Traditionally Professional Courtesy is something that physicians gave each other - but we had to be careful with it when…
Monday Morning Update 8/2/10
From Capillary: “Re: Allscripts. The CEO announced last week on the earnings call that the company was chosen by the Indiana REC, but the selections have been announced and Allscripts was left off. Anyone know what happened?” Allscripts confirms that you are correct. They have apologized to the REC for the unintentional miscommunication. The vendors chosen by the Indiana HITEC as appropriate for small and rural providers are athenahealth, iSALUS, and MDLand.
From UK Watcher: “Re: Aspira. Aspira is/was the UK feeder to IntelleHealth/iCapital, the consulting entity working some of the Cerner projects in the Middle East. Many of the recruits that they had secured in the UK were from Cerner UK and had been moved to the ME anyway. Will be interesting to see what happens to their tax-free and prior negotiated packages with the ‘new’ boss.”

From Privacy NOT: “Re: security breach. The Achilles right heel of HIT is failed privacy. The Achilles left heel of HIT is failed safety and efficacy. The rotator cuff tear of HIT is failed usability.” I don’t know about all of that, but it was in response to news of a stolen laptop from Thomas Jefferson University Hospital in June. The laptop was password-protected, but was not encrypted (I swear the hospital laptop encryption rate must be even lower than CPOE adoption, but in this case, it the employee’s personal laptop and storing PHI on it violated hospital policy). Laptops apparently aren’t encrypted at Texas Children’s Hospital either, as the hospital admits after the theft of a doctor’s laptop containing patient information.
From Smart Room Needed Here: “Re: UPMC. Hospitals should get their employees to watch the monitors.” A patient’s family sues UPMC Mercy Hospital, claiming he suffered permanent brain damage after choking on a clogged tracheotomy tube for 40 minutes before ICU nurses answered the cardiac monitor alarm. And in other UPMC news, it creates a VP of community relations position for a state senator who’s quitting. The closed UPMC Braddock Hospital is in his district, leading an official with Save Our Community Hospitals to state, “… Sen. Logan worked to ensure UPMC’s objective of closing and demolishing the hospital. Now we know why. Mr. Logan has received his ’30 pieces of silver’ as payoff for his work on UPMC’s behalf.”
A reader asked me to put together a list of some of the music I’ve recommended over the years, so I compiled and posted a list here. And in digging back through those archives, I dug up an old favorite to revisit: Nine Black Alps, hard rocking Brits.
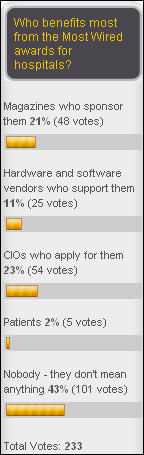
As hospitals issue press releases congratulating themselves on being Most Wired, most HIStalk readers think awards of that type mean nothing, while the majority of the remainder think they’re just self-promotion for magazines and CIOs. New poll to your right: will state HIEs be viable once their stimulus money has been spent?
Speaking of Most Wired, AHA says the criteria have been toughened up, requiring hospitals to at least claim (on the self-reporting survey) that they are actually using technology. So, if you are among the Most Wired skeptics who think it means nothing, imagine what it was like before (those old and now-suspect awards still pepper CIO resumes, I’m certain). If this were an art contest, it has gone from (a) who owns the most paintbrushes, to (b) who uses the most paintbrushes, but is still far short of actually evaluating (c) whose painting is the best and whether having the most paintbrushes made any difference. I was in charge of completing the survey for a Most Wired hospital for several years (I have a Most Wired Winner shirt somewhere) and even my hospital made fun of it given our hopelessly outdated and seldom-used clinical systems back then. I suspect that we and our fellow award-seekers were as optimistic as a vendor’s RFP department in our responses.
Are patients better off in a Most Wired hospital and can it be proved that the technology is responsible? No on both counts. As I always say, if you are a good hospital, judiciously deployed IT can make you a little bit better. If you’re a bad hospital, all the technology in the world probably won’t help you improve (and may well increase your level of suckitude). If you are marginal, you might see improvement, but I wouldn’t count on it.
The folks at FierceHealthIT and I are swapping links for a few weeks, so you’ll see their headlines to your right and mine on their site. It’s a trial to see if we send each other readers. If not, we call the experiment quits.
Scott Storrer is ousted as CEO of MEDecision, replaced after just eight months by un-retiring founder David St. Clair (above) until a permanent replacement is named in six months or so. David’s blog entry on the subject is here.
