There was a time when my company went through multiple rebrands. These were relatively minor shifts, but completely unnecessary. It…
News 3/26/14
Top News
The GAO looks at HIE efforts in four states and finds a lack of sufficient health data standards, variations in privacy rules across states, difficulties matching patient records, and concerns over covering exchange costs. GAO recommends that CMS and the ONC develop and prioritize specific actions to advance HIE and develop milestones with time frames to gauge progress.
Reader Comments
From The Reverend: “Exemption letter. A little mentioned part of the exemption that was offered up as “Vendor Certification Issues” for Meaningful Use 2 is that it requires the vendor to provide the EP with a letter. There is no guidance on what the letter must contain, who it needs to come from (vendor CEO, sales person, tier I tech support), or how to attach it to the exemption itself, but it a required (marked with a *) part of the exemption. The exemption also requires the EP to list the exact version they are currently running…which is obviously not the 2014 certified version (*because if it was, we wouldn’t be applying for the extension.) I am quite certain I am not the only concerned/confused person about this. It sure seems like it may be hard to extract this ‘letter of shame’ from the vendor. Can you help me?” If anyone can offer The Reverend some advice, please share.
HIStalk Announcements and Requests
![]() Mr. H is taking the night off, hopefully doing something fun, meaning I’m flying solo. Thanks for reading.
Mr. H is taking the night off, hopefully doing something fun, meaning I’m flying solo. Thanks for reading.
Upcoming Webinars
April 2 (Wednesday) 1:00 ET. A Landmark 12-Point Review of Population Health Management Companies. Sponsored by Health Catalyst. Presenter: Dale Sanders, SVP, Health Catalyst. Learn the 12 criteria that a health system should use to evaluate population health vendors and to plot its internal strategy, then see the results of grading seven top PHM vendors against these criteria. No single vendor can meet all PHM needs. The most important of the 12 criteria over the next three years will be precise patient registries, patient-provider attribution, and precise numerators in patient registries.
Acquisitions, Funding, Business, and Stock
Healthcare data analytics firm IMS Health expects to set its IPO price at $18 to $21 a share, giving the company a valuation of up to $6.97 billion.
Cloud storage provider Box looks to raise $250 million in an IPO. For the year ending January 31 Box reported revenue of $124.2 million with losses of $168.6 million.
Sales
Prime Healthcare Services’ Roxborough Memorial Hospital (PA) selects Wellsoft EDIS.
Baptist Health Care (FL) signs a multi-year agreement with MedAssets for multiple cost management and operational efficiency solutions.
People
Physician connectivity platform provider Updox hires Pat Bickley (Health Care DataWorks) to lead product management.
Xerox names Robert Zapfel (IBM) president of Xerox Services, replacing the retiring Lynn Blodgett.
Marc Krellenstein (Relay Technology Management) joins Decision Resources Group as SVP/CTO.
Health Revenue Assurance Holdings appoints Dennis Veasman (MModal) SVP of business development and sales.
Announcements and Implementations
Aprima Medical and Etransmedia announce an upgrade program for Etransmedia customers using the Allscripts MyWay platform. Etransmedia customers, which include providers that purchased MyWay through Costco, have the option to become an Aprima client, or, to use the Aprima system but remain a hosted client of Etransmedia. Both options provide current Etransmedia customers with one free Aprima licenses for each existing MyWay license.
ProHealth (WI) utilizes consulting services from Perficient to become the first healthcare system to produce reports and data out of Epic’s Cogito data warehouse in a production environment.
St. Francis Health System (OK) will go live across its 70 physician offices in May and at its hospitals in June.
The Robert Wood Johnson Foundation launches Flip The Clinic, an initiative meant to transform the average doctor visit to be more satisfying. The idea is to have the Flip The Clinic website serve as a hub for patients, providers, and other stakeholders to share ideas for improving the physician visit experience so that it’s more satisfying for patients and optimizes physician expertise. After reading Dr. Jayne’s latest Curbside Consult I’m hoping she will evaluate the site and share her opinions.
The South West Alliance of Rural Health’s Portland Hospital (AU) implements TrakCare Medication Management from InterSystems.
Government and Politics
Provider uncertainty is slowing implementation of the Designated Test EHR Program according to a representative from Meditech, which is one of three companies serving as test vendors. The ONC admits receiving a “decent amount” of questions on the program and says documentation is being developed to guide providers. Meanwhile, John Valutkevich, Meditech’s manager of interoperability initiatives notes that the ONC information already exists but many physicians and staff “don’t even know where to start.” I did a quick surf of the both the CMS and HealthIT.gov websites and I wasn’t able to locate relevant details, so I’m not surprised that providers are confused. Not for the first time I’m left to conclude that CMS and the ONC have plenty of “opportunities” to improve navigation on their sites.
HHS announces it strategic plan for 2014-2018 which includes an objective to meaningfully use HIT to improve healthcare and population health. Some of the noted HHS-supported initiatives include the promotion of HIT and standards through the MU programs; support for remote patient monitoring and telemedicine technologies; and promotion for programs such as Blue Button to engage and empower patients.
