Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…
Monday Morning Update 9/16/24
Top News
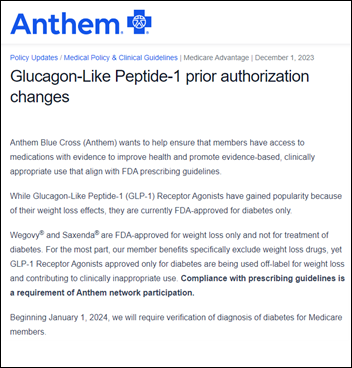
Elevance Health’s Anthem Blue Cross Blue Shield accuses physicians of falsifying patient medical records with the intention of getting the insurer to pay for improper prescribing of the diabetes drug Ozempic for weight loss, a use that is not approved by the FDA.
The insurer is demanding that those prescribers reimburse the company directly and is sending them bills. It warns providers that falsifying medical records or prior authorization requests to obtain insurance payment constitutes fraud.
Anthem notified one physician that he had submitted prior authorization forms for 125 Ozempic prescriptions for 22 patients and asked him to pay the $126,00 that the company had covered for patients. The doctor said that he did not submit any PAs and never claimed that the 22 patients were diabetic – he says he just issued the prescriptions and Anthem paid.
Experts suggest that it is unlikely that doctors can be compelled to pay the insurer since they did not benefit directly from issuing the prescriptions. They also note that providers can legally prescribe a drug for any purpose regardless of FDA’s approval for a given condition, although insurers make their own decisions about coverage.
Reader Comments
From Bigdog: “Re: S&P Consultants. Did they divorce from Nordic?” Nordic acquired the company in December 2021. The LinkedIn of Andrew Splitz says he worked for Nordic / S&P from the acquisition until September 2023, then lists him as S&P’s founder and CEO as of September 2024. Also updating LinkedIn from Nordic to S&P effective this month is newly announced S&P president Zach Johnson. The old website still had Nordic on the logo until that site was inactivated in December 2023.
HIStalk Announcements and Requests
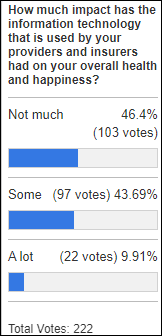
Poll respondents have seen modest impact on their health and happiness that can be attributed to the IT decisions of their providers and insurers.
New poll to your right or here, because of a comment by Dr. Jayne: In the past two years, have you carried your paper medical records from one provider to another?
Webinars
September 17 (Thursday) noon ET. “Level Up Your Stars – Innovative Approaches to Boosting Quality Performance.” Sponsor: Navina. Presenters: Dana McCalley, MBA, VP of value-based care, Navina; Michael S. Barr, MD, MBA, chief medical officer, PreferCare; Yair Lewis, MD, PhD, chief medical officer, Navina. The presenters will explore strategies to boost quality performance and close care gaps effectively. Topics include enhancing quality metrics, developing strategies for care gap closure, leveraging AI for enhanced performance, and optimizing workflows.
September 19 (Thursday) 1 ET. “Cutting-Edge Conversations: A Fireside Chat With Top CMIOs.” Sponsor: DrFirst. Presenters: Drex DeFord, MSHI, MPA, This Week Health; Lacy Knight, MD, MSMI, Piedmont Health; Jake Lancaster, MD, MSHA, MS, Baptist Memorial Health Care; Colin Banas, MD, MSHA, chief medical officer DrFirst. This fireside chat will distill key points from 15 CMIO participants of the 229 Executive Summit. Topics include the impact of AI on clinical workflows, strategies for optimizing healthcare operations, addressing physician burnout and patient safety, and advances in population health management.
October 3 (Thursday) 1 ET. “Navigating AI-Powered Medical Interpretation: Insights for Health Leaders.” Sponsor: Globo. Presenter: Dipak Patel, CEO, Globo. AI is redefining how providers can communicate with patients who speak limited English. However, not all LLMs are created equal, and their potential and limitations need to be examined further. Globo has published its results from testing several LLMs. This webinar will address the promises and perils of AI-enabled medical interpretation in summarizing that research in four key domains: the process of AI interpretation, how to measure it, the state of AI tools today, and the areas where AI falls short with interpretation.
Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Sales
- Bergen New Bridge Medical Center chooses NeuroFlow’s tools to identify and prioritize the behavioral health needs of ambulatory care patients.
- Curry Health Network (OR) goes live on Epic via the Community Connect model, replacing CPSI Evident Thrive.
People



Virtual nursing solution provider Collette Health promotes Holly Miller to CEO and hires Leif Cefalo, MBA (TraceLink) as VP of revenue operations and Terri Davis, MA (HealthEC) as VP of marketing.
