Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…
News 8/9/13
Top News
Allscripts reports Q2 results: revenue down 7 percent, adjusted EPS $0.05 vs. $0.16, missing earnings expectations of $0.10. Revenue of $345 million missed expectations of $357 million. Shares are down 6 percent in after-hours trading. It’s the third straight quarter that MDRX has fallen short of expected profit. The announcement’s headline is a clear signal of a bad quarter given that neither revenue nor earnings are mentioned, indicating that the company was forced to dive deeper into the financials to find something to brag about. Allscripts is moving its focus (or at least the attention of analysts) to population health management given the minimal mention of its ambulatory solutions. I tried to listen to the conference call, but felt cognitive dissonance as the optimism I heard didn’t match the pessimism the numbers suggest.
From Fraudbuster: “Re: Farid Fata, MD. Charged with Medicare fraud. He is affiliated with Crittenton Hospital in Rochester, MI and its cancer center. It’s big news in the Detroit metro.” Federal agents arrested the doctor at his practice Tuesday, charging him with a $35 million Medicare fraud scheme that included administering chemotherapy and PET scans to cancer patients who had no chance of survival. He is accused of employing hundreds of unlicensed doctors trained outside the US to see patients first so he could visit with 50-70 patients per day and bill Medicare for his time, which totaled $25 million plus another $24 million in drug infusions, making him #1 in Michigan. He’s also accused of taking home bags of patient records to do billing from his home. The complaint says that in one case, the doctor insisted that a male patient who had fallen and struck his head on the way to the clinic be given his chemo before being taken to the ED, where he later died of the head injury. You might think CMS suspicion might have been raised earlier(and payments frozen) by doctor billing $25 million.
From Bob: “Re: McKesson Horizon. My hospital is looking to migrate to Paragon. Can anyone share insight?” If your hospital has done the conversion or is underway, please leave a comment.
From DCInternRoomate: “Re: ONC-funded HIEs. They are failing, so expect a huge Blue Button push next week.” I’m assuming you are saying that HIEs have had minimal impact, so patients will be reenlisted as the hand-carrying human interfaces between non-interoperable systems. I wouldn’t necessarily disagree. Technology bears some of the blame for mandatory sneakernet, but mostly it’s the screwy US health system that created the problems involved with expecting competitors to freely share information, not to mention to disenfranchise the patient to the point where they are merely the widget that must be processed in order to trigger sending out a bill. Medicare in the 1960s made healthcare a business and not a charitable endeavor or a public health project as it simultaneous drove (short term) and drained (long term) the US economy, so it’s hard to work corporate empathy and compassion in there. Hospitals have generally good intentions but poor execution.

From Velvet Hammer: “Re: HCA. This e-mail should give you an idea about HCA’s EMR plans.” The e-mail describes plans for HCA and Reston Hospital Center to roll out Meditech Advanced Clinicals, which would suggest that perhaps HCA won’t abandon Meditech for Epic or Cerner after all.
From MyFirstTime: “Re: [vendor’s name omitted]. I called them to learn more, but they say they are getting so many calls that they have started a wait list for new customers. Is healthcare IT so popular that it is now mainstream?” I can’t imagine that a lab ordering and results solution is creating such demand no matter how good it is, but readers have reported that it’s the real deal. I’m not mentioning the name again because this comment smells a bit like a company planted item, having originated in the same location as the company’s headquarters.
From Gordian Knot: “Re: Halamka’s recent self-indulgent blog post about benefits of keeping his organization homegrown. First, I really, really wonder what the cost analysis is when sites need to meet current regs. Second, I do find it humorous how other bloggers and semi-news sources immediately linked his comments with Maine Med having issues with an install of Epic. It all sounded like voices that have been waiting to jump on anything negative about Epic. How many people in leadership got ejected because of an install gone bad with Allscripts or Cerner or Siemens any other system? Look at Lahey and UCSF as extremes of installs gone bad. Since Epic is just about the only one installing anything, a few missteps gonna happen.” I used to advocate homegrown software, but those days were gone once the federal government started setting the development agenda. It’s ironic that hospitals that outsource activities such as food service, ED coverage, and even clinical departments assume that they are better enterprise software developers than companies whose own core mission is exactly that. Sometimes organizations really do have expertise and processes that preclude using commercial software effectively, but usually they just overestimate their wonderfulness. Those big hospital systems that like developing their own systems (not BIDMC specifically – I ‘m generalizing now) often have the money to run huge IT departments because they’ve created a lofty-brand pricing monopoly rather than because they have the highest efficiency or best outcomes, and with reimbursement changes, they will just keep buying up practices and hospitals and spreading mediocrity.
