Anything related to defense will need to go to Genesis.
News 8/28/09
CEO donates $1 billion to create “Bell Labs of healthcare”
Investors seek HIT companies that improve provider cash flow
Organizations partner to create next-generation LIS
From Roger Murdock: “Can you figure out a way to shake the truth out of HIT vendors and consultants? It seems to me that sales and acquisitions of anything HIT have really stalled since the beginning of the year. What do you think? I know vendors are reluctant to say anything other than ‘Sales are through the roof!’, but I don’t think so.” I don’t think so either, in most cases. Some companies, especially those with big market share and some diversification, are doing OK. Most, I’m guessing, are limping along as meaningful use uncertainty and capital constraints keep customers on the sidelines, at least for now. I think you’ll see the rich and the best get richer, while those with mediocre leadership, uninspiring products, and a shrinking war chest will find it hard to keep the vampires away until daylight finally comes. Vendors, please leave a comment (anonymous is OK) about your experience – is it boom times, so-so, or bust?
From Vilma Banky: “Re: MUSC. Funny, but I can remember community hospitals and vendor executives saying that they didn’t need anything that one of those big tertiary care or academic hospitals might need. MUSC provides care across a wide spectrum of patients in the Charleston area. I just can’t imagine them not needing everything for clinical documentation or medication administration. There are relatively standard charting requirement or needs (as well as medication administration needs).” I think Frank was saying that he doesn’t necessarily want it all from a single vendor. I’ve interviewed him twice and I really like him, by the way. I can never tell how someone comes across in the written interview transcript, but I can tell you that he impresses me as honest, sincere, and respectful.
From The PACS Designer: “Re: another WebOS. WebOS platforms are gaining more popularity, and this month SourceForge has named eyeOS as project of the month. The eyeOS application was created in Spain and is an open source Web desktop that would be good for testing potential cloud applications.”
From Seeking Truth: “Re: Cigna’s decision to stop receiving electronic claims via the Emdeon clearinghouse. The battle is presumably over the fees Emdeon charges payers to receive electronic claims. Cigna doesn’t want to pay and Emdeon doesn’t want to offer a lower price. Emdeon and Cigna may resolve this price battle, or alternatively, Emdeon may ‘reclassify’ the payer as ‘non-participating’ payer (similar to Medicare and Medicaid, which are prevented from paying clearinghouse fees). This reclassification may allow Emdeon to charge providers a higher per claim charge per their contract terms with the provider. The Cigna e-mail indicates other options available to providers, but those options require a vendor change, which may involve other costs to the provider community. Obviously, the healthcare industry is being hammered to ‘reduce costs’ and this may be a payer response to that pressure. As a publically traded company, Emdeon will try to preserve their revenue, though clearinghouse charges may be difficult to justify. Since the advent of HIPAA Title II – Transactions and Code Sets (TCS), clearinghouses have had growing difficulty justifying transaction charges incurred by both providers and payers (consider how many ownership changes for Emdeon, NDC Health, Per Se’ and other clearinghouse vendors since 2002). The upcoming ANSI 5010 conversion may also influence how payers and providers exchange transactions. Dare I say, ‘never a dull moment in healthcare EDI.’”

From Ex-Cerner Guy: “Re: Waterbury to Meditech. Waterbury hosts site visits and reference calls for Cerner and WH Clinicians are happy. Could be for Patient Financials / Rev Cycle, but even then, I doubt it.” Me too. A reader’s got a line on a source there who may give us the real scoop, which I’m betting is no scoop since I doubt they’re switching.
From A Fan: “Re: vendor disclosure. We’re coming at it from the wrong angle. The real issue here is not what your vendor is preventing you from disclosing, but rather what your vendor discloses to you (whether or not it came from another client). The other thing I wonder is, of the issues that are reported to someone like Dr. Koppel, how many make it to the vendor? There’s no question vendors gear development towards sales, but as we all know, health care has arguably as much bureaucracy as government and the feedback loop from real users to vendors is not great.” I know my vendor doesn’t seem to care much about issues we report, even those with patient safety implications. Their excuse always is: (a) it’s working like we designed it, as suckily as that might well be; (b) nobody else has reported it, so it can’t be much of a problem; (c) you’re doing weird stuff, so stop it; (d) we begrudgingly acknowledge that it’s a problem, but we plan to give you an unrealistic workaround and mark it as a future development project until you simply wear down; and (e) it will take at least a year to get a quick fix into your hands, so that automatically makes it unimportant since you’re stuck with it until then. I’ll also say that none of my vendors have ever been very good at proactively letting customers know about issues reported by others, meaning you go through a ton of testing and documentation to place the neatly tied package into their laps only to be told they already knew about the problem. If your vendor is better than mine, tell me.
