I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…
News 12/8/21
Top News

The Spokane, WA newspaper talks to local patients and employees about the VA’s implementation of Cerner at the city’s Mann-Grandstaff Medical Center, reporting these issues:
- Two former senior VA officials who were involved in the project say it was misguided and is unlikely to improve on the existing VistA system.
- One hour after VA Deputy Secretary Donald Remy assured a House subcommittee that “The Cerner system works,” the system went down for 80 minutes and had at least some downtime 10 times in September and October. The system has gone fully down four times since it went live in October 2020.
- Former VA deputy CIO and CTO Ed Meagher said it is “absolute malpractice” that the VA did not anticipate performance problems by modeling workload against infrastructure, adding that otherwise, “you’re working off of Cerner marketing material.”
- Several veterans said they were unable to navigate the patient portal and it sometimes locks up and fails to deliver messages.
- Prescriptions were not transferred to Cerner, requiring mistake-prone manual re-entry that left some veterans without psychiatric and other chronic care medications.
- Employees sometimes have to fax medication lists when patients are sent to other facilities for emergency treatment that isn’t offered 24×7 at Mann-Grandstaff..
- The VA, which was the subject of a national wait-time scandal in 2014, has removed Mann-Grandstaff from the wait time web page because it hasn’t figured out how to measure wait times on Cerner.
- The VA’s training did not include the referral management module and one veteran whose urology referral was lost was found to have an untreated, aggressive form of prostate cancer when finally seen nine months later.
- A chief of anesthesiology said EHRs are billing systems with text editors tacked on while VistA was written by clinicians whose goal was to provide the best care possible. He says that Cerner told him that one online form requires 90 minutes to complete, and when doctors told the company that the nurse had under five minutes to examine the patient and document the visit, Cerner said they should hire more people.
- Meagher concluded, “What Cerner does best is capture billable events via exhaustive questions and back-and-forth as you input things. That’s what ties them up. They’re answering questions that are meaningless to them. They’re very meaningful to a commercial organization, because that’s how they get paid, but they’re meaningless to the VA.”
Webinars
December 8 (Wednesday) 1 ET. “What Lies Ahead for the EHR’s Problem List.” Sponsor: Intelligent Medical Objects. Presenters: James Thompson, MD, physician informaticist, IMO; Deepak Pillai, MD, MBA, physician informaticist, IMO; Jonathan Gold, MD, MHA, MSc, physician informaticist, IMO. The EHR problem list can be cluttered with redundant, missing, and outdated diagnoses, and displays don’t always help clinicians process the available data correctly. The presenters will discuss how improvements in creating, maintaining, and displaying problems could reduce errors and decrease the cognitive load of clinicians while continuing to optimize reimbursement.
December 9 (Thursday) 1:30 ET. “Cone Health: Creating Extreme Efficiencies in Surgical Services.” Sponsor: RelayOne. Presenters: Wayne McFatter, RN, MSN and Sharon McCarter, RN co-directors of perioperative services, Cone Health. The presenters will discuss how they have empowered the entire surgical care team, including vendor representatives, to get real-time access to surgery schedules and case requirements in the palms of their hand. RelayOne CEO Cam Sexton will also present the findings of a recent study of 100 hospital leaders regarding their operating room optimization plans for 2022.
December 14 (Tuesday) 1 ET. “Using Cloud to Boost AI and Enterprise Imaging.” Sponsor: CloudWave. Presenters: Larry Sitka, MS, VP/CSIO of enterprise applications, Canon Medical Informatics; Jacob Wheeler, MBA, senior product manager, CloudWave. Enterprise imaging has remained a holdout of data center complexity despite the benefits the cloud offers. The presenters will discuss innovative ways to reduce complexity and lead with disruptive technology using AI, enterprise imaging, and the cloud.
December 15 (Wednesday) 1 ET. “Improve Efficiency, Reduce Burnout: Leveraging Smart Clinical Communications.” Sponsor: Spok. Presenters: Matt Mesnik, MD, chief medical officer, Spok; Kiley Black, MSN, APRN, director of clinical innovation, Spok. The presenters will identify the technologies that most often contribute to clinician burnout, then explain how improving common clinical workflows can help care teams collaborate better and focus on what they do best—taking care of patients. They will describe how a clinical communication and collaboration platform can automate clinical consults and code calls to alleviate burnout.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Accounting and advisory firm BDO USA acquires 90-employee Culbert Healthcare Solutions.
Healthcare voice AI vendor Suki raises $55 million in a Series C funding round that values the business at $400 million.
Change Healthcare will permanently lay off 170 employees in Pittsburgh in February.
Sales
- The Christ Hospital Health Network in Ohio will offer IncludeHealth’s virtual physical therapy service to its pre- and post-operative patients.
- Kidney care company Strive Health selects Bamboo Health’s Pings real-time admission, discharge, and transfer (ADT) e-notifications; and interactive, real-time Spotlights performance metrics dashboards.
People

