In fairness to the person on the thread the other day: Now THIS is politics on the blog. :)
News 7/20/12
WorldOne acquires the 130,000 physician-member Sermo, which adds to WorldOne’s global network of 1.7 million healthcare professionals across 80 countries.
Reader Comments
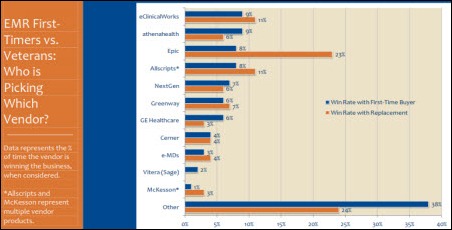
![]() From Simple Simon: “Re: ambulatory EMR satisfaction. First the CDC reports that 55% of US doctors are using some type of EHR and 85% of those claim to be somewhat or very satisfied with its day-to-day operations. Now KLAS says that 49% of practices with existing EHRs are considering replacing their systems. Somebody has to be wrong.” Perhaps, but keep in mind the sample sizes and methodologies were quite different. CDC’s findings are based on the results of a mail-in survey from 3,200 physicians. KLAS used a smaller sample of 302 practices. KLAS suggests that practice consolidation may be contributing to the high replacement figure as entities search for a single solution to replace disparate EHRs. In other words, a good number of providers may be perfectly happy with their EHR, even as the organization searches for a new system. As a whole, I think you can draw some broad conclusions that adoption is up, that support and product issues are creating discontent among some users, and that the replacement EHR market will continue to flourish. I am reminded of the advice that Mr. H regularly administers: be leery of the conclusions drawn by many of these surveys because methodology and biases sometimes make them questionable.
From Simple Simon: “Re: ambulatory EMR satisfaction. First the CDC reports that 55% of US doctors are using some type of EHR and 85% of those claim to be somewhat or very satisfied with its day-to-day operations. Now KLAS says that 49% of practices with existing EHRs are considering replacing their systems. Somebody has to be wrong.” Perhaps, but keep in mind the sample sizes and methodologies were quite different. CDC’s findings are based on the results of a mail-in survey from 3,200 physicians. KLAS used a smaller sample of 302 practices. KLAS suggests that practice consolidation may be contributing to the high replacement figure as entities search for a single solution to replace disparate EHRs. In other words, a good number of providers may be perfectly happy with their EHR, even as the organization searches for a new system. As a whole, I think you can draw some broad conclusions that adoption is up, that support and product issues are creating discontent among some users, and that the replacement EHR market will continue to flourish. I am reminded of the advice that Mr. H regularly administers: be leery of the conclusions drawn by many of these surveys because methodology and biases sometimes make them questionable.
From CDMer: “Re: DoD-VA Interagency Program Office. They’ve issued an RFI to survey the market for vendors who can meet the specs of the future iEHR that will allow them to replace AHLTA and VistA. It’s always nice to have 100-year goals!”
From Wurka Round: “Re: NYU Langone. Paper checklists are being deployed to keep results from being silo-bound in the ER.” The hospital, stung by media coverage of the death of a 12-year-old boy who was discharged from the ED despite available lab results showing significant infection, now requires ED employees to complete a pre-discharge checklist indicating that they have reviewed labs and vitals one last time. The hospital also says it will make sure that any post-discharge abnormal lab values are communicated to the referring physician, which also didn’t happen in the boy’s case.
From Clownface: “Re: Epic. What qualifies as an employee-owned company? In my training class, Epic says it’s employee owned, but SEC reporting of financial data is required for more than 500 shareholders and Epic does no reporting. With more than 5,000 employees, that means less than 10% of them are shareholders. How is that employee ownership? Does the CEO just have to be an employee to count?” Good question. From what I can tell, SEC requires detailed financial reporting for private companies exceeding $10 million in revenue and 500 shareholders. Meditech is a good example. I don’t see any Epic filings on EDGAR, but maybe they use a less-obvious name to avoid prying eyes. Or, you could be right that most employees will never get a shot at owning shares. Maybe someone who works there can enlighten us, although I’m not counting on that happening.