All Children’s Hospital (FL)will open its new building in December (a very cool set of daily construction pictures is here – check out the Time Lapse option) and will use the Pediatric Edition of the Patient Life System by GetWellNetwork.
SNOMED Terminology Solutions is offering a free course by teleconference, SNOMED Clinical Terms Basics. New courses offered: Introduction to Terminology and Classifications and Introduction to Mapping.
I’m guesting (is that a word?) at Inside Healthcare Computing with an editorial called Lessons from Shark Tank — Beware of Vendors Borrowing Money or Going Public, where I drew my inspiration from (what else?) a TV show. Here’s a snip: “It also makes me wonder how many dull, average companies got that way because they took someone’s cash, put the founders out to pasture, and set all the fun, smart ideas aside and turned themselves into a bad mutual fund run by second-tier MBA school graduates.” I also worked in a fun reference to, as I call him, Dead Billy Mays.
I guess a wheezing economy has led us to this TV news headline, which refers to temporary jobs at a McKesson H1N1 vaccine center: Swine Flu Brings Jobs to West Sacramento.
Sunquest, Mass General, and Partners will jointly develop a new generation of LIS that focuses on anatomic and clinical pathology. I’ve said for years that if you want to see inarguable success in getting benefits from IT, find yourself some lab people. It’s no accident that the first really useful and clinically-focused hospital systems were LISs, back in the day when “nursing systems” meant online requisitions (aka, “order communication”). The most advanced automation of its kind is in the big reference labs, where you see a lot of computers and not so many people handling pipettes and swabbing agar plates. Instead of complaining about automation, laboratorians embraced it, designed it, extended it (rules capability, standard interfaces, repositories, barcoding, digital imaging, FDA-regulated instrument interfaces, portable data collection, RFID), and are now on the cutting edge of genomics, clinical alerting, and data warehousing. Among all providers and ancillary departments in hospitals, labs are about the only ones that we don’t have to be embarrassed by when talking to people from other sectors that are decades ahead of healthcare. The MGH pathology informatics doc said that tomorrow’s labs will “utilize advanced diagnostic and information management technologies, such as digital pathology, molecular studies, business intelligence and service-oriented architectures to simplify and strengthen the informatics infrastructure.” That ball you saw going over the Green Monster was Sunquest smacking one out of the park in a blockbuster boost to the company.
You know when a press release says somebody “applauds” some government action, they’re smelling cash. The HIMSS Electronic Health Record Association “responded with enthusiasm” (salivation) to Uncle Sam’s decision to donate $1.2 billion in freshly printed and rapidly devaluing currency to pay for the software its members sell. According to the “About” section, membership is open only to HIMSS Corporate Members. Should a non-profit, advocacy-heavy member organization like HIMSS really be running a vendor trade group while claiming to be impartial and patient-centered? As a provider, should I be paying dues to an organization that sells my information to vendors (mailing lists, HIMSS Analytics survey results, conference information), organizes those vendors to influence government policy, and runs Webinars and sales pitches on their behalf that are aimed at getting us poor provider members to buy stuff from its far more lucrative vendor members? It’s Ladies’ Night – I’m getting cheap drinks, but only if I can stand being constantly groped by those paying full price for that privilege.
Peace Health expects to get $30 million from HITECH.
This is one of those times where I say that I’m a bit behind despite working absurd hours, so if you’ve e-mailed me about something lately, be patient – I read every e-mail and respond appropriately, but it might be a bit slow in coming (working two full-time jobs is sometimes challenging).
Another vendor heard from who does not put non-disclosure language in its contracts: Eclipsys. They join Meditech and Medsphere. So. what say you, Cerner, Epic, and McKesson?
Inga connected with one of our old pals at Noteworthy Medical Systems (they used to be a sponsor pre-CompuGroup) since a reader asked about the Cleveland office. She says it’s alive and well and nobody has moved to Phoenix, although all locations have had some restructuring.
If you don’t read HIStalk Practice, you missed this excellent piece, DrLyle’s Meaningful Discussion about Meaningful Use. Put your e-mail address on that page if you want updates when we write something new on HIStalk Practice – it has its own e-mail list separate from the HIStalk one. We have some fine sponsors, guest writers, and interviews there – like HIStalk, but more oriented toward physician practices.