Announcements and Implementations
UTHealth Houston will collaborate with OpenAI to give students, faculty, and staff access to ChatGPT Education to develop HIPAA-compliant applications.
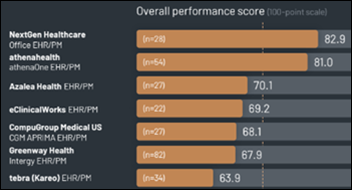
A new KLAS report on EHR/PM in practices with 10 or fewer physicians is topped by NextGen Healthcare and Athenahealth, with all other vendors trailing significantly. Elation Health and Epic Community Connect scored well but with limited user feedback. The top add-on solutions clients that sought elsewhere are telehealth, patient engagement, patient intake, RCM, and analytics.
Privacy and Security
Atrium Health notifies patients that an unauthorized third party gained access to multiple employee email accounts in a phishing attack. The health system says that the two-day incident affected only patients and employees whose information was contained in the emails or attachments of the affected accounts.
23andMe will pay $30 million to settle a lawsuit that accused the company of failing to protect the records of 6.9 million of its users whose information was exposed in a 2023 breach.
Sponsor Updates
- CereCore wins ClearlyRated’s 2024 Best of Staffing Client and Talent 5 Year Diamond Awards for service excellence.
- Knox Public Health improves revenue with EClinicalWorks EHR and RCM optimization services.
- Healthcare IT Leaders releases a new podcast, “Focus on Employee Health and Cost Savings at Northwell Direct.”
- Waystar will exhibit at the HBMA Revenue Cycle Management Fall Conference September 17-19 in Austin.
- Optimum Healthcare IT launches a data and analytics governance offering and hires Terri Mikol (Clearsense) as principal data governance advisor.
Blog Posts
- Building a Workday Resource and Staffing Plan for Healthcare (Healthcare IT Leaders)
- 5 Ways to Empower DSPs in Recognition of Direct Support Professionals Month (Netsmart)
- Governing GenAI in healthcare: a strategic imperative (Nordic)
- Ensuring Technical Readiness for Your Go-Live (Optimum Healthcare IT)
- Healthcare Contact Center Top Challenges: How to Solve Them (PerfectServe)
- Innovation Day: A Day Dedicated to Moving Mountains (Prominence Advisors)
- Mastering Anesthesia Scheduling for Optimal Efficiency and Care (QGenda)
- Adapting IT Recruiting Practices for Healthcare Projects (Revuud)
- How RLDatix Supports Readiness and Implementation of CMS Patient Safety Structure Measure (RLDatix)
- What is a Travel Nurse? Salary, Benefits, and Everything You Need to Know (SnapCare)
- Optimize Plan Design with 4 Practice Use Cases for Therapeutic Alternatives (Surescripts)
- The Ethics of RCM: Balancing Profitability with Patient Care (TruBridge)
- Beyond De-Duplication: Innovative Use Cases for Master Data Management in Healthcare (Verato)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



Re: BCBS GLP-1. If anecdotal studies have shown that these drugs also reduce addictions, and improve BP and other metabolic diseases, why aren’t insurers pushing them instead of limiting them? Taking a drug that will prevent further metabolic disease seems like a logical cost-cutting opportunity. They should be making it easier for physicians and patients to obtain these life-changing drugs. A couple of people I know have lost ~100 lbs and are off all their other meds. BP is stable etc.
I suspect that there are a lot of opportunities for problematic use of GLP-1. And I doubt that anecdotal studies will be enough to settle the matter of safe and appropriate drug uses.
Somewhere (sorry, I don’t have a source at hand) I read that patients who go off the drugs? They regain the weight. Thus weight control with Ozempic means long-term or lifetime prescription regimes.
For morbidly obese people, this would seem to be a very promising clinical approach. However I can easily see people who want to lose 20 pounds for a social occasion, taking GLP-1 for a week or two to achieve that. OK, what are the clinical implications? And do we want insurers paying?
We already know that overweight people are prone to dieting for a while, losing weight successfully, then going off the diet and regaining the weight. Is Ozempic going to be different, and if so, why?
My guess is, there’s a psychological layer that is shared between treatment with diets and treatment with GLP-1.
https://www.epicresearch.org/articles/many-patients-maintain-weight-loss-a-year-after-stopping-semaglutide-and-liraglutide
https://www.epicresearch.org/articles/patients-with-higher-initial-bmis-and-greater-weight-loss-while-on-glp-1s-most-likely-to-maintain-or-continue-weight-loss-after-stopping-glp-1s
Regaining the weight is a risk, but it seems many people with obesity maintain or even lose more weight after discontinuing the medication. Perhaps the adjustment while on the medications leads to better habits?
If those results hold up, that would be awesome!