From Albert: “Re: UC Health, Cincinnati. Ambulatory applications went live in big bang fashion last week, replacing an extremely customized GE Centricity. Nearly 100 clinics and 3,000 users are up and running!” I believe they’re implementing Epic.
From MT Hammer: “Re: M*Modal. Nuance tried to buy them?” An interesting blog post makes a strong case that Nuance was the unidentified company that offered $17 a share for M*Modal in June, an offer that was rejected because the unnamed company had just purchased an M*Modal competitor (presumably Nuance’s acquisition of Transcend), leading to uncertainty about whether the deal would actually close due to antitrust issues. Quite a few folks (some of them working for securities class action law firms) say M*Modal sold out to JP Morgan Chase too cheaply, so they will undoubtedly point to this news to support their position.
HIStalk Announcements and Requests
![]() I am back from my semi-vacation and still busy cleaning out my inbox. If you haven’t had a chance to read the recent HIStalk Practice posts, here are a few goodies you might have missed. Highlights from KLAS’s recent report on ambulatory EHRs, including the most replaced and most considered vendors. NCQA extends a “Distinction” designation to 60 PCMH primary care practices. Greenway publishes a cool infographic that overviews the MU process. MGMA’s tips for practices considering a social media presence. New payment methodologies may have helped primary care physicians increase their 2011 compensation by more than five percent. Aaron Berdofe discusses health record banks in the third part of his series on healthcare infrastructure data models. Dr. Gregg explains the commonality of clubbing, EHRs, and religion. Brad Boyd of Culbert Healthcare Solutions highlights the great promise of centralizing patient access and revenue cycle. Take a moment to cool yourself from the summer’s heat with HIStalk Practice’s refreshing ambulatory HIT news. Sign up for the e-mail updates while you are there. And, thanks for reading.
I am back from my semi-vacation and still busy cleaning out my inbox. If you haven’t had a chance to read the recent HIStalk Practice posts, here are a few goodies you might have missed. Highlights from KLAS’s recent report on ambulatory EHRs, including the most replaced and most considered vendors. NCQA extends a “Distinction” designation to 60 PCMH primary care practices. Greenway publishes a cool infographic that overviews the MU process. MGMA’s tips for practices considering a social media presence. New payment methodologies may have helped primary care physicians increase their 2011 compensation by more than five percent. Aaron Berdofe discusses health record banks in the third part of his series on healthcare infrastructure data models. Dr. Gregg explains the commonality of clubbing, EHRs, and religion. Brad Boyd of Culbert Healthcare Solutions highlights the great promise of centralizing patient access and revenue cycle. Take a moment to cool yourself from the summer’s heat with HIStalk Practice’s refreshing ambulatory HIT news. Sign up for the e-mail updates while you are there. And, thanks for reading.
Here’s a gentle reminder for PR folks anxious to get the executive hires of their clients listed in the “People” section of HIStalk. I like including a photo since it’s 100 times easier for someone to recall if they know someone if they’re looking at a photo (can you imagine a text-only high school yearbook?) Every executive should have a LinkedIn profile that includes a high-quality, professionally made head shot (not resized down to the tiny, low-resolution thumbnail – LinkedIn does that automatically, but the high-res version still pops up if you click the thumbnail.) No full-length dramatic pose shot at an angle, no tiny head in a big picture that can’t be cropped without an astounding loss of quality. And of course, as I always preach, don’t bother sending me a press release that hasn’t been posted to the news services or the company’s own site – I can’t use it unless I have something to link to. I’m not in the PR biz, but all of this seems pretty obvious to me.