Sparrow Hospital (MI) kicks off its EMR project.
A sweet deal for Misys PLC CEO Mike Lawrie: his contract requires him to be paid in dollars, so the significant drop in pound against the dollar didn’t cost him loss of several hundred thousand dollars of buying power. With a projected US 10-year deficit now up to $9 trillion, I don’t think he’ll have that problem for long.
In India, Apollo Group of Hospitals has started on its IBM-led “Health Superhighway” connectivity project. It’s also working on a unique ID number project. I’m pretty sure I’ve mentioned both before, but it’s still pretty cool.
A WSJ blog on venture capital says investors are looking for opportunity at the intersection of healthcare and IT (that’s us). It credits athenahealth and its $1.3 billion market cap for increasing investor interest, also juiced by HITECH headlines. As we’ve said here before, though, investors want companies that can improve the cash flow of providers, not those trying to sell a nice-to-have product.
Dayton Children’s (OH) goes live with its $27 million Epic project.
So why isn’t this making headlines? A drug company billionaire CEO/MD is donating $1 billion of the $3 billion he made from the sale of his company “to create the Bell Labs of healthcare”. Some quotes from him: “The idea is to create a health grid that empowers the patient and the provider. This should be a public utility, basically what I call a U.S. public health grid … The idea is to actually go across the country and bring scientists, mathematicians, computer scientists, engineers, biologists, clinicians, surgeons, oncologists, pathologists, all together. And really integrate, truly integrate, information from the basic science to the bench to the clinic … So I’ve started funding and bringing together computer scientist to implement the grid, in an open architecture for the country … We have now the opportunity to jump-start health care, straight into molecular world. Or having the integrated, open-source software system that allows access to the 200-300 Legacy systems of software. So my great concern is, if we go ahead and implement a plan that just says, ‘OK, everybody just has an electronic medical record, with 200 proprietary systems, that don’t talk to each other by its nature.’” This is truly amazing, fascinating, and inspiring all at once. If anyone has a connection, I’d like to interview this guy (maybe sucking up a little in a quest to become Official Blogger of the Bell Labs of Healthcare at a significant salary).
Everyone thinks Cache’ is a healthcare-only MUMPS thing, but here’s proof that they’re wrong: a private bank for rich people selects it to run its Web-based banking system.
HERtalk by Inga
Christiana Care Health System (DE) selects Patient Care Technology Systems’ Amelior Tracker system to automate the management and tracking of its hospital assets.
Five hundred doctors with Jefferson University Physicians (PA) will soon be live on Allscripts EHR.
The newly public Emdeon signs a 15-lease for a new data center in Nashville. Emdeon, whose IPO raised $367 million, will rent 34,200 square feet for $39,500 a month, making the lease value more than $8 million.
Thanks to Mike and those crazy guys at Compuware for sending over their latest Youtube creation. This Rockstar CIO interview is definitely worth a 41-second diversion. And since I was amused enough to watch it over and over, I’ll give the company a little pitch for a survey of hospital clinical system users they’re doing that should take about 60 seconds or less of your time.
Covenant Medical Center (IA) agrees to pay $4.5 million to settle alleged violations to the Stark Law and submitting false Medicare claims. The federal lawsuit claimed the hospital paid the five specialists “above fair market value” for their services at rates that were “commercially unreasonable.” The government claims the physicians, who referred patients to the hospital, were among the highest paid hospital-employed physicians in the entire country. Records show the doctors were each paid between $633,000 and $2.1 million.
A couple of traditional ambulatory vendors announce they are now offering HIE functionality. Greenway Medical introduces PrimeEnterprise, which enables a community of Greenway customers to share select clinical and financial data. Also, Rabbit Healthcare Systems implements the first phase of its HIE solution, going live with data exchange between McKesson’s Lynx Mobile Inventory Management System, GenPath Reference Lab, and Docuda’s ERCard patient product (it doesn’t sound like an HIE, but that’s what they say).
The Stevens Institute of Technology (NJ) plans to use a $2.8 million grant from HHS to create an electronic system to boost the care of women of color with HIV/AIDS.
The Northwest Pennsylvania AIDS Alliance was also a recipient of grant money to support their IT projects. The HRSA awarded the alliance $45,188, which will allow it to create a new computer network and permit real time access to the Lab Tracker database.
More consolidation in the medical transcription world: Transcend Services will pay $16.2 million in cash and stock to acquire Medical Dictation Services.
