Monday Morning Update 3/11/19
Top News
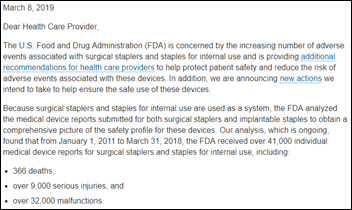
FDA has given the manufacturers of surgical staplers an exemption from publicly reporting problems to its MAUDE database of medical device failures, allowing them to hide widespread problems by submitting just 100 incidents in 2016 vs. the 10,000 that were actually reported.
FDA’s alternate summary reporting program – created to save FDA employee processing time — allows manufacturers to send a quarterly or annual spreadsheet list of problems instead of detailed reports.
Several experts, including former FDA Commissioner Rob Califf, said they’ve never heard of the program. Companies that use the option tend to keep quiet about it to prevent competitors or prescribers from finding out the true patient impact.
Among the non-reporters are manufacturers of pelvic mesh, the da Vinci surgical robot, and several critical heart devices.
FDA responded to the Kaiser Health News report by saying it will analyze the summary reports, also adding it will make public the 41,000 safety reports it has received that involved surgical staplers. Those reports included 366 deaths, 9,000 serious injuries, and 32,000 malfunctions.
It’s puzzling that FDA received so many patient safety incident reports that it decided its best action was to stop requiring them.
HIStalk Announcements and Requests
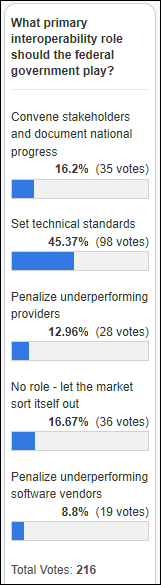
Around half of poll respondents say the federal government’s role in interoperability should be to set technical standards, while the distant #2 choice is for the federal government to stay out of it entirely and let the market figure it out.
New poll to your right or here: for provider employees, how much time and energy does your employer devote to planning or delivering value-based care?
Webinars
March 27 (Wednesday) 2:00 ET. “Waiting on interoperability: What can payers and providers do to collaborate?” Sponsored by Casenet. Presenter: Amy Simpson, RN, director of clinical solutions, Casenet. A wealth of data exists to identify at-risk patients and to analyze populations, allowing every payer and provider to operate readmissions intervention and care management programs. Still, payer and provider care managers are challenged to coordinate and collaborate to improve outcomes because of the long road ahead to interoperability. Attend this webinar to learn what payers and providers can do now to share information and to coordinate their efforts to create the best healthcare journey for members and patients.
Previous webinars are on our YouTube channel. Contact Lorre for information.
Sales
- Medway NHS Foundation Trust joins TriNetX’s global health research network to attract more clinical trials and to support research collaboration.
Decisions
- Firelands Regional Medical Center (OH) replaced Aris Radiology with REAL Radiology For teleradiology in fall 2018.
- Braxton County Memorial Hospital (WV) will Implement Epic in June 2019.
These provider-reported updates are supplied by Definitive Healthcare, which offers a free trial of its powerful intelligence on hospitals, physicians, and healthcare providers.
Privacy and Security
Columbia Surgical Specialists (WA) pays $15,000 to regain access to its data following a ransomware attack, explaining, “We received notice from the people that encrypted the files just a few hours before several patients were scheduled for surgeries, and they made it clear we would not have access to patient information until we paid a fee.”
Other
Kaiser Permanente apologizes for one of its doctors telling a 79-year-old inpatient that he is dying via a telemedicine robot. The family says it was hard to hear what the doctor was saying due to the robot’s small speaker, but it was clear when he said, “I don’t know if he’s going to get home” due to the patient’s failing lungs. The man’s daughter recorded the incident on video thinking the family would be receiving care instructions. The patient died two days later. It sounds harsh, but I’m not so sure – not all telemedicine visits will result in good news, the provider isn’t necessarily geographically accessible to the patient, and the idea that empathy requires physical presence may need to be challenged. Or perhaps it’s unreasonable to expect skilled clinicians to be good at comforting patients or consoling their families as much as we as patients would like it. There’s probably no good way to be told – accurately, as it turns out – that you are dying.