Valerie Simon (Rise Consulting) joins Lumeris as SVP and chief of marketing and communications.

Lee Taylor, MBA (Relatient) joins Health Catalyst as VP of sales.
Geoff Gibson (Teladoc Health) joins Mend as VP of sales.

Wolters Kluwer Health promotes Greg Samios, MSE, MBA to president and CEO of the clinical effectiveness business unit.

Zach Wood, MBA (Surescripts) joins Well Health as head of corporate development.
Announcements and Implementations
Ochsner Health (LA) has implemented provider data management and API technologies from Kyruus to improve patient-provider matching on its website and apps.
Mach7 Technologies incorporates ImageMover’s EHR-integrated medical imaging capture technology into its vendor neutral archive and enterprise diagnostic viewer.
Surescripts leverages Diameter Health’s data optimization capabilities to ensure specialty pharmacies can easily access accurate patient data through the Surescripts Specialty Medications Gateway.

Holy Cross Health (FL) implements online patient appointment scheduling capabilities from DocASAP.

HCA Healthcare will go live on Meditech Expanse at three hospitals in New Hampshire by the end of 2022, with the assistance of CereCore.
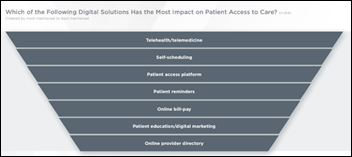
A survey performed by the Center for Connected Medicine and KLAS finds that health system executives expect patient access to be the top area that will be improved by digital health. Respondents name telehealth as the greatest area of technology-driven improvement in the past two years, while 38% expect AI to be the most exciting emerging technology in the next two years but acknowledge that it hasn’t yet met expectations for improving patient outcomes. Nearly all of the respondents say their health systems are placing a high priority on improving access and most of those say they will invest in technology accordingly (most commonly used are telehealth, patient reminders, an online provider directory, and online bill pay). Just over half of responding health systems are using some form of a digital front door, but expect to continue improving and optimizing it while recognizing that not all patients want to connect digitally. Only 17% of respondents are using patient financial financial experience vendors such as Flywire, Patientco, and RevSpring. Health systems like the idea of price transparency, but recognize that it’s hard to show a given patient their actual cost.
Other
A study using Epic Health Research Network finds that 91% of sore throat patients whose encounter was via telehealth are prescribed antibiotics without having a strep test performed (down from 98% pre-pandemic), while the test was done before prescribing (per AAFP recommendations) for in-office visits about half the time, raising concerns about future antimicrobial resistance.
An imaging magazine says that even though the just-concluded RSNA 2021 conference had two-thirds fewer professional attendees compared to pre-pandemic numbers, vendors were happier because the interactions they had were more serious in the absence of “tire-kickers.” It says that HIMSS21 similarly delighted exhibitors with one-third the usual attendance because only non-buyers stayed home (color me skeptical in a “make lemons into lemonade” sort of way now that brag-worthy record attendee numbers aren’t happening).
Sponsor Updates
- Availity rebrands its suite of provider products to Availity Essentials, and will soon give its customers the ability to gain access to additional payers throughout its network.
- The State of Delaware’s Treatment and Referral Network, built on Bamboo Health’s OpenBeds software, has in its first year seen a 45% increase in treatment referral requests and a 25% increase in the rapid acknowledgment of referrals.
- CHIME names University of Missouri Health Care CEO Jonathan Curtright and CIO Bryan Bliven winners of the 2021 CHIME-AHA Transformational Leadership Award.
- CloudWave congratulates 14 of its hospital partners for being recognized as part of CHIME’s Digital Health Most Wired program.
- Gartner includes Dimensional Insight in its 2021 “Hype Cycle for Healthcare Providers” report as a sample vendor in the Digital Analytics Architecture category.
Blog Posts
- Why Resilience is Not Enough for Today’s Healthcare Cybersecurity and Privacy Programs (Clearwater)
- Introducing: True remote diagnostic imaging workflow (Agfa HealthCare)
- Improve healthcare cybersecurity through Zero Trust (Alcatel-Lucent Enterprise)
- Azara Mourns Loss of Cherished Colleague (Azara Healthcare)
- How the CMS Interoperability and Patient Access Rule Creates a Vision for Interoperability and the Delivery of Whole Person Care (Bamboo Health)
- From EHR to Health IT Operations: 10 Ways to Lower Costs and Save Time (CereCore)
- HEDIS 2022 is Here: Everything Payers Must Know (Collective Medical)
- (Part 2) Reaching Patients Along the Specialty Medication Journey: Trusting Patients (ConnectiveRx)
- UMass Memorial Health: In-Home Hospital Care Focused on Equity (Current Health)
- Toward the Liberation of Medical Data (EClinicalWorks)
- Better estimates, faster payments: using automation for a better patient financial experience (Experian Health)
- Driving Value: Taking the Healthcare Revenue Cycle to the Next Level (EZDI)
- Sorting Through ServiceNow Opportunities (Optimum Healthcare IT)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.