Q1 numbers from NextGen parent Quality Systems: revenue up 24%, EPS $0.42 vs. $0.36, missing on consensus earnings.
A reader sent over workshop documents from a July 27-28 invitation-only meeting involving the Institute of Medicine and ONC, addressing the role of technology in continuous healthcare improvement. Some of the issues discussed: what can IT do to improve health and healthcare by 2020, what are the rate-limiting issues, how can data be used, how can innovation be fostered, how can healthcare cost be reduced by technology, how can disease management be improved by technology, how can consumers be engaged, and how can a global public network be created? Some familiar names were on the participant list: Molly Coye, Bill Bria, Mark Frisse, John Halamka, Rob Kolodner, Marc Probst, Stephanie Reel, and Paul Tang (familiar names not on the list were yours and mine).
UMass Memorial Health Care will announce Monday that it has chosen the Symedical terminology management and interoperability tool from Clinical Architecture to create a central data repository with a single terminology set.
HIStalk sponsor jobs: Interface Analyst, Epic Clarity Analyst, RVP Sales – Southeast, New England/NY, and Mid-Atlantic Territories.
McKesson’s Q1 numbers: revenue up 3%, EPS $1.10 vs. $1.06. My interpretation of nuggets from the call transcript: (a) Health Solutions and RelayHealth did fine; (b) Provider Technologies (the hospital technology part) underperformed, with revenue growth slowing to just 2% and profit down 7%; (c) they’re spending a lot of money on Horizon Clinicals and Horizon Enterprise Revenue Management, taking an $8 million accounting hit on HERM amortization during the most recent quarter alone; (d) John Hammergren says the company is interested in global acquisitions, but is often named just to increase the price that someone else eventually pays; (e) MCK isn’t seeing an increase in technology purchases by physician practices, but Hammergren says it’s because those practices aren’t yet paying attention to HITECH; (f) the company is confident that its products can get providers to Meaningful Use. My cheap seats analysis: Horizon Clinicals and HERM are struggling, which is hardly news other than it’s McKesson saying so (indirectly).
HHS withdraws HITECH’s breach notification final rule after reviewing the public comments. Organizations involved in a privacy breach would have been allowed to decide on their own whether to notify patients or just keep them secret. That’s significant given that the rule had already gone to OMB. A replacement rule will be issued “in the coming months.”

DrLyle weighs in on Meaningful Use on HIStalk Practice. A snip: “To correctly measure many of these details (e.g. give clinical summary to 50% of those who ask) we would need to figure out a way to keep track of who ‘asks’. That seems like a strange request for structured data and certainly should not be what a doctor is spending his time doing.”
Dossia Consortium names Jim Hansen, former CEO of the Kansas City-based CareEntrust HIE, as VP and executive director.
TriHealth and University of Cincinnati will spend up to $100 million each on clinical systems, with Epic being a candidate in both (I’d say shoo-in given that TriHealth already uses Epic in its physician practices). Also named as local hospitals bringing up Epic and spending more than $50 million each to do so: Mercy Health Partners, Cincinnati Children’s, Christ Hospital, and St. Elizabeth.
A senior at University of Maryland who created the DoseSpot electronic prescribing system is named a finalist for an entrepreneur award.
Doctors and nurses in Thailand wear black lab coats to protest a draft law that would allow patients to be immediately compensated for medical malpractice from a special fund. A medical union representative says, “It means our staff would have to be extra careful during work, which would decrease efficiency.”
An Alaska clinic becomes the first US site to use ALERT Clinic software, which I assume is from the Portugal-based ALERT that made a mini-splash a couple of years ago at HIMSS (I think I recall cute booth staff in red-striped white jumpsuits, but I could be wrong), then seemed to disappear without a trace. Everybody (me included) was impressed by what we saw, so I don’t know what happened. I pegged them as a hot new entrant.
A hospital employee is fired for posting a Facebook comment about the suspected killer of a police officer that she treated, saying she hoped he rotted in hell. The hospital said she violated HIPAA even though she didn’t mention the name of the suspect or her hospital.
