Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…
EPtalk by Dr. Jayne 1/15/26
Plenty of people have been asking me for my thoughts about last week’s announcement of OpenAI for Healthcare.
Models that are tuned to physician needs and that have been through robust clinical testing certainly offer advantages. The incorporation of the organization’s internal documents via SharePoint and other platforms is also attractive.
I recently chatted with a friend who is both a physician and an attorney about the impacts of such integrated solutions on the medicolegal landscape.
In the current state, with many physicians playing the “bring your own AI” game and using various solutions on their phones, no connection exists between those queries and the legal medical record. However, an enterprise platform that ties it all together and specifically encourages the use of patient data and PHI adds an additional layer of complexity to medicolegal investigations.
It won’t just be about the EHR and its audit log. It will involve all the potentially related queries that may have been entered and acted upon by the care team. We’re starting to see some legal activity around physicians who based their decisions on inappropriate AI-generated information. This is an area to watch.
I also wonder about the ability for hospital policies to negatively influence access to information by clinicians. For example, if you work in a hospital that restricts certain procedures or medications for religious reasons, how will those limitations shape the responses when those prohibited treatments might be the right answer for a patient?
This could evolve to include a bedside component for patients. They could ask questions about their care plan while hospitalized. However, they might learn that their care is limited by their choice of facility.
My conference BFF Craig Joseph, MD recently wrote that healthcare is betting on the wrong AI instead of looking at solutions that actually improve clinical outcomes. He cites a study from the University of Southern California that found that physical robots outperformed chatbots in reducing psychiatric distress. He goes on to talk about how the brain perceives interactions when there is a physical presence compared to a virtual one and about the benefits of emotional experience in delivering care.
It made me think of my own experiences with physical therapy. It’s an advantage having your friendly (or not so friendly) physical therapist right there urging you to push yourself compared to a therapy bot at home that is less perceptive when you’re slacking off.
The robots used in the study looked fairly low-tech and had crochet covers, reminding me a bit of the cats in Disney’s “Lady and the Tramp.” For a tech industry that focuses on flashy products, these wouldn’t even be on the radar. I agree with Dr. Joseph that sometimes low tech is best. Maybe we’ll have to make that the focus of our next conference booth crawl.
Speaking of low tech, I was talking with a couple of physician friends recently about the Oura ring as a potential adjunct to addressing sleep issues. One colleague swears by his, although the actions that he has taken based on the ring’s sleep data are the things that every family physician recommends for sleep issues: consistent routine around and time for sleep, adjusting environmental conditions, appropriate timing of meals, and keeping a basic sleep diary to identify triggers.
My other colleague proposed a decidedly low-tech approach: sleeping with a stuffed animal. He pulled out his phone to share a Wirecutter blog from last year that addressed the tactic. It cites several scholars and their comments on the practice, including notes on how it might help adults shift from a state of cognitive arousal to the more relaxed mindset required for sleep.
The blog notes the lack of literature on adults sleeping with stuffed animals, but I bet if we threw some AI into the mix, people would be eager to study it. Maybe those crochet cats can work the night shift as well as having a day job.
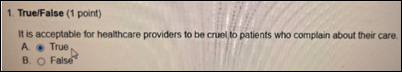
From Night Nurse: “Re: my annual refresher training. Passing pre-tests exempted us from that section. This was one of the questions. What kind of world are we in where this is considered an appropriate question?”
I have unfortunately seen some bad behavior from healthcare providers during my career, so I agree that we should be screening for people who have thoughts like this. I don’t think a bold annual training question is the way to pick them up. Even in a written survey, I would probably recommend a more subtle approach to identify those who have such sentiments. I’ve done a fair amount of work writing test questions and I wonder what the hospital’s item writers were thinking with this one.
From Tech Traveler: “Re: swearing. I’m a medical device representative and read your blog to keep up with healthcare tech topics so I can commiserate with the physicians I call on. I’m in and out of operating rooms and physician lounges all day and notice that there’s a certain amount of swearing that goes on among physicians, but it seems to vary by specialty and age as well as by topic. I’ve joked about doing a research project to explain the phenomenon, but it looks like researchers beat me to the punch.”
The article notes that although swearing is “often dismissed as socially inappropriate,” it has been linked to increased physical performance through state disinhibition. That is a psychological state in which individuals are less likely to restrain their behavior. The authors propose that this leads to flow, confidence, and focus, with those who swear being able to perform better on strength and endurance tasks than those who used neutral words.
They note that “these effects have potential implications for athletic performance, rehabilitation, and contexts requiring courage or assertiveness. As such, swearing may represent a low-cost, widely accessible psychological intervention to help individuals “not hold back” when peak performance is needed.”
Another one of the practices where I receive care has finally given in to the private equity company that has been pursuing it for the past couple of years. The physician mentioned this at a recent visit and shared the behind-the-scenes story. She has been struggling since she opened a second location, but has been keeping her head above water through the availability of same-day dermatology appointments, which turned local primary care doctors into a loyal referral base.
We’ve all been impressed by her ability to fit people in. Who doesn’t love being able to have a patient’s suspicious lesion removed in a timely fashion? Before she opened, patients often waited months for appointments.
Although she offers some cosmetic dermatology services, the practice is heavily skewed towards medical dermatology. She shared that automatic payer downcoding has been financially devastating. Her attempts to promote the more lucrative cosmetic treatments, which are typically cash pay, couldn’t compete with local med spas that run coupon specials. She decided to give in with five years to retirement. We’ll see how well that same-day availability holds up with private equity operations leaders at the helm.
If your care providers have been acquired by private equity, what changes have you noticed? Leave a comment or email me.

Email Dr. Jayne.


On the cruelty question, I interpret it the same way I view questions on security exams that ask whether it’s OK to share your password with other people. Everyone knows the answer but this way they have in writing that you know. That might help in disciplinary proceedings.
https://www.youtube.com/watch?v=b0l3QWUXVho