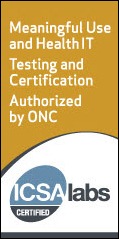
Welcome to new HIStalk Platinum Sponsor ICSA Labs. The company, which is an independent division of Verizon, offers testing and certification of EHRs and health IT technology. They’ve certified over 100 health IT products since launching ONC-ATCB services in March 2011. Vendors (and self-certifying providers) have a choice of testing and certifying partners, so why choose ICSA Labs? (a) their folks have a lot of healthcare and/or interoperability experience (every employee has at least 10 years’ worth); (b) they make sure their clients are prepared for testing, providing them with documents that include sample code, interoperability tips, and step-by-step instructions; (c) they offer low prices, flexible payments, and any needed re-testing within two business days at no extra charge; (d) they help their clients market their certification. Fresh news this week is that ICSA Labs was just accredited by ANSI as a permanent certification body for ONC, meaning they can certify complete EHRs and EHR modules after the temporary program (ONC-ATCB) expires. They created a cool web page just for HIStalk readers, and based on e-mails Inga and I have swapped with some of their folks, they actually read what we write (that isn’t always true of sponsors, although thankfully it usually is.) Thanks to ICSA Labs for supporting HIStalk.
You know what’s coming next: I went to YouTube to scrounge for ICSA Labs videos that would give you a visual on what they do. Here’s a recent and nicely done webcast covering the 2014 Edition Security and Privacy criteria. I was just going to post it and move on, but I got kind of hooked on it and ended up watching a good bit of it.
On the Job Board: McKesson HSM and MAC Activation Support, Account Executive – NE and Mid-Atlantic.
Acquisitions, Funding, Business, and Stock
Gateway EDI, a subsidiary of The TriZetto Group, expands into the hospital and large-practice base with the acquisition of ClaimLogic. Terms were not disclosed, but Sermo had raised $40 million in its seven-year history.
Microsoft reports its first quarterly loss in 26 years as a publicly traded company, triggered by the full write-down of the $6.3 billion it paid to buy ad platform company aQuantive.
Application development tools vendor Progress Software names former Allscripts board chair Phil Pead as non-executive chairman. It also hires former Picis CFO Melissa Cruz as SVP/CFO.
Athenahealth reports Q2 numbers: revenue up 33%, adjusted EPS $0.24 vs. $0.12, beating consensus earnings expectations of $0.23.
Sales
The Denver Hospice selects HEALTHCAREfirst for its clinical and business operations.
Health Management Associates will implement athenahealth’s solutions for its 1,200 employed providers. athenahealth will also offer services to the 10,000 independent physicians affiliated with HMA hospitals.
In the UK, Royal Berkshire NHS Foundation Trust signs a $26 million contract with Cerner for Millennium hosting and system support.
People
MedVentive appoints Bernard Chien (Radisphere) chief technology officer.
John Lynch (Provena Health) is named VP/CIO of Greater Hudson Valley Health System (NY).
Announcements and Implementations
Duke University Health System (NC) goes live on the first phase of its $500 million Epic implementation this week at 33 primary care practices.
ANSI announces the first accredited certification bodies for the ONC’s Permanent Certification Program for HIT. They include CCHIT, Drummond Group, ICSA Laboratories, InfoGard Laboratories, and Orion Register.
CareTech Solutions releases BoardNet 4.0, a new version of its Web-based portal for hospital board members.
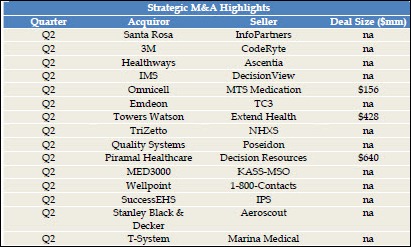
Healthcare Growth Partners releases its healthcare IT and services quarterly report.
Three Sentara hospitals are scheduling inpatient procedures in its Epic system, which the apparently detail-challenged local newspaper interpreted as being synonymous with “smart room technology” because the words were close together in announcement’s headline.
Government and Politics
A House Appropriations subcommittee votes to cut $1.3 billion in HHS funding and eliminate all funding for AHRQ.
CMS announces the 15 ACOs that will participate in the Advanced Payment ACO model and receive upfront and monthly payments to invest in their care coordination infrastructure.