The National Quality Forum endorses 18 standards for measuring quality and safety metrics for over-the-counter and prescription medications.
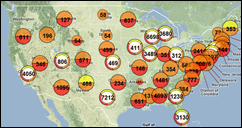
A friend was diagnosed with the H1N1 swine flu, which got me surfing a bit, just to assess the likelihood that I, too, might end up being bedridden. Fortunately my friend is now fine and I seemingly dodged the bullet. Anyway, I found this cool flu-tracker map that allows you to see the the number of suspected and confirmed cases in your community. Or, perhaps to figure out what vacation spots to avoid.
Another ex-hospital worker is arrested for allegedly stealing personal information from patients. The former Our Lady of the Lake Regional Medical Center (LA) employee opened 46 debit cards and filed fraudulent income tax returns. He also received $20,000 from fraudulent claims.
Researchers now believe that women with stronger thighs might be better protected from knee pain. Surely my thigh abundance is related to strength. Thus, I’m no longer going to obsess about the size of my thighs; rather, I’ll now be thankful that they are helping to preserve my articulatio genu.










re: Greenway and Rabbit – What is the benefit of an HIE that is limited to only the HIE vendor’s proprietary products? Certainly won’t help in any situation where the docs or facilities are using a disparate system. Good Lord, wake up, vendors! The intention of an HIE is not to simply connect YOUR products. The intention is to link systems no matter their origins or creators to improve healthcare globally. Greenway and Rabbit should be looking beyond padding their own pockets through inadequate sophomoric products and offer something truly valuable to patients, physicians and facilities. Come on, guys.
I have read with interest your one-on-one interviews. I am wondering if you have ever asked H. Stephen Lieber (HIMSS CEO) or Mark Leavitt (CCHIT Chair) for an interview? Your interviews are very fair. I would like to see a balanced interview on HIStalk, I’m sure other readers would like to see this too. Perhaps readers can send in their questions, and you can sort through them. There are so many unanswered questions I would like to finally have answered by Lieber and Leavitt. You know so much about their activities, I personally would like to know more. But please, don’t bring up the subject of cats and dogs! A solid Q&A would do just fine. Would they be willing to subject themselves to an interview? Would any former employees like equal time as well?
I am personally shocked they both made Modern Healthcare’s Top 100 list, even though they are further down the list than in the past. These are the people we can thank for leading our county into crisis and gross systemic failure, one of the most expensive, unsafe health care systems in the world. They do not put patient safety first, they put profits first. They are all millionaires living off the fat of tax-dodging non profits. This is an outrage! We taxpayers deserve answers.
If Mark and Steve are at the top of the list for health care, then how can they call themselves “nonprofits” when health care is a multi-trillion dollar a year industry and the U.S. has the most expensive, most profitable system in the world?
Wow, Mr. HIStalk…your comment about vendor disclosure by “A Fan” was right on! How is it that we have allowed this kind of behavior by the vendors? It’s time they start delivering software that is safe for patient care!!
FYI re: Patrick Soon-Shiong’s $1B for healthcare — I did not see a link; a solid resource about this appears to be the 8/25 Forbes article. http://www.forbes.com/2009/08/24/healthcare-obama-reform-business-billionaires-national.html
Cerner has NDAs in all its contract. They will not work with a client that disagrees with the NDA.
Is it just me, or is the idea of spending “only” a billion dollars to integrate every hospital in the nation not nearly enough? The IEEE (or one of the professional organizations, I’m not industrious enough to look it up) commissioned a study on “ultra-large systems”, the logical step up from VLSI (very large systems) where you’re dealing with BILLIONS of lines of code.
Billions of lines of code sounds outlandish, but if you add up all the customizations each hospital makes to its various HIS/CIS/LIS/RIS/PACS/HIT/whatever systems, and multiply that for each hospital (or hospital system, assuming they standardize)–customizations could well number in the billions.
And this is an honest question: am I missing something? Is there some automated way to understand the customizations deeply enough to map a lab result from any arbitrary system? I vaguely remember something from a previous HIStalk interview how a company was acting as a middleman with its canonical data format, but it’s not coming to me. Is integrating easier than I make it sound?
re: Roger Murdock
It’s a mystery to me why there is so much focus on HIT vendors regarding sales – boom or bust. Why aren’t you asking hospitals why their strategies for implementing advanced clinical information systems is based on ARRA/HITECH. Stimulus is not a strategy! Have we reduced the acquisition and implementation of CIS to a profit strategy? What happened to strategic thinking in hospitals? What happens if the stimulus money doesn’t materialize? The industry needs to quit focusing solely on stimulus monies as a rationalization for acquiring information systems.
