Today's post contains the phoenixes rising from the ashes of the post COVID telehealth era. There's two things that destroy…
News 9/25/24
Top News
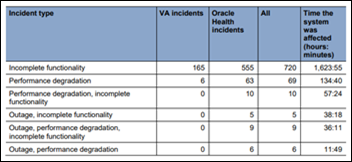
A new report from the VA OIG finds that the VA’s Oracle Health-based EHR that has been implemented at six facilities experienced 826 major performance incidents between October 2020 and March 2024.
Over half of the incidents — including outages, performance degradations, and incomplete functionality — occurred after the VA put further EHR go-lives on hold. Major incidents collectively impacted the system’s performance for nearly 80 days.
The VA plans to restart EHR rollouts sometime next year.
Reader Comments

From Joe Friday: “Re: Particle Health. I believe in sticking with the facts, of which I think maybe they are playing loose and fast. They claim that the Carequality Steering Committee fully agreed with their arguments and did nothing wrong. That’s a knowable fact, isn’t it? I wonder if the steering committee’s report would actually say that. And if not, I would question just how factual the entire suit is.” Particle should be able to produce documentation to support these claims:
- Particle says that both insurers and their software vendors have a right to access EHR patient treatment information. This should be an easy question for ASTP to answer.
- Epic limits the use of its data for treatment purposes, while Carequality’s policy allows it to also be used for healthcare operations and research. All of that is surely documented, assuming that any policy other than Epic’s matters when you’re getting your data from Epic.
- Epic coerced its big-investment customers to stop using Particle. Any such communication should be discoverable.
- The company says that Epic urged its customers to flood Particle with inquiries. The lawsuit cites an Epic recommendation to its clients that they email a generic company support address if they needed Particle’s technical help to audit use of their patient data.
- Epic claims that Particle admitted wrongdoing. Particle should provide the source of this information. It apparently relates to one Particle customer that Epic complained about, which Particle immediately removed from its system.
- Particle cites the Carequality Steering Committee as finding the company guilt-free, yet required Particle to conform to a corrective plan. That documentation should be readily available from Carequality, which will certainly need to get involved in the lawsuit discovery since some of Particle’s accusations involve Carequality and its board decisions.
- Particle says that Epic turned off access to 20% of Particle’s customers “who were seemingly chosen at random.” If I remember correctly, Epic said its logs identified organizations that were retrieving a lot of treatment data without sending anything back to the network, which suggests that they weren’t actually providing treatment and thus were violating its policies.
From Patients Paying the Price: “Re: Oracle Health to Epic conversions. Been a part of a handful of these over the past few years. More often than not, it seems like the legacy systems are poorly implemented and the root cause is hospital/IT leadership. I’ve seen only one instance where I would definitively say that the vendor was at fault. You would think that spending one-fourth of the 8-9 figure price tag of these systems on optimization, hiring more senior employees, and spending the time on governance and training would yield better results. Maybe it’s an easier sell to the board than a harder-to-quantify optimization cycle, that CIOs want a sexy project instead of getting into the day-to-day work of improve patient care and user experience, or maybe I’m just being overly cynical and this is an expected outcome of the implementation rush from the Meaningful Use days of yore. Probably all of the above, but it makes me wonder if these new installs will go any better or they’ll be ripped and replaced in another 10 years for something ‘better.’ At the end of the day, we all know who is actually paying for all of this (patients) and you have to wonder if the cost will pay dividends back.” Health systems try to forget that they have perpetually promised that expensive technology will make American healthcare better, faster, and cheaper.
From Readers Take Note: “Re: scrubbing personal information from the interwebs. You mentioned a service that you liked so much that you upgraded to the annual plan. Could you repost the company’s name?” I’ve used Optery for three years and just upgraded to its extended plan at renewal for $149 per year that covers 186 data brokers (I ended up paying $120 using some promo code I found online). Signing up for a free account shows you which sites are displaying your details, while the subscriber dashboard shows the shocking level of detail that Optery has removed from web searches. You could find and contact those sites yourself, but that would be a lot of work and regular rechecks.
HIStalk Announcements and Requests
I also published today:
- Responses–What Companies Should I Consider for a Mid-Career Sales Job?
- Particle Health Versus Epic Lawsuit Summary
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock

Hancock Regional Hospital (IN) will transition 49 employees to its RCM vendor Revology.
AssureCare, a population health management company focused on the health and human services sector, acquires competitor Clinigence Health.

