Yes! Flip flops are essential as the back up for professional footwear. Plus they are easy to put into your…
News 4/24/20
Top News

Banner Health will pay $8.9 million to settle claims from its 2016 data breach. An Arizona federal judge approved the settlement, which was reached in early December, on Tuesday.
Each patient who is covered by the class action will receive $500, while the plaintiffs’ attorneys will earn $2.9 million.
Cyberattackers breached Banner’s credit card payment system that is used in its food outlets, then extended their attack to other systems, exposing the information of 3.7 million patients and health plan members.
Reader Comments
From COVID Thoughts: “Re: traveling contractors. How will hospitals address vendors and consultants coming on site post-COVID? If widespread testing is not available, will they permit traveling contractors in their hospital and office buildings?” I’ll open the floor to what, at this point, will be speculation at best. I assume that whatever precautions hospitals will take with patient visitors – temperature checks, limits on numbers, etc. – will be applied to business visitors, but I wouldn’t expect getting them into the building will be a high priority. They could require meeting at locations other than buildings where patient care is provided.
From Disengage: “Re: chatbots. Those should keep people out of the ED even after the pandemic is controlled.” Don’t count on it. The customers of those chatbots are health systems who make a lot of money from ED patients in normal times, where the ED helps keeps heads in beds. The sudden interest in doing the opposite — keeping people away from the ED who don’t need to be there — could well be temporary. Health systems are happy to have full EDs as long as someone is paying, and I expect them to deploy their post-pandemic chatbots accordingly. You don’t run a successfully restaurant by testing prospective diners to verify that they are actually hungry.
Webinars
April 28 (Tuesday) 1 ET: “COVID-19: Managing an evolving patient population with health information systems.” Sponsor: Intelligent Medical Objects. Presenters: Julie Glasgow, MD, clinical terminologist, IMO; Reeti Chauhan, senior product manager, IMO. IMO recently released new novel coronavirus descriptors to help clinicians accurately record diagnoses and also created free IMO Precision COVID-19 Sets to help identify and analyze patients with potential or documented infection. The presenters will discuss these new tools and describe how to use them optimally.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Sales
- Cerner expands its VA contract with Vecna Technologies to include greater EHR systems integration and go-live support at Mann-Grandstaff VA Medical Center (WA).
- TCARE, which offers a family caregiver support program, will use CareSignal’s COVID-19 programs (linking to local public health resources and information, a self-monitoring text system, and staff support) for its 20 million members.
- The VA expands its contract with CirrusMD for the text-based VA Health Chat, in which VA employees provide medical advice, manage prescription refills, and schedule appointments.
Announcements and Implementations
Cleveland Clinic and SAS share predictive modeling code on GitHub that can help hospitals better prepare for COVID-19-related supply chain, capacity, medical device, and financial scenarios.
The Dallas VA implements cloud-based COVID-19 monitoring, surveillance, and tracking solutions custom-developed by CliniComp across 42 sites.
The Regenstrief Institute partners with the Indiana Health Information Exchange, Indiana University School of Medicine, and several state-based agencies to develop a COVID-19 tracking and response dashboard using data from the state’s health systems and labs.
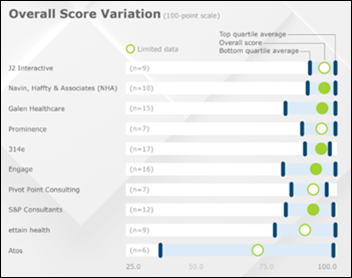
A KLAS report on technical services providers finds that Galen Healthcare and 314e have the broadest range of clients, J2 Interactive and Navin, Haffty & Associates are most consistent in client satisfaction, and those four vendors offer the best balance of prce and performance. Client scores from Atos, which grew in the US by acquisition, place it at the bottom. Prominence earned top scores for quality of staff and its deep Epic expertise.
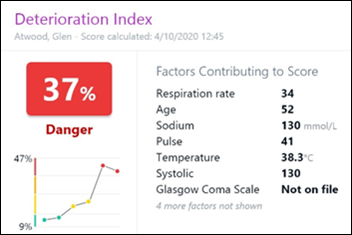
Epic reports that hundreds of hospitals are using its machine learning predictive model to alert clinicians of patients whose conditions are worsening. COVID-19 modules are being validated and used.
Government and Politics
HHS updates providers on the distribution and timing of CARES Act Funds, stressing that payments will be made weekly beginning Friday. High-impact areas such as New York will be allocated $10 billion.

EHR vendor KPMD pays $1.7 million to settle charges that Southwest Regional Medical Center (OH) falsely attested to state and federal governments that its ED met the requirements for EHR incentive payments even as the hospital was shutting down. KPMD’s contract called for the hospital to send the company its government incentive payments. KPMD’s CEO Krishna Surapeneni later bought the hospital in September 2013 and closed it one year later.