HIStalk Announcements and Requests
![]() From HIStalk Practice this week: 80 percent of clinicians use smartphones and almost half of physicians use a combination of smartphones, tablets, and laptops / desktops for professional work. Patients using EMRs through online portals express significantly higher satisfaction with their physicians and believe they are receiving better care. The AMA says CMS still has more work to do on the Medicare Physician Compare website. A reader reports on Aprima’s national user conference. A Colorado orthopedic clinic fires an employee who emailed PHI to her personal email in order to do some work from home. August is “Admit You’re Happy Month” which seems like the perfect reason to admit you’d love to make me happy by signing up for HIStalk Practice email updates. Thanks for reading.
From HIStalk Practice this week: 80 percent of clinicians use smartphones and almost half of physicians use a combination of smartphones, tablets, and laptops / desktops for professional work. Patients using EMRs through online portals express significantly higher satisfaction with their physicians and believe they are receiving better care. The AMA says CMS still has more work to do on the Medicare Physician Compare website. A reader reports on Aprima’s national user conference. A Colorado orthopedic clinic fires an employee who emailed PHI to her personal email in order to do some work from home. August is “Admit You’re Happy Month” which seems like the perfect reason to admit you’d love to make me happy by signing up for HIStalk Practice email updates. Thanks for reading.
Some recent HIStalk Connect posts worth your time:
Epocrates Mobile Trends 2013
HIStalk Connect Interviews Joe Reinardy, Founder and CEO, CenterX
Battle of the App Stores: athena vs. Greenway
Listening: Built to Spill, Idaho-based catchy guitar indie rockers that hit their popularity peak in the late 1990s that I’ve somehow missed until now. They’re on tour and I’m likely to check them out.
Welcome to new HIStalk Platinum Sponsor Valence Health, which offers providers turnkey solutions for delivering value-based care. The Chicago-based company has been doing that for 20 years and serves 35,000 physicians, 115 hospitals, and 15 million patients. Customers include Cleveland Clinic, Scott & White, OhioHealth, and half of the country’s freestanding children’s hospitals. Hospital solutions include clinical integration, population health, care management, analytics, managed services, physician network development, and financial analysis of value-based arrangements. Its Vision platform combines data from practice-based PM/EMRs, standardizes it with other data (hospital bills, labs, PBMs, LTC, payer), runs it through a proprietary EMPI, and then generates reports and analytics that measure quality, cost, and utilization and provides risk scores, identification of high-risk patients, and information to establish programs for specific populations and conditions. Its vMine technology obtains daily data from all certified PM/EMR systems and takes only 30 minutes to install remotely. Thanks to Valence Health for supporting HIStalk.
HIStalk Webinar
Elsevier will present “Invigorate Order Set Management: Four Essential Steps” on Tuesday, August 27 from 12:00 – 12:45 p.m. Eastern. Presenters will be Jim Nolin, MD, editor in chief for order sets at Elsevier, and Kevin W. Hatton, MD, medical director of clinical decision support at University of Kentucky HealthCare.
Acquisitions, Funding, Business, and Stock
LifeNexus, which offers a personalized health information smart card, raises $3.7 million from unnamed investors. Smart cards have been a solution looking for a healthcare problem for at least 20 years and almost always fail miserably, even when packaged as a hospital loyalty card.
Could computing vendor ClearDATA secures $7 million in second-round funding from Excel Venture Management and Norwest Venture Partners.
SEC filings indicate that activist investor Carl Icahn has increased his stake in Nuance from the 9.3 percent of the company’s shares he reported in April to 16 percent now.
Sales
Geisinger Health System selects VisiQuate to develop predictive revenue cycle analytics to increase efficiencies and lower collection costs.
Boulder Community Hospital Physician Clinics select Wellcentive’s Advance platform to facilitate care coordination in support of its PCMH implementation and as part of its comprehensive primary care initiative.
Twenty-four bed Cozby-Germany Hospital (TX) will implement RazorInsights ONE-Enterprise Edition.
People

Chris Belmont (Ochsner Health System) will be named as VP/CIO of The University of Texas MD Anderson Cancer Center (TX). I interviewed him in February.
Announcements and Implementations
St. Louis Children’s Hospital (MO) goes live on iMDsoft’s MetaVision for perioperative.