Massachusetts eHealth Collaborative CEO Micky Tripathi tells participants at a Federal Trade Commission workshop that HIT and HIE are “beginning to take off” now that the market is better rewarded for their adoption. He also warns that the industry is now seeing “a lot of tension” over the appropriate role of government in Stage 2 and Stage 3. I don’t know the full context of Tripathi’s statement but it seems the “tension” is less about the government’s role and more about what objectives and measures should be included and what tweaks should be made to the timing of the program. After all, doesn’t the government’s “role” include “owner” of the MU program?
Innovation and Research
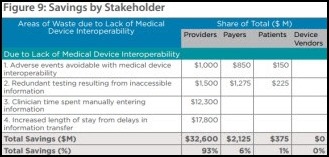
Analysis by West Health Institute finds that widespread medical device interoperability could eliminate $36 billion in waste in the health care system and increase clinician efficiencies. Direct cost savings could be driven by avoiding redundant testing and reducing adverse events.
Other
EHR usage in small physician offices has helped spur overall EHR adoption to 61 percent, according to an SK&A report on physician office EHR use.
Disturbing: a Topeka, KS man opens a dumpster in his office complex and finds discarded medical records, complete with patient names and social security numbers. Perhaps not coincidentally a document scanning service also has an office in the same complex. The state attorney general’s office have removed the charts for further investigation.
The Federation of State Medical Boards consider a telemedicine policy that would require physicians to be licensed in the state where the patient is located and would require the same standards of care for both virtual and face-to-face encounters. Opponents of the proposal believe the licensing requirement creates an unnecessary barrier to telehealth expansion and adoption.
Scientists from Johns Hopkins University (MD) and George Washington University (DC) claim their flu tracking method using Twitter was 93 percent accurate during the last flu season when compared to CDC-collected data. Google’s Flu Trend tool was recently criticized for overestimating flu prevalence by more than 50 percent.
Some features of EMRs are unintentionally contributing to patient harm according to the recently released Maryland Hospital Patient Safety Program Annual Report. The report notes that the Office of Health Care Quality “received numerous reports of adverse events in which IT system omissions or glitches contributed to adverse events.”
Sponsor Updates
- Healthx will add InstaMed Member Payments to its member portal solution.
- Madison Magazine names Vonlay to its list of best places to work in technology for employers with over 100 employees.
- CareVia will integrate its remote patient monitoring capability with the Harris FusionRX healthcare integration platform.
- Surescripts awards e-MDs its White Coat of Quality award for applying best practices to the use of e-prescribing technology.
- PatientPoint will deliver its population health management solutions with HealthTronics IT solutions for urologists.
- Consulting Magazine names Akhila Skiftenes of Aspen Advisors and Ryan Uteg of Impact Advisors to its list of 35 Rising Star consultants under the age of 35.
- Vecna, a provider of patient self-service solutions, will add Fujitsu’s PalmSecure technology to Vecna’s On-Site Registration solution.
- TriZetto recommends that organizations identify the top ICD-9 codes used in their highest dollar claims to reduce claim rejections after the ICD-10 transition.
- Health Catalyst profiles Texas Children’s Hospital and how the organization used Health Catalyst’s late-binding Enterprise Data Warehouse and analytics apps in its Pediatric Radiology department to improve patient care and achieve $400,000 in savings.
- Health Catalyst hosts a two-day Healthcare Analytics Summit September 24-25 in Salt Lake City.
- Dallas Business Journal names MedAssets to its list of 2014 Healthiest Employers.
- CareTech Solutions serves as a technology sponsor for IABC Detroit’s Renaissance Awards, which honor the best in business communication in Southeast Michigan.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis, Lorre
More news: HIStalk Practice, HIStalk Connect.
















A word to the good Reverend.
You got it right. The vendor has to acknowledge there was a problem with either delivering the software, or if 2014 certified software was delivered…somehow it did not work as certified.
I cannot imagine a vendor writing such a letter keeping in mind that ONC has appointed the Accreditation Agency (ANSI) to conduct surveillance on vendors and ATLs. And it all becomes public information. If a vendor admits failure after they received a 2014 Certification, then the AA would issue a notice of investigation and temporarily pull the 2014 certification for that vendor. About as close to a kiss of death any vendor could have. The vendors first line of defense will be to claim the user did not properly install or run the system, then you would have to respond, and round and round you go..while ONC pulls your bonus money back.
Good luck in getting a letter…might want to first start with a good legal advisor and you better have contemporaneous documentation available. If there was ever a case to be made for regulation generating work for lawyers…this has got to be it.
On the other side, if your vendor did not /could not deliver a 2014 certified system, which means it did not pass privacy and security criteria, and therefore could not be considered HIPAA compliant – OCR’s instructions are crystal clear – FIND ANOTHER VENDOR!
So the transition to ICD-10 goes for voting: House tomorrow and Senate on Monday.
See Section 212:
http://docs.house.gov/billsthisweek/20140324/BILLS-113hrSGR-sus.pdf
What do you think are the chances ICD-10 will be postponed again ?
The chances of another postponement are high, but it should not be, as the delay will only further confuse the issue with ICD-11 on the horizon. ICD-11-CM will not be comparable going forward from here with ICD-9-CM! Let your Representatives and Senators know that a further delay of ICD-10 is vote against patients!