Seven directors resign from 23andMe’s board, citing differences of opinion on the company’s future. Co-founder and CEO Anne Wojcicki, the only remaining board member, has expressed strong interest in taking the company private amidst declining revenue and a sharp drop in valuation, which has plummeted from $3.5 billion to under $200 million. 23andMe is also facing $30 million payout to settle a lawsuit that accused the company of failing to protect the records of 7 million customers whose information was breached in 2023.
Scribenote, which has developed an ambient documentation system for veterinarians, raises $8 million in seed funding. The brother-and-sister company cites studies that find high burnout rates of veterinarians whose heavy case loads require after-hours medical records completion. Scribenote’s system costs $165 per DVM per month for unlimited records.
A Time article says that reduced payments from pharmacy benefits managers have helped drive drugstore patient satisfaction down 10% in 2024 alone. The article describes the pharmacy customer experience as “miserable” due to understaffed and closed stores, merchandise that has been moved behind lock doors due to shoplifting, and excessive workload that has left some stores with inexperienced pharmacists. Another factor was that the pandemic encouraged consumers to buy prescriptions and merchandise online, which they learned saved them money.
Sales
- Ballad Health will implement Andor Health’s ThinkAndor virtual care technology to unify its virtual care services across facilities in four states.
- Surescripts will use Clear’s identity verification software to enhance ongoing identity validation within its network.
- CareRing Health selects WellSky’s EHR, analytics, and services.
- Wellsheet will add Wolters Kluwer Health’s UpToDate clinical decision support tool to its Smart EHR UI clinical workflow application.
People

Prolucent names Jason Phibbs, MA (Press Ganey) VP of growth.

David Carmouche, MD (Walmart Health) joins Lumeris as EVP and chief clinical transformation officer.

Episode Solutions names Kyle Cooksey (Monogram Health) president.

Paul Burke (Zelis) joins Reveleer as chief product officer.
Announcements and Implementations

Long Island Community Hospital (NY) rolls out MyWall interactive bedside tablets using technology from OneView Healthcare as part of an enterprise implementation across NYU Langone Health.
Government and Politics

HRSA awards contracts to to five federal contractors to overhaul the national Organ Procurement and Transplantation Network’s systems that are provided exclusively by United Network for Organ Sharing (UNOS).
ASTP publishes a draft of the 2024 Federal FHIR Action Plan.
The Indian Health Service says that it will avoid the VA’s mistakes with its own Oracle Health project:
- The IHS system was competitively bid, unlike the VA’s $10 billion, no-bid contract.
- IHS’s $2.5 billion project will be managed by government contractor GDIT, where the VA allowed Oracle Health (Cerner at that time) serve as its own prime contractor.
- IHS will invite participation of tribes and urban Indian organizations and will require implementation only at those clinics that IHS manages directly.
Other
A transplant surgeon at Memorial Hermann Health System admits to state health authorities that he changed patient data to move specific transplant candidates higher on the list.
Sponsor Updates

- Ascom employees volunteer at the Salvation Army Thrift Store in Raleigh, NC, helping to organize, sort, tag and put items on display for resale.
- Dronning Ingrids hospital in Greenland will implement Sectra’s enterprise imaging software.
- AdvancedMD staff win numerous medals, raise $2,600 for the Utah Food Bank, donate 22 units of blood to the American Red Cross and the local blood donor center, and win the Heart & Soul Award during the Salt Lake County Corporate Games.
- Availity releases a new episode of its Availity on Air Podcast, “A New Approach to Prior Auths with Elevance Health.”
- Capital Rx releases a new episode of The Astonishing Healthcare Podcast, “The Rise of GLP-1s & Partnering to Manage Chronic Diseases, with Vida Health.”
- The Empowered Patient Podcast features CliniComp SVP of Client Services Sandra Johnson, “Innovation in the EHR Landscape to Break Down Data Silos and Improve the Healthcare Provider Experience.”
Blog Posts
- Key Insights From the 2024 KLAS Digital Health Investment Symposium (Tegria)
- Meditech Expanse 2.1 to 2.2: What Will Nurses Think? (CereCore)
- Driving Revenue Cycle Success with Intelligent Automation (AGS Health)
- Learn How Top PE-Backed Medical Groups Scale Their Team’s Expertise (Alpha II)
- Increase revenue by complying with current Medicare waste/charge billing requirements (Altera Digital Health)
- Hiring for Culture Fit: Why It Matters and How to Do It Right (Direct Recruiters)
- From the Last Go Live to the First Upgrade (Divurgent)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



Don’t worry about rip and replace. In 10 years, there won’t be any alternative to Epic.
Re: “…legacy systems are poorly implemented …”
and
“Maybe it’s an easier sell to [Board/CEO/Senior Management]”
Yes. I’ve seen this routinely, and outside healthcare too. Implementing the new system becomes the one and only priority, while leveraging/optimizing the new system falls through the cracks.
It’s a failure to set expectations properly. The “New System” becomes code for, “the New Horizon”, “Everything Is Better Land”, and “Improvement is as Easy as Falling Down.”
Eventually, the New System becomes the Old System. I’ve literally seen a failure to optimize the Old System, as justification for the Next New System!