The “truth” is many hospitals are indeed in a wait and see mode with respect to ARRA and “meaningful use”, but that doesn’t mean that every purchase falls under that type of scrutiny. When a server fails, the smart CIO doesn’t hold off on a replacement in order to wait and see if Obama will pay for it. Same goes for RAC, Data Security, Patient Safety, etc. etc. Established vendors offering a diverse product line are positioned to not only weather the storm, but emerge even stronger.
@p_anon – make that one billion and five (or so). I just got an e-mail that now they want those reports to print automatically every morning at 6. Don’t blame me…I just write the stuff.
“I know my vendor doesn’t seem to care much about issues we report, even those with patient safety implications. Their excuse always is: (a) it’s working like we designed it, as suckily as that might well be; ” Thank you Mr. Histalk.
This, my friends, is the reason they need the FDA to protect the safety of patients.
In aggreement with comments on an earlier blog, y’all call the FDA w your catastrophes, k?
Enjoyed the snippet of your editorial on IHC and share your fascination with the Shark Tank show. Not sure I want to spend $20 to read the rest of the story. As most small HIS shops will tell you these days, the sharks are not just on television!
I would be interested in seeing some examples of patient safety issues that vendors refused to fix.
Why doesn’t HIMSS get involved, regarding Patient Safety and nondisclosure clauses? If they really care about patient safety, and not the profits they generate for themselves and their EHRVA group, then they would reach out to help resolve this matter. They claim to be THE leader in HIT.
HIMSS can get their research arm, HIMSS Analytics, to conduct a survey with vendors from HIMSS other nonprofit org, EHRVA. FULL DISCLOSURE! Then present the data to HHS and CCHIT Board, to decide what to do with this information, force the vendors to comply with their ruling. The FDA is a great idea, but I remember reading Dr. Borges comment that he had already contacted FDA back in 2006 regarding the ceritifying body “CCHIT” and got no results from the FDA.
Write to the FDA and HHS. Let them know that this is a big issue of concern within the HIT community. I already did, and I hope others will join me.
To Michael Peters:
I think the Joint Commission will solve this problem. Want to pass Joint Commission inspections? Don’t buy medical devices whose defects you’ve agreed not to disclose.
The Joint Commission will have to do this, because with this knowledge in the public domain, if a patient is harmed or dies at a hospital that passed JC inspection, from a health care IT malfunction or defect that could have been prevented by knowledge sharing with some other hospital or the vendor itself, there really will be hell to pay from many quarters in the court room.
The vendors in their arrogance and hospital executives (such as CIO’s) in their naivete have painted themselves into a very, very unpleasant corner.
Re: Sunquest, Mass General, Partners – And, I’ve said for years that if you want to see success in getting benefits from medical device integration, find yourself some clinical lab people! After all, the clinical lab is a room(s) of stand-alone, proprietary medical devices / instruments. The fact that during the 1980s these folks figured out the rules, repositories, instrument interfaces, etc. (and are now looking at genomics, clinical alerting, data warehousing, etc.), makes me wonder why today we are having such a tough time doing same with the plethora of stand-alone, proprietary devices / instruments that beg to be integrated into our EHRs.
I took the SNOMED course this week. It is a worthwile introduction if you don’t know anything about standardization.
Thanks for the followup. I will look at the Joint Commission’s website. I do not believe HIMSS would take the initiative anyway, because of their close association with their own group, EHRVA, and H. Stephen Lieber’s role as CCHIT Trustee Chair. I was hoping HIMSS and CCHIT would take the lead and prove to the HIT industry that they actually care, that they are not in it just for the money.
It is well known in the HIT industry that Patient Safety issues do not come first for HIMSS or EHRVA. And Mark Leavitt, chair of CCHIT, answers to his boss, H. Stephen Lieber, who has paid his salary and healthcare benefits up to January 2009.
So until H. Stephen Lieber steps down as CCHIT Trustee Chair (and possibly steps down as HIMSS CEO) we should not expect change. Expect more of the same.
A National browser-based EHR has a propensity score for success as that antidotal carburetor that gets 100 miles per gallon. The healthcare industry would handle a national standard browser-based EHR solution that same way the oil industry terminates innovation for fuel economy; with extreme prejudice.