Other
Demand for HIE consulting services is on the rise, according to KLAS. However, hospitals are struggling to differentiate among the 13 firms that offering the service.
A KLAS report on ambulatory EMR perception finds that there’s a lot of rip-and-replace going on, especially in larger practices. Systems from Allscripts, GE, and McKesson are the most replaced (not surprising since they have a lot of customers and have been around for a long time.) Most often chosen as replacement systems are eClinicalWorks, Epic, and Greenway. In addition, the win rate for vendors outside the most popular group increased significantly in the past year. Common reasons for replacement are poor support, hidden costs, and products too technically complicated for a small practice to keep running.
Vermont leaders express frustration with lack of results from $70 million in healthcare IT investment, even though most of that money came from the federal government. A Senator said, “I hear genuine frustration from providers who are spending time and resources trying to modernize and make their offices more efficient, and prepare for the future, and yet every one of them feels like they’ve been burned. Basically we’re not getting any results for these millions and millions of dollars that have been pumped into IT. We should be a lot further along. I just don’t think the leadership’s in place.”
A study finds that registered dietitians can enter physician-approved nutrition orders faster and more accurately than RNs and clerical employees. The original research article, which appeared in a nutrition journal, urges that dietitians be given access to electronic diet order systems.
A pretty funny Gawker article entitled If You Go to a Hospital in July, Get Ready to Die covers The July Effect, which fascinates laypeople because they think we hospital folks try to hide the bungling that happens when clueless new residents first try out their medical wings (we do actually try to hide that, but nobody really denies it.) Gawker’s gonzo journalism summarizes, “Being a doctor is one big game of Operation to these punks. You go in with a headache and all of a sudden they’re trying to remove your Wish Bone with a pair of tweezers, being real, real careful not to touch the sides. The stethoscopes around their necks are made of plastic. Their doctor’s coats are just one of their dad’s white dress shirts.”
Bloomberg covers a California surgery center chain that bills insurance companies exclusively at out-of-network rates, allowing its surgeon-investors earn up to 200% rate of return. The chain’s seven centers bring in $100 million per year in revenue. Aetna is suing the chain, saying it gouges on rates, excessively rewards surgeons for referrals, and defrauds health plans. One surgeon says his partnership was terminated because he didn’t refer enough patients whose insurance had extensive out-of-network coverage, or as the text message the company sent him explained, “Simple rule of thumb is Aetna, United, Cigna, and Blues with no daily max.” The company’s marketing pitch to surgeons was that their $10,000 investment would give them monthly payouts of $6,709. The Iranian immigrant who started the company did so after being inspired by her sister and brother-in law, who were making $10,000 for each out-of-network colonoscopy they performed from a rented office.
Three Chicago-area men contemplate filing lawsuits against Northwestern Medical Faculty Foundation, whose sperm freezers and alarm systems failed in April, ruining the men’s sperm samples they had stored there before undergoing fertility-affecting medical procedures.
Sponsor Updates
- GetWellNetwork creates a highlights video from its May user conference in Orlando. It’s far more interesting and entertaining than you might expect.
- eClinicalWorks was the most-used EHR among respondents to an OIG survey research the use of EHRs, the company says.
- Beacon Partners expands its HIPAA and HITECH privacy and security services into an Enterprise Information Assurance practice.
- Park Place International receives Meditech’s approval to provide OpSus|Connect and secure Meditech VPN support connectivity.
- Billian’s HealthDATA releases its report on the Ten Busiest Home Health Agencies.
- BridgeHead Software demonstrates that its Healthcare Data Management Solution meets the requirements of Integrating the Healthcare Enterprise at the European Connectathon.
- Boca Raton Regional Hospital (FL), The Independent Physicians Association of Nassau/Suffolk Counties (NY), The Huron Valley Physicians Association (MI) and The Arizona State Physicians Association are some of the new health systems and IPAs choosing Greenway’s PrimeSUITE EHR/PM solution.
- The Illinois Department of Healthcare and Family Services expands its contract with Optum to include an expanded data warehouse for advanced analytics.