The Medical Center of Central Georgia (GA) implements Cerner CPOE with assistance from HCI Group.
The Baylor Quality Alliance ACO (TX) will expand its private HIE into a community HIE using technology from Sandlot Solutions.
Quantros will announce Friday that more than 1,500 Target stores and 50 Target clinics will implement its Safety Rx medication incident reporting system.
Texas Health Harris Methodist Hospital Hurst-Euless-Bedford, which surely must possess the longest and least-pronounceable hospital name in America, goes live on PCCI’s Pieces EMR-driven clinical surveillance and risk scoring system. PCCI is Parkland Center for Clinical Innovation, launched by Dallas-based Parkland Health & Hospital System in October 2012. Meanwhile, Parkland Memorial Hospital was finally deemed safe by CMS on Wednesday, which threatened in 2011 to cut off the hospital’s Medicare and Medicaid funding because of patient safety issues. The federal government said then that Parkland’s problems posed “an immediate and serious threat to patient health and safety,” forcing the hospital to spend $75 million on changes in the past two years.
Lubbock, TX hospitals launch the Llano Estacado Access Partners HIE, with the $80K startup costs underwritten by University Medical Center and Covenant Health System.
Government and Politics
HHS releases a strategy for accelerating HIE in support of delivery and payment reform. Specific strategies and policies include:
- Developing regulations and guidance on existing programs to enable the secure portability of health information
- Advancing HIE among long-term, post-acute, behavioral health, and laboratory providers
- Developing standards, including an interoperability and certification road map and HIT standards for quality measurement and improvement
- Implementing incentive and reward-based policies to encourage providers to incrementally incremental adopt electronic HIE.
Innovation and Research
The Inova Translational Medicine Institute at Inova Fairfax Hospital (VA) and GNS Healthcare will develop and commercialize computer models for predicting risk of preterm live birth using next generation sequencing and EMR data.
Other
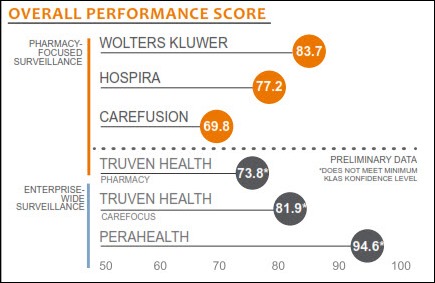
Seventy-nine percent of providers using clinical decision support surveillance software report that utilizing the technology has a moderate to significant impact on clinical outcomes, according to a KLAS report. Nearly all Epic, Hospira, and Wolters Kluwer users reported a moderate to significant impact on clinical outcomes, including reductions in length of stay, antibiotic usage, medication costs, and adverse reactions as well as better IV-to-PO conversions.
Highly rated with preliminary data in the KLAS report is PeraHealth, formerly Rothman Healthcare Corporation. I interviewed co-founder Michael Rothman in 2010 about what was then known as the Rothman Index, a real-time patient assessment and clinical decision support tool that readers found promising.
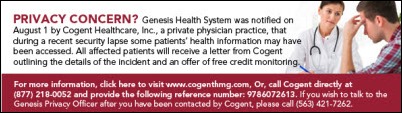
Genesis Health (IA) alerts several hundred patients that the transcription company used by Cogent Healthcare, its contract hospitalist provider, had exposed their information. It turns out it wasn’t just Genesis: Cogent now says India-based M2ComSys exposed information on 32,000 patients due to an incorrectly secured Web server. Cogent has since fired M2ComSys, which might have triggered confidence concerns initially given that all the photos on its home page still bear the stock photography watermark indicating that they apparently just stole the pictures instead of licensing them.
GlaxoSmithKline announces that packages of its vaccines will include two-dimension bar codes, which are smaller and can contain more information that linear bar codes. GSK will include lot number and expiration date so that hospitals and practices can log the information automatically in their EMRs.
Weird News Andy says he isn’t Captain Renault, but he is shocked – shocked – to read that CMS is months behind in testing data security for the health insurance exchanges that are supposed to be operational on October 1. CMS, having missed two June test dates, says it will instead test security on September 30, the day before the PPACA-mandated insurance exchanges are scheduled to be open for business.
Sponsor Updates
- Encore Health Resources announces that its Activation Support Services has supported 28 go-lives in 22 hospitals involving more than 10,000 physicians in the past 18 months. Chief Medical Officer Judi Binderman, MD will present EHR go-live challenges in an August 15 HIStalk Webinar, “Full Speed Ahead: Creating Go-Live Success.”