Huh, do the major telemedicine urgent care vendors have better antibiotic stewardship than Epic’s customers when it comes to telemedicine? Though I can’t source it, Teladoc’s reported numbers were better than that. I guess Teladoc is in some way a specialty in this appointment type so would be more likely to have those programs in place.
in regards to the VA issues, they went to Jared.
I’m reminding of the scene in The quiet man, where someone says “if you knew your history as well as you say you do”.
“What Cerner does best is capture billable events via exhaustive questions and back-and-forth as you input things…. They’re very meaningful to a commercial organization, because that’s how they get paid, but they’re meaningless to the VA.”h
Well, they’re not meaningful to the actual healthcare providers in the commercial organization. So the problem, although admittedly large in the VA context, is really universal, namely trying to organize clinical information and reasoning using “billing systems with text editors tacked on.”
Wow, that Spokane article on Cerner sure was a hatchet job, but I guess it helps sell more papers, helps the publisher get more visibility.
Looking at all those purported claims of various things that have gone “wrong” I’d wager a heavy bet that same could have been said for any EHR vendor in the market today that would take on such a large and visible deployment of their solution.
This quote towards the end: “ What Cerner does best is capture billable events via exhaustive questions and back-and-forth as you input things.” Reminds me of a conversation I had with my doc at then Partners Healthcare after they went live with Cerner’s major competitor. My doc echoed the same sentiment in saying to me: “It’s a good system for billing I guess, but does nothing for me in helping to care for my patients.”
Sad testament to our massive efforts to digitize health. It’s a slow slog.
Yeah? I guess? The real problem is, nobody is going to pay for the things that help doctors take better care of their patients, unless there is an “ROI” associated with it. I have almost 18 years’ worth of confluence pages, sharepoint documents, emails sitting in my draft folder, wherever I can write, containing detailed specs, wireframes, user stories, workflow, requirements, etc. that would make the lives of clinicians (and their patients) better but…in the end there’s no business case. There are a lot of smart and creative people in healthcare IT with a lot of really good ideas, who want to do the right thing, but none of us work for free and that’s what it all comes down to at the end of the day.
This is the most accurate (and tragic) observation of how the industry operates that I’ve ever seen – thank you!
But, isn’t it obvious? None of the doctors/nurses/hospitals/clinics are free. Whatever you want/need, someone has to create it and that someone needs to get paid. The doctors (in most cases) do not really care about the billing aspects of the system as long as they get paid. They don’t want to accept the fact that the reason the billing is complicated is that they want to get paid “more”. It is very easy to skip several fields on multiple forms and code a complex procedure as an office consult and get paid $129 instead of $6,429 but they won’t do that. Doctors need to get off their high horse and stop complaining about software being too complex. One thing that this industry has taught me over several decades – waste or excess for one group is lunch for the other group.
