EPtalk by Dr. Jayne 8/13/15
CMS continues to remind everyone that the ICD-10 transition is less than 50 days away. Unfortunately this seems to be news to some. I’ve been absolutely inundated with requests for ICD-10 training. I suspect the previous delays encouraged some providers to procrastinate, thinking there would be another reprieve. I’d be seriously surprised if there is one, so if you haven’t started prepping, now is definitely the time. My free consulting advice:
- Every provider should have a list of his or her top 50 diagnoses and should practice documenting those diagnoses in the EHR, either with dual-coding on a live system or otherwise in a test system.
- By specialty, providers should know what common codes might have pitfalls and be ready to diagnose them.
- Organizations should follow their vendors’ ICD-10 readiness checklists. Some EHRs require updates and there may be nuances on how they need to be applied compared to “typical” updates given the number of moving parts for ICD.
- Each office should identify an ICD-10 point person to handle issues on October 1.
- Everyone should dust off their business continuity plans. Your office may be OK, but your clearinghouse or payers may not, so it pays to think through the possibilities.
CMS also sent out a link to the National Broadband Map, where providers can see if they will qualify for certain Meaningful Use exclusions based on the availability of broadband service. I don’t qualify for an exclusion, but the page did have some interesting information about my county, including racial and ethnic data, median income, poverty rate, and educational status.
My former employer still hasn’t figured out how to remove me from all its email distribution lists. From time to time I still receive confidential information, including physician performance data. This week I received a system-wide bulletin stating that in order to prepare for ICD-10, effective next week the hospitals are no longer going to accept only ICD-9 codes for the patient diagnosis. Physicians must include a narrative description of the diagnosis if they want their orders to be processed. Quarterbacking from afar, I think a week’s notice is pretty short and the lack of a grace period isn’t very provider-friendly. They also didn’t mention what they would do when orders are received without a narrative. Will the patient be turned away? Will someone try to contact the provider? Heaven forbid will someone whip out a code book and scribble a narrative on the order so the patient can be taken care of? I’ve asked a couple of my former colleagues to let me know how it goes.
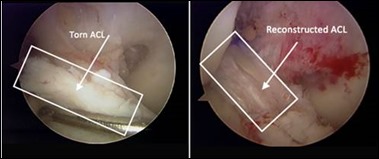
I wrote a few months ago about a friend who had knee surgery and some of her experiences while I played patient advocate for a day. She still hasn’t gotten a full copy of her records, but watching the bills and insurance Explanation of Benefits statements come in has been entertaining. Although it’s been more than four months and she’s 90 percent back to normal activities, the surgeon still hasn’t billed her. The hospital sent her a mysterious refund check with no explanation even though her insurance statement indicated that she actually owed money. Given the slim margins that some of us operate on, it surprises me that anyone would leave money on the table.
The DME vendor has double billed her and two other vendors have failed to submit to insurance prior to billing her. The only vendor that seems to have its act together is the physical therapy provider. The bills arrive monthly and are detailed and accurate. Even though I’m in healthcare and understand the markups, the actual dollar amounts are pretty amazing. Overall she was billed more than $45,000 and insurance has adjusted off about 75 percent of that. She’s got tremendous insurance, so her out-of-pocket cost has been manageable. Not being in healthcare, I’m pretty sure she has decided that our entire industry is simply crazy.
PricewaterhouseCoopers (you have to love the arrangement of that name) is projecting a potential increase in healthcare costs. The cost of security for electronic systems is cited as a factor, along with new and expensive specialty drugs hitting the market. Increasing employment of physicians by hospitals is also cited, particularly with the practice of billing out physician office visits with a hospital facility charge. Team-based care is predicted to help lower or stabilize spending. Not surprisingly, they predict that patients with high-deductible plans will be more cost conscious. It will be interesting to see what the data shows in five years and whether patients who forego medical services due to high deductibles end up having larger expenditures as conditions are left underdiagnosed or undertreated. The proliferation of such plans feels a bit like an experiment being conducted on people without the benefit of an institutional review board to protect them.
What do you think about healthcare spending trends? Email me.

Email Dr. Jayne.



I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…