- OTTR releases details of its September OTTR Users International 2012 meeting in Omaha, NE.
- MDeverywhere selects Health Language’s Language Engine and provider-friendly terminology to integrate with its charge capture software.
- Peoria Tazewell Pathology Group (IL) selects McKesson Revenue Management Solutions to provide RCM services.
CMS publishes a new guide for Eligible Professionals seeking to demonstrate Meaningful Use through the Medicaid program. Although the 94-page length is a little off-putting, it’s written at a high level and is a reasonable entry-level document. If you haven’t figured out your MU strategy and you see a fair number of Medicaid patients, check it out.
The Joint Commission releases a statement on the use of unlicensed persons acting as scribes. Although it is specifically targeted at Critical Access Hospitals, it makes several good points relevant to all settings. You’d think these are largely common sense, but I often see behaviors that don’t quite meet these standards:
- The job description clearly defines scribe qualifications and responsibilities
- The employer offers specific orientation and training
- Employment is contingent on competency assessment and performance evaluations
- Physicians must authenticate notes after the scribe enters them (and do so before leaving the patient care area, since others are using the information)
- Scribes should not enter orders (it’s CPOE, not CSOE)
Especially in the ambulatory setting, I see physicians who think they can take a medical assistant or nurse and add “scribe” to their already-full list of duties. These staffers may be pushed outside their comfort zone with little or no training. They may be expected to document according to “understood” physician intent rather than fully scribing the visit, which is never a good idea. I use scribes in one of my practice settings and a good scribe is worth his or her weight in gold. It doesn’t remove the need for the physician to know the system and be able to assimilate data, however.
I ran across a piece on the “clickiness” of EHRs. I deal with doctors day in and day out who refuse to come to training, yet expect to be instantly proficient in use of EHR, CPOE, and other systems. When they’re not, they blame it on the software. Having been a user of most of the major EHR vendors out there at one time or another, I know that they all have their issues. My favorite comment:
We don’t assume that someone can step up to a piano and play all the right notes to a complicated piece of music with no training. Yet for some reason, we think that a doctor can step up to a complicated piece of software (EHR for those following at home) and quickly navigate all of the features of the software. Training matters and can make the world of difference in how you feel about the number of “clicks” you have to do in your EHR.
Too true. Even with the most intuitive design, physicians who try to leap into seeing patients without adequate training will feel stressed and likely fail. The requirements of documentation (thanks to CMS, payers, regulators, and uber-conservative compliance departments) have become so cumbersome that documenting a visit is like playing a video game – you just have to figure out how to get to the next power-up. Those that recognize it for what it is (just another hoop we have to jump through to get paid) seem to do much better on the learning curve. Yelling at the IT department is not going to change what CMS thinks about documentation bullets and correct coding.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.
More news: HIStalk Practice, HIStalk Mobile.









Dr. Jayne,
Glad you liked my article on EMR Clickiness. For those following at home, here’s a link to the full article: http://www.emrandehr.com/2012/07/16/too-many-ehr-mouseclicks-and-keystrokes-a-solution-for-ehr-vendors/
Epic probably uses an ESOP, a tax-advantaged way to sell stock to employees. The ESOP only counts as one shareholder even if 5,000 employees are benficiaroes of the ESOP.
HEpic is very careful to stay under the SEC limit for shareholders. Carefully adjusted each quarter to avoid reporting requirements. Slightly less than 10% get shares that must be sold back when leaving the collective. Rank and file get Stock Appreciation Rights; imaginary shares with no voting or annual meeting rights.
EPIC’s ESOP reports that there are 1,352 participants in its ESOP a of 12/31/2011
I am sad and my heart goes out to the family of the boy who died at NYU Langone. I am impressed that after spending how many $$$ millions on their Epic EMR system (http://www.crainsnewyork.com/article/20090121/PULSE/901209954), NYU Langone E.D. must now resort to an ingenious paper work around to assure that the results of tests are known by its health care professionals.