23andMe will add type 2 diabetes risk factors to its consumer genetic screening once FDA approves the test, although the science behind it is shaky (it looks at a package of existing genetic traits rather than a specific genetic abnormality and it is known to be super inaccurate for black Americans, for example) and it has not been reviewed in the medical literature. My questions:
- How many people already have known diabetic risk factors, what are they doing about it, and how does this new test benefit anyone other than 23andMe?
- A big percentage of people have known diabetic risk and it’s not clear how many of them take action that are proven effective to avoid moving to active diabetes. What would patients do differently from the results of this test? How does this test change outcomes?
- What is the immediate course of action for someone who tests positive? Call their PCP for an immediate appointment and then be identified for life as “prediabetic” and run up bills for drugs and monitoring? Who’s going to pay? How many of those patients have already been told by their PCP that they are at risk but haven’t done anything?
- Is 23andMe motivated more by its partner agreements that allow those who are identified as being at risk to sign up for paid coaching programs?
- As one expert says, “You might as well just look in a mirror. That’s as good a predictor for diabetes as all your genes put together.”
- Every medical student is taught that you don’t measure something just because you can — the course of action is uncertain; chasing a lab result isn’t necessarily beneficial to the patient; medicalizing a symptom-free patient often doesn’t make sense; and plenty of people already have diabetes but don’t receive treatment.
- The odds that this test will move the US public health needle is just about zero despite our widespread (and profitable) misperception that we just need to diagnose more stuff.
Sponsor Updates

- US Air Force Reservist Senior Master Sergeant Andrew Branning, director of CloudWave’s project management office and quality and recently returned from overseas deployment, nominates his supervisor Mark Middleton, VP of cloud services and chief quality officer, for the Patriot Award. The award, overseen by the DoD’s Employer Support of the Guard and Reserve, allows citizen soldiers to recognize the supervisors who support their work by offering flexible schedules, time off before and after deployment, and family care.
- Seven hospitals in Mississippi and Alabama form the Mississippi Meditech CIO Collaborative to share common goals, challenges, and a dedication to improving healthcare with EHR technologies.
- Medhost enables integration of National Decision Support Co.’s CareSelect Imaging with its EHR.
- NextGate will exhibit at State Health IT Connect Summit March 18-20 in Baltimore.
- Clinical Computer Systems, developer of the Obix Perinatal Data System, will exhibit at the AWHONN Virginia Section Conference March 17-18 in Charlottesville.
- FlyWire’s global payment and receivables business accelerates into 2019 after integrating OnPlan Health.
- Experian Health will exhibit at the Semi-Annual ACO Leadership Forum March 11-12 in Chicago.
- Sansoro Health releases a new podcast, “The Power of Patient & Family Engagement.”
- Vocera will exhibit at the NYONEL Annual Meeting & Leadership Conference March 17 in Tarrytown.
Blog Posts
- Transforming Health: Health IT and Patient Access (Vyne Medical)
- Let’s celebrate nurses in 2019 (Meditech)
- Top 5 challenges in claim status inquiries – and how to solve them (Waystar)
- Government to private industry: Take the lead in patient records matching (NextGate)
- Customer Success Story: MMR Healthcare — Using Data to Defeat Diabetes (EClinicalWorks)
- Out with the Old: Comprehensive Nursing Systems’ Transition (Netsmart)
- Charge Reconciliation Training, Maintenance, and Accountability (CereCore)
- How AdvantageCare Physicians increased security of patient portals (Experian Health)
- 3 Steps to Amplify Conversion Rates from Print Campaigns for Health System Marketing (PatientBond)
- Is It Time to Upgrade Your Patient Payment Software? (Patientco)
- It’s Time to Simplify Docs’ Docs (PatientKeeper)
- What physicians need to do to change patient behavior (PerfectServe)
- 5 reasons why you shouldn’t do direct-to-database ER integrations (Redox)
- Your Patient Access Management Opportunity (The SSI Group)
- Technology as extra eyes and ears. (Voalte)
- 10 Physical Therapy Marketing Metrics that Matter (WebPT)
- A digital platform for value-based care management (Philips)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates. Send news or rumors.
Contact us.




Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…