- Sharp HealthCare (CA) reports that its use of Caradigm’s Identity and Access Management suite has allowed it to grant system access requests in an average of one day compared to 21 days previously.
NextGen Healthcare reseller ITelagen introduces UroWorx, a series of urology-focused templates for use with NextGen Ambulatory EHR. - Imprivata announces that its OneSign solution is the most widely deployed SSO product at hospitals using Siemens Soarian Clinicals.
- CTG Health Solutions posts a white paper outlining the potential impact of big data on healthcare organizations.
- TrustHCS joins Greenway Medical’s online marketplace to offer PrimeSUITE customers access to its coding and ICD-10-readiness solutions.
- StrataRx releases details of its annual conference September 25-27 in Boston.
- iHT2 interviews Rick MacCornack, chief systems integration office for Northwest Physicians Networks (WA), who will be a featured speaker at iHT2’s August 21-22 HIT Summit in Seattle.
- Emdeon simplifies the new ACA operating rules and guidelines in its August newsletter.
EPtalk by Dr. Jayne
I can’t count the number of emails and text messages I received this week asking what I thought about Dr. Farzad Mostashari’s impending departure from ONC. Of all the names that are being thrown around as possible successors, none of them happen to share his impeccable taste in neckwear. I’m going to continue to appreciate each day that he remains on the job, although I suspect I will likely have to go into mourning when he leaves. I have a feeling we haven’t seen the end of his influence on health IT regardless of where he lands.
CMS issues a clarification on how multiple eligible professionals contributing to a patient portal may count a patient who views information. I’m glad they clarified that the patient does not have to specifically view information contributed by a particular provider for him/her to receive credit. Trying to track that level of data would truly be a chore.
Registration for ONC’s Third Annual Consumer Health IT Summit will begin on August 12. The event is September 16 and will include an announcement about a new eHealth campaign. How’s that for a teaser? The email from ONC was quite mysterious, and although it included a sentence missing the object of a preposition, it didn’t include a link to register or a specific website.
It may be old news, but I didn’t want to fail to mention the planned partnership to link LOINC and SNOMED. It should help with interoperability and hopefully will make things a little less difficult for those of us who have to hook everything up behind the scenes for hospitals and health systems.
Earlier this week one of my good friends mentioned he was frustrated with my health system’s lack of a patient portal. He can access the competitor’s portal but not ours and wanted to let me know. I was surprised since I helped install it almost four years ago. Turns out his physician is merely on staff at one of our hospitals rather than being employed by us, therefore uses a different EHR that may or may not have a portal live. We had a nice chat about the different kinds of community physicians and that their choice of EHR is largely determined by their employment status. It reminded me how obtuse the architecture of our healthcare delivery system is and how ridiculous it must seem to people working in more reasonably structured industries.
Pressure ulcers are a major problem in debilitated patients and ONC announced the winners of their mobile app challenge aimed at assisting nurses in documenting assessments and interventions for ulcer risk and prevention. The winning solution was WoundMAP PUMP from MobileHealthWare. It includes automatic graphing of wound size and time-lapse review of photos. The app is currently in beta testing.
I always like to hear about low-tech solutions and this story got my goat. Eco-Goats provides “environmentally friendly vegetation control,” which will be used at Washington’s Congressional Cemetery. Maybe I can get them to assist with my kudzu problem.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.














If HCA has chosen not to go with Epic or Cerner after an evaluation then does this mean “smart money” has voted with its feet and stayed with Meditech? Given Bain and KKR as key investors and a fairly sophisticated for profit focus I would guess there was a fairly through analysis of the long term costs and benefits done.
RE: Weird News Andy says he isn’t Captain Renault, but he is shocked – shocked – to read that CMS is months behind in testing data security for the health insurance exchanges that are supposed to be operational on October 1. CMS, having missed two June test dates, says it will instead test security on September 30, the day before the PPACA-mandated insurance exchanges are scheduled to be open for business.
Does anybody besides me find a bit of irony in the fact that the primary entity (CMS) telling the rest of us what we need to do and by when, is the least prepared for any parts they are responsible for, in making this happen?
I know, I know….there are many moving parts here, but would it make sense to not set a deadline until you know for sure you’re able to operationalize? There is a lot to be said for “under promise, over deliver!” I know, I’m feeling a little grouchy tonight.