It would be helpful for all of us IT specialists to know why the key results were not seen in a timely manner. There has got to be an IT app or solution to their problem.
@suzy, RN
NYU is not yet live on Epic in the ED, also your link requires an account, any chance you can summarize the article?
I don’t believe NYU Langone is live yet on Epic in the ED or hospital.
The University of Kansas Hospital has implemented a real-time clinical surveillance tool for early detection of sepsis.
KU is using a third-party bolt-on to their Epic install because you can’t doreal time surveillance like that on a MUMPS database. Cerner has a real-time agent that uses cloud computing to recognize sepsis. Places like WellSpan in PA a using I and saving lives.
Anon asks for detail on NYU Langone Epic EMR deal: “For NYU Langone, the timing couldn’t be better. This
fall, the Medical Center will become the first healthcare
institution in the New York area to implement computerized
medicine on an enterprise-wide basis when it begins rolling
out Epic, a state-of-the-art information system that promises
to revolutionize NYU’s storage and retrieval of patient
information. Within several years, all medically related
operations — inpatient and outpatient offices, along with
physicians, nurses, pharmacists, claims specialists, and
patients themselves — will be fully integrated through a
single, vast online network…”
If not Epic, what vendor had wired the Emergency Ward?
Even if Epic is live in the NYU ED the outcome ould have been no different. An object oriented database does not allow for the real-time decision support to impact clinical care. Epic does its reporting on an Oracle export, not its native Cache,and that is retrospective, not real-time. While object oriented databases handle the banking type of transactions (deposit and withdrawal of data) reliably and quickly, they cannot handle the analytics to take healthcare to the next level. NYU says it best when they talk ONLY of “storage and retrieval” and say NOTHING of analyzing the data to impact care at the bedside.
When will the misguided notion that using an object-oriented database is the approach to take in forward-thinking healthcare organizations end? Or is the herd mentality that “everyone has Epic so we should too” so dominant that strategic thought processes have been crushed?
Dear Sal,
As an ER doc, I do not need guidance from your apps to detect a sick kid. I do need the results of tests put in to my hands, if there is ambiguity in my clinical exam and eval.
There are countless examples of data going to your devices, but who knew the results were there? No one.
This causes delays in diagnosis and treatment, apparently, just what happened at the NYU.
Harriet,
Kudos to you if you never miss a case of sepsis. In the case at NYU, unfortunately, this child had at least 3 signs of SIRS (fever, tachycardia and tachypnea per the NY Times article), yet was discharged. The Surviving Sepsis Campaign and the GNYHA STOP Sepsis Collabrative (of which NYU is a member) both recognize that many cases of sepsis go unrecognized and the delay in recognition increases mortality. Physicians can ONLY become better clinicians if the right information is delivered to them in a timely manner. Technology, properly applied, assists those trained to care for patients. In your ED I am sure that you use physiologic monitors such as pulse oximeters and EKGs and they sound an alert when an abnormal value or trend is identified. Indeed, no optical in their right mind would purchase such deics that silently recorded data without looking for trends that can identify patients in need of furthe attention.
The EMR is the next stage in that technology. It collects and transmits data, but if that is all its doing, then it’s value is very limited. My argument is that hospitals, like NYU, are spending hundreds of millions of dollars to purchase healthcare nformation systems that are merely recording devices, when the technology exists for those same systems to analyze the “recorded” data for trends that can impact outcomes. Every other major industry gets this concept but healthcare, as typical,is a laggard. Major hospitals, like NYU, a focused on recording transactions today, when they should be BOTH recording those transactions AND analyzing the data so that sepsis is recognized earlier, poor glycemic control is identified before it results in microvasualr disease, etc.
-Sal
To: Sal Mavet
Your comments are very interesting because they go to technical limitation issues. You write coherently too. I’d love to see a longer piece from you on “Databases for Dummies” that would explain to me what’s actually under the hood of Epic and what it means for those of us slated to use it. Or would that be rubbing salt in the wound?