeded to over test while billing exorbitant rates. Some patients were charged upwards of $1,900 and he was also recommending daily telehealth visits for a separate fee. Of course, his game wasn’t discovered until the bills started hitting, which typically takes at least 30 days for most patients with health insurance. Towns were effectively duped, with promises of a speedier economic recovery through greater testing. They in turn promoted the services, and then the physician took advantage.
Seems like a pretty clear ethics violation and I hope the relevant licensing boards take note. The physician is clearly delusional, stating that he tested for all kinds of other respiratory viruses because “just testing for coronavirus is one of the most dangerous things you could do… it is crystal clear that mentality is bad for public health.” I’d argue that unnecessary testing is also bad for public health, as is medical bankruptcy. People like him are the reason patients don’t trust the medical establishment. It takes far too many good experiences to undo the damage caused by a bad apple like this one.
Have you received a balance billing statement for COVID testing or related services? Leave a comment or email me.

Email Dr. Jayne.


So your contention is that DOGE was a good-faith administrative effort? LOL! Parachuting in unqualified outsiders ought to be a…