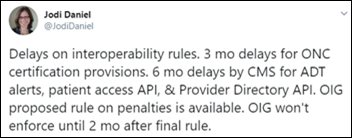
CMS, ONC, and the HHS Office of the Inspector General announce they will delay enforcing compliance with final interoperability rules so that healthcare stakeholders can focus on COVID-19-related operations.
FedScoop profiles HHS Protect, health data visualization technology used by the White House’s Coronavirus Task Force that comprises 187 datasets from federal agencies, state governments, healthcare facilities, academia, and industry partners. The dataset, developed and managed by the HHS Office of the CIO, gives 200 users access to COVID-19 case count sources; hospital capacity, utilization, inventory, and supply data; government and industry supply chain data; lab testing data; and data from community-based testing sites.
COVID-19
Scientists determine that coronavirus was spreading undetected in the US by early February and the first known death occurred February 6, as international and domestic travelers then spread the infection. New York City had 600 people with unidentified infections in mid-February and confirmed its first COVID-19 case on March 1, but the city may have had more than 10,000 cases by then.
NIH Director Francis Collins, MD, PhD cites research that found that 44% of coronavirus transmissions occur before the infected person develops symptoms, which will make contact tracing harder. Those studies suggest that people can spread the infection for 2-3 days before they become ill themselves, which then requires tracking down and quarantining 90% of their close contacts who by then have been exposed.
A Health Affairs blog post warns that US maps that show few COVID-19 cases outside of metro areas are misleading, concluding that “the virus is everywhere” based on hospital referral regions where people travel across county and state lines to seek hospital care. Case rates are increasing in all of those regions. The authors recommend that the referral region information be considered by states that are loosening their distancing requirements.
A Kaiser Family Foundation poll finds that:
- 51% of Americans think the worst is yet to come with coronavirus, down 23 percentage points from three weeks ago.
- 80% say shelter-in-place is worth it to protect people and limit spread.
- The majority of respondents say they can continue physical distancing and shelter-in-place for more than another month.
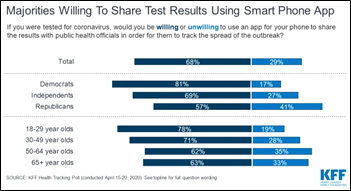
- Two-thirds of people support phone-based contact tracing after they were told that it could allow schools and business to reopen.
- Twice as many people would be willing to download a contract tracing app if the data was managed by local or state health departments or the CDC instead of a technology company.
- 38% worry that companies will sell data from contact tracing apps, while 33% think the federal government will use the data for purposes that go beyond tracking coronavirus spread.Two-thirds say they would not feel safer if phone-based contact tracing were in place.
Partners HealthCare (MA) turns its internal employee communications app into a COVID-19 messaging tool, giving its 78,000 staff members daily updates on testing protocols and stay-at-home policies.
Johns Hopkins University hosts a free public course titled “Understanding the COVID-19 Pandemic: Insights from the Experts.”
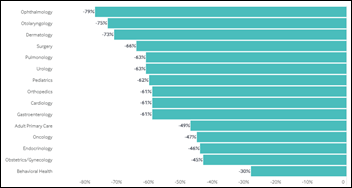
Researchers find that ambulatory practice visits dropped 60% overall starting in mid-March, a reduction that has not been fully offset by the upswing in telehealth visits.
A study finds that of 318 coronavirus outbreaks (three or more cases) in China, only a single outbreak happened outdoors and that outbreak involved just two cases. The study did not take note of the fact that most of the outbreaks occurred during winter when people would have been mostly indoors anyway, but the results may still encourage states to allow churches, restaurants, and gym classes to reopen with a recommendation to use outdoor spaces. The study also found that home contacts were involved in 80% of outbreaks and most of those involved 3-5 cases. A significant percentage involved public transportation.
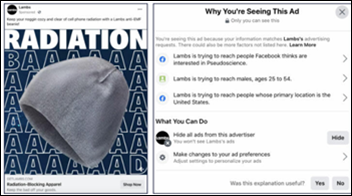
Facebook removes its “pseudoscience” user interest category — which tagged 78 million people — after a website discovered the targeting option when its reporter was served an ad for a radiation-blocking hat. Consumer Reports found that despite Facebook’s declared crackdown on false pandemic content, the magazine was able to buy ads claiming that social distancing doesn’t work and that drinking bleach preserves health.
Drugmaker Jaguar Health — whose only product is the diarrhea medication Mytesi that is approved for use in HIV/AIDS patients who are being treated with antiretroviral drugs — raised the price from $11 to $37 per tablet in early April, right after asking FDA to allow its use for COVID-19 patients being treated with remdisivir. The FDA denied the request. The company says it is going broke fast because insurers won’t pay for Mytesi, which is made from tree sap.