A Stanford Medical School professor and novel writer worries about letting technology interfere with patient-physician relationships:
Rituals are about transformation. You know, we marry with great ceremony to signal a transformation. We are baptized in a ritual to signal a transformation. The ritual of one individual coming to another and confessing to them things they wouldn’t tell their spouse, their preacher, their rabbi, and then even more incredibly, disrobing and allowing touch, which in any other context would be assault, you know, tell me that that’s not a ritual of great significance. And if we short-change the ritual by not being attentive, or you are inputting into the computer while the patient’s talking to you, you basically are destroying the opportunity for the transformation. And what is a transformation? It’s the sealing of the patient-physician bond.
Hospitals in Victoria, Australia will arm 500 doctors and nurses with iPads in a pilot program.
Boy Scouts at this year’s Jamboree at Fort A.P. Hill, Virginia have access to AT&T WiFi and a wireless EMR system used by its 20 medical centers and team of EMTs. Next thing you know they’ll be using a GPS to track snipe.
Standard Register’s healthcare revenue fell short of expectations in Q2, mostly because of cheaper document management solutions.
The former CEO of Baltimore-based insurance company CareFirst BCBS, recipient of a contested $18 million severance package, joins Healthcare Interactive as an advisor. The company offers healthcare performance management systems of several types.






Don’t have to worry about the Boy Scouts — they already have GPSr’s! One of the lastest badges is the “Geocaching Badge”. You can find more about the hobby at http://www.geocaching.com — and I can tell you, its addictive!
Love the press release about the use of technology in a mobile environment!
The Stanford Medical School Professor makes a valid point: “And if we short-change the ritual by not being attentive, or you are inputting into the computer while the patient’s talking to you, you basically are destroying the opportunity for the transformation.”
This cognitive and spiritually functional concept relates to your report of the patient at an award winning computerized modern hospital in Pittsburgh, who, together with the monitor was allegedly ignored and is now brain damaged. There are many nurses, doctors, respiratory therapists, students, PAs, NPs, and consultants, in ICUs at that hour of the morning.
What are their rituals now, exactly, with all of the wires connecting to EMRs?
Privacy breaches are under reported. Secretary Sebelius appropriately acknowledges the HHS’s failure to understand the magnitude and implications of the breaches by rethinking the protections when stating: “This is a complex issue and the Administration is committed to ensuring that individuals’ health information is secured to the extent possible to avoid unauthorized uses and disclosures, and that individuals are appropriately notified when incidents do occur.”
Additionally, the sale of any data, even if “deidentified” should be banned.
McKesson continues to struggle with Horizon Clinicals and HERM. The massive upgrade, which only begins to move those clinical applications onto one database has been ongoing for five years now and remember, it is just the beginning of moving all those apps onto one database. HERM is clearly not making the impact MCK had intended when they spent over $150M in its development.
Relay Health financial transactions are the products posting gains. The Relay physician connectivity products aren’t doing well as they were not initially intended to be HIE’s.
Overall, it appears MCK is struggling. In addition, to this, they continue to RIF employees and have employees leave, as well as significant senior leadership changes.
None of these things are signs of a healthy company.
I understand what the good doctor means when speaking of the ritual of a patient/physician interaction. But the other rituals he references are all once in a life time experiences that we set a date aside for and elaborately plan. Compare the preparations made for a wedding to that made for an emergency trip to the doctor; now compare how long a full wedding ceremony lasts compared to a typical visit’s duration, with a physician you may not even know. Besides the physical nature of disrobing, there’s little intimacy involved.
Some physicians can be just as buried in their paper records and own theorizing as others who might be distracted by a computer terminal. The best doctors will overcome these barriers and still focus on the patient. Certainly, I’ve had my share of negative physician encounters that had nothing to do with the technology involved.
By the way, thanks for the Up! reference, it made a nice diversion–squirrel!
Dr. Verghese is spot on. Faith is vital to medical care and is the fundamental tenet of the doctor patient relationship.
Faith in the computerization of medical care is heretical, especially considering th reports of adversity you have posted on your great site. These adverse events and situations that sap the faith include privacy breaches, defects in the software, conflicts of interest which promote wealth of the vendors and their lobbyists, but not the health of the patients, unusability of the devices that ultimately cause serious interference with the relationship between doctor and patient.
Thank you Mr. HIStalk for educating us.
So now a nurse not reponding to an audible alarm is the EMR’s fault?
Hi Histalk – any insight on the reason why CEO of MEDecision, Scott, was removed. the official release says, obviouly, other pursuits. any insider inputs or market news you heard of? (I last heard the Med was doing real good, so this comes as a surprise, given that their parent HCSC brought Scott in with a lot of fanfare).