HCA is known and self avowed to do the cheapest thing possible – always paying below market and comfortable trying to squeeze dimes above all.
Anyways, Meditech works and isn’t a bad solution for small hospitals or hospitals that operate independent of health systems.
I think we’ll see HCA vary their software based on market and need. They don’t really operate as a national system so different solutions at different times in different markets probably is a reasonable approach for them while they manage the costs.
His blog was self serving and self aggrandizing as it normally is. To expect anything different would be silly.
What John will come to grips with is that doing what others have done for a long, long, long time and doing it not quite as well as they do isn’t what most would call “innovative”.
The leading health systems are looking EMR companies to provide the block and tackling but to do so in a manner that they can innovate on top of that platform.
That’s where Epic seems to do a reasonably good job – they are an EMR and as well a platform for innovation. You might still complain that innovation is hard, but that’s the nature of it.
Even though John might go down with the sinking ship of self development and high costs of internal IT, the BIDMC might not. Lots changing in that market and although the BI can command a premium for medical groups on the outs with Partners, their day will come.
“Medicare in the 1960s made healthcare a business and not a charitable endeavor…”
What? There is a lot that’s wrong with Medicare, but it’s both historically inaccurate and naive to think that healthcare was not a business before the 1960s. Medicare based its benefits on the Blues.
It’s certainly true that healthcare has become more and more like just another profit-focused business and has lost some of the public service ethos that physicians and hospitals had in the first half of the century, but the big changes here didn’t occur until the 1980s. That’s when the outpatient bonanza began and America’s healthcare costs started to skyrocket above those for other nations. If you’re going to dramatically oversimplify the blame, blame Reagan and the pursuit of self-interest over the common good. I may sound ideological here, but just look at the numbers for when America started becoming uniquely messed up with respect to health care expenses. It’s 1980, not 1963.
Medicare absolutely enabled this, but so did commercial insurance and, clearly, the mindset of the American people.
I am the Clinical Informatics Manager for a ~300 bed, multi-facility hospital system in the northwest that is converting from McKesson Horizon to Paragon in 17 days. I would be happy to entertain any questions you may have about our decision and progress. bob.cutter@yahoo.com
“Since Epic is just about the only one installing anything”
oh, really?
I agree with HCA and Money’s statement. The Epic pilot in Salt Lake was simply a ploy to place serious downward price pressure on Meditech. Think Wal-Mart like tactics here.
I’m curious about this statement: “Medicare in the 1960s made healthcare a business and not a charitable endeavor or a public health project as it simultaneous drove (short term) and drained (long term) the US economy, so it’s hard to work corporate empathy and compassion in there. Hospitals have generally good intentions but poor execution.” An interesting and, to me anyway, unfamiliar perspective. How do you reconcile this with the blizzard of recent news articles on the vagaries of pricing among hospitals? And what’s the solution? Going all free market or all master plan, as the hybrid is killing us?
Easy to be judgmental about a greedy doctor fleecing the government. I don’t know the guy, maybe he’s a crook after all. From looking at the info above, it just seems like he’s harder working and more efficient than other doctors. If he worked for a big corporation, he’d probably get a bonus and a raise. Would rather see the evidence than assume that just because he made a lot of money and CMS paints him as a criminal that he actually is. Anyone who has worked in health care long enough to see one of these fraud investigations up close and personal knows that they’re rarely as clear cut as the press releases sound.
Your webinar by Elsevier sounds interesting: “Presented by Elsevier. Order sets have moved to the top of the C-suite agenda. Hospitals and health systems that previously developed order sets are now under pressure to keep them updated with current…..”
U Kentucky Health was a beta test site for Elsevier’s CPOE order sets as stated by their CMIO Steltenkamp in “Information Week” a bit back. She stated that they had innumerable redundant order sets that accumulated over the years.
I wonder how they were monitoring the outcomes of these beta experiemnts.
Folks,
There is no innovation in HCIT.
There is no Apple because there are no Steve Jobs.
It is what it is.
Built to Spill’s “You in Reverse” is a go-to choice for me when listening to music to drown out the low-wall-cubicle people noise
Enough with the Epic evangelists! It is an excellent EMR, but the unquestioning idol worship is nauseating.
Ask Farzad, on the way out, where he witnessed the most innovative and effective use of a commercial EMR to drive patient outcomes and it was not an Epic site.
@The Other Side — If Dr. Fata wasn’t robbing CMS, then he was robbing his patients by spending such little time with them. I hope CMS takes a look at other highest billing doctors as well.