Privacy and Security
Hackers expose the stolen logon credentials of 25,000 users from WHO, NIH, CDC, and the Gates Foundation. WHO says only 457 credentials of the original 6,835 remain active. A white-hat hacker who gained access to WHO’s system using the stolen data says that nearly 50 accounts use “password” as their password, while others use the user’s name or “changeme.” White supremacist groups that have targeted hospitals and medical workers published the stolen credentials to their members almost immediately.
Other
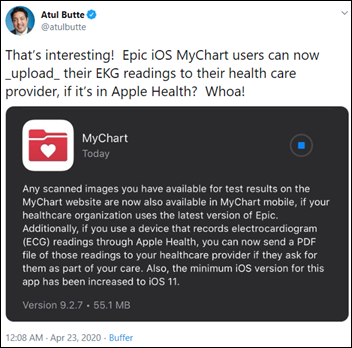
USCF’s Atul Butte tweets that patients can send their Apple Health-stored ECGs to their providers using Epic’s MyChart patient portal.

Hospitals that hope to avoid Joint Commission penalties by throwing away medical supplies with a close expiration date are now scrambling to obtain PPE.
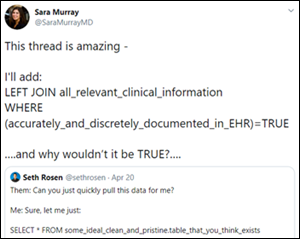
This is pretty great.
Sponsor Updates
- CareSignal and Texas Health Aetna launch a free, text-based COVID-19 education messaging service.
- Ellkay releases a video in celebration of Medical Professionals Week 2020.
- The Big Unlock Podcast features Wolters Kluwer Health VP and General Manager of Clinical Surveillance Karen Kobelski.
- Hyland Healthcare and HIMSS Media publish 2020 Connected Care and the State of Interoperability in Healthcare study results.
- Imprivata expands its collaboration with Microsoft to offer new digital identity innovations.
- InterSystems announces that RxMx has built its new Chameleon platform on InterSystems IRIS for Health, powering a new COVID-19 testing and monitoring solution for employers.
- Glytec customers AdventHealth and CHI Franciscan will lead the “Computer-Guided Insulin Dosing” session at the 2020 Diabetes Technology Society Virtual Hospital Diabetes Meeting April 24 at noon ET.
- The local business paper profiles the rapid uptake in adoption of the Healow telemedicine app from EClinicalWorks.
Blog Posts
- Adding Value in 2020: Keeping It Simple (PMD)
- Shift in the Medical Mindset (EClinicalWorks)
- New Feature Lets Users Instantly See if a PAC Provider Accepts COVID-19 Patients (Ensocare)
- Intelligent Monitoring of the End-User Experience is Necessary in Healthcare Environments More than Ever (Goliath Technologies)
- Protecting businesses against cyber threats during COVID-19 and beyond (Google Cloud)
- Resolve these 3 front desk challenges (Greenway Health)
- Local Telehealth Businesses are Booming During the Pandemic (HCTec)
- COVID-19 and the Importance of Health Informatics (Healthcare Growth Partners)
- Furry Friends of Healthfinch (Healthfinch)
- COVID-19, Loneliness, and Cabin Fever (Healthwise)
- Enterprise Imaging: Answers to Fundamental Questions (Impact Advisors)
- Maximizing capacity for rescheduled elective and routine care (Nordic)
- Tips I learned running IT for the US Air Force during 9/11 (Imprivata)
- Virtual Care Visits and the Importance of Electronic Data Access (InterSystems)
- Business as (un)usual: Security, continuity, and the COVID-19 response (Intelligent Medical Objects)
- How Health Systems are Responding to COVID-19 – And Using Tech to Do It (Kyruus)
- Combatting COVID: 5 Benefits For Text-Based Screening Tools (Dina)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



Re: people throwing out PPE in advance of a Joint Commission inspection out of fear of being caught with expired supplies: This is totally believable.
Everyone is terrified that the surveyors will find some minute arcane thing that no one would ever dream of being a problem and then cite you for it. I understand that the intent of the Joint Commission is good and the surveyors always say they are just implementing CMS rules, but after 40 years of working in hospitals, I generally see their review process and requirements as more of a hindrance than a help. If there’s anything good that could come out of this horrible pandemic, perhaps Joint Commission and CMS could get together and get rid of all of the silly requirements that bog down care delivery and are just costly and unnecessary as this incident points out.
There’s a saying among pilots and the trades that “safety codes are written in blood.” Safety regulations tend to be written in response to incidents that led to serious harm or loss of life. Just because your organization hasn’t accidentally administered vercuronium instead of versed doesn’t mean that JC regulations to prevent such an event are silly.
Undoubtedly there is probably some chaff in the safety regulations (I completely agree that “expired” face masks is kinda silly), but the idea that most of the regulations are pointless and silly is missing the point.
Additionally the regulators need to engender good faith trust from the industry. If hospitals see the JC surveyors as people who are trying to find something to ding them for, then the process becomes hostile and combative, and the regulations end up being seen as detrimental. It’s really on the JC to fix the perception problem.