Please don’t call our industry names – it is just business.
That’s how *all* industry behaves. I deserve to be paid for my work, and I don’t apologize for that. If you want what I can build that will make your life easier, you can pay me for it. If you don’t place a dollar value on it that is more than it costs me and my colleagues to build it, then you can’t have it. This is true for healthcare software, washing machines, off-the-rack shirts, and french fries.
Cerner at the VA it’s a chronicle of a death foretold.
Complaints started from day 0, years ago – physicians, nurses, pharmacists, administrators, patients – all complained about the issues with Cerner.
The result ? “The beating will continue until everybody’s happy…”
IMHO – only a major catastrophe (hospital off line for 6 months, deaths of numerous patients due to errors, major litigations, loss of millions in revenue, etc. – will cause VA, Congress to reconsider this piece of crap called Cerner.
And no, I don’t think Epic is any better…after trying to work as a physician with both EHRs…
Got it. So what do you suggest?
Stay with the working horse Vista …
Invest the billions slated for Cerner – in improving Vista – an open source EHR that is better suited for the VA than epicerner will ever be,
I admit Vista it’s not as good a billing / patient milking machine as epicerner may be…
The feds can only use misaligned and under incentivized contractors. The federal government can’t employ any number of software developers, because the feds can’t pay or hire enough, because of salary caps and other limits to hiring. This compensation scheme is a continued request from multiple well-represented political interests. One is the chamber of commerce-esque lobby, which is involved in the coalition of both political parties. One political party, the one that made the Cerner decision, also has a more direct influence from large corporate and multinational interests; they have a mandate to minimize the capacity of federal government to implement really anything. The VA benefits a veteran constituency in a political coalition with corporate interests that want the VA benefit gone.
If the solution requires changing a fundamental preference or coalition of a major political party, it is hard consider it a solution. If we’re talking major political party change, then why focus on the VA instead of universal healthcare or something on the minds of most americans? Here’s my solution within the constraints. Find an executive good at bullying departments into action. Pair that bully with Mina Hsiang and put them in charge of changing the VA. Recruit staff by giving the promise that if they prove they can manage one of the most technologically challenging gov problems at one of the largest government bureaucracies, they’ll get their pick of and subsequent support at any other federal government position.
A reminder that the original bad-at-face-value Cerner decision was made by the Obama administration for the DOD. The subsequent worse-at-face-value decision was no-bid by the Trump admin because “how else could the two systems be interoperable?” Plenty of blame to go around, red and blue.
I’ll note to the several people above with an anti-EHR agenda that saying “Cerner is designed for/ good at billing” is an instant tip off that you don’t know what you’re talking about.
Whatever the contract is or could have been, they have it now. I’m not looking to blame anyone, just pointing out the bounds the VA operates within.