I definitely leave my mic on often as I walk around. It's never recording, but it's easier to leave it…
News 1/29/21
Top News

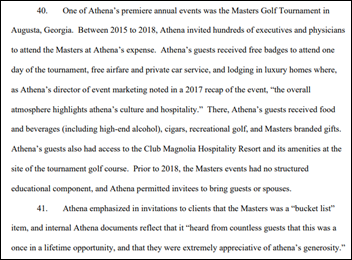
Athenahealth will pay $18.25 million to settle federal False Claims Act allegations that it paid kickbacks to increase sales of its products from January 2014 through September 2020.
The federal government says the company’s marketing programs:
- Provided prospects with all-expense-paid sporting, entertainment, and recreational events, including luxury trips to the Masters Tournament and Kentucky Derby.
- Paid customers up to $3,000 for each new physician who signed up after being identified by the customer as a prospect.
- Entered into deals with companies that were retiring their health IT products (SOAPware was the biggest such arrangement) to refer their users to Athenahealth.
Reader Comments
From Dirty Martini: “Re: Olive. I interview with them just over a year ago for a solution architect position, which reviews tasks that are candidates for automation and then translates the requirements from the customer to the development. Nothing about their services involved AI and customers could do everything they were proposing with standard Epic enterprise functionality. It’s interesting to see how much they’ve grown, but I’m not confident they have actual AI or will have it in the near future.”
From Dripping Faucet: “Re: Baylor Scott & White. Stay tuned for outsourcing and layoffs.” The health system announced Monday that it will outsource or reassign 1,700 employees in hoping to save $600 million over five years. Two-thirds of those affected will be transferred to third-party partners, while 650 jobs will be eliminated with the possibility of retraining for different positions. The health system didn’t announce those third-party partners, but employees reported that one of them is Atos.
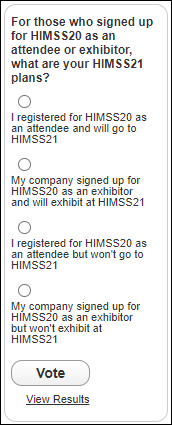
From Pondering Exhibitor: “Re: HIMSS21. Looks like there a lot of available spaces or those labeled ‘HIMSS’ on the show floor. Will you be doing an updated survey to ask vendors and attendees about their HIMSS21 plans? The deadline to cancel booth space is February 4.” That’s just a week away, so I’ll run a special poll now: For those who signed up for HIMSS20 as an attendee or exhibitor, what are your HIMSS21 plans? You can add a comment with an explanation of your decision after you vote. The floor plan shows 401 exhibitors, no keynotes have been announced, and the call for proposals runs until February 24, so it will be a leap of faith to commit without knowing who is presenting and exhibiting, not to mention that COVID limitations are hard to predict these days. I have heard nothing as a member or HIMSS20 registrant, but an exhibitor passed along a rumor today that HIMSS will make some kind announcement about HIMSS21 in the next three days, and given its quietness otherwise, it could be a significant one that will make my poll instantly obsolete.
HIStalk Announcements and Requests
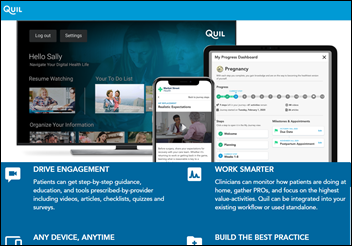
Welcome to new HIStalk Platinum Sponsor Quil. The Philadelphia-based company, which is a joint venture between Independence Health Group and Comcast, is the digital health platform that offers personalized and interactive health journeys to consumers and their caregivers. Quil is committed to educating and engaging consumers, leading to better health experiences and better outcomes, at a lower cost. Quil serves patients, members, and their caregivers in partnership with their healthcare providers and health plans nationally. Thanks to Quil for supporting HIStalk.
Webinars
February 24 (Wednesday) 1 ET. “Maximizing the Value of Digital Initiatives with Enterprise Provider Data Management.” Sponsor: Phynd Technologies. Presenters: Tom White, founder and CEO, Phynd Technologies; Adam Cherrington, research director, KLAS Research. Health systems can derive great business value and competitive advantage by centrally managing their provider data. A clear roadmap and management solution can solve problems with fragmented data, workflows, and patient experiences and support operational efficiency and delivery of a remarkable patient experience. The presenters will describe common pitfalls in managing enterprise information and digital strategy in silos, how to align stakeholders to maximize the value of digital initiatives, and how leading health systems are using best-of-breed strategies to evolve provider data management.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
GetWellNetwork acquires consumer engagement software vendor Docent Health.
Emids acquires software development consulting firm Macadamian.
EHR-integrated patient-specific prescription pricing platform vendor RxRevu raises $7 million in a Series B funding round, increasing its total to $28 million.
Investors are reportedly discussing executing a deal in which consumer health information platform Sharecare would be merged with AI vendor Doc.ai with the combined companies then being taken public at a valuation of $4 billion.
SCP & CO Healthcare Acquisition Company, a health IT-focused SPAC, closes its initial offering for $230 million and will begin looking for one or more companies to absorb.
NextGen Healthcare reports Q3 results: revenue up 3%, adjusted EPS $0.26 versus $0.23, beating Wall Street expectations for both. NXGN shares are up 59% in the past year versus the Nasdaq’s 45% gain, valuing the company at $1.5 billion.

The Cincinnati business paper profiles clinical collaboration platform vendor Halo Health, which just announced new financing and the hiring of its first chief marketing officer and CTO.
Sales
- The state of West Virginia will use Everbridge’s COVID-19 Shield Vaccine Distribution – an extension of its critical event management system — to coordinate vaccine distribution and schedule appointments.
- UNC Health chooses Medicom Health’s Epic-integrated Rx Savings Assistant solution to notify prescribers of pharma discounts and free trials for their patients.
People

4Medica hires Cynthia McIntyre (IBM Watson Health) as SVP of sales and marketing.

Children’s therapy provider The Theraplay Family of Companies names Fran Spivak, MS, RN (Strive Health) as VP of IT.

Verily hires Preston Simons, MBA (Simons & Associates) as CIO.
Announcements and Implementations
Optimum Healthcare IT will offer its CareerPath health IT apprenticeship program at University of Colorado Denver, giving students three months of health IT training, then hiring them on after completion.

Darena Solutions offers a free version of its BlueButtonPro solution for meeting Cures Act interoperability and patient access requirements.
A new KLAS report on quality management solutions — which includes quality and regulatory reporting, performance improvement and benchmarking, and patient safety and risk – finds that Naunce and Medisolv lead in overall performance, while Conduent users are dissatisfied and the company has backed away from its Juvo product and is again developing the Midas platform. IBM Watson Health has the lowest “would buy again” percentage as users report lack of innovation and the feeling that the company has forgotten them. Premier scores well for advanced users but is seen as being expensive, while Vizient users like its peer-hospital comparison but think the product is cumbersome.
A Black Book population health management poll of hospitals, practices, and payers finds that most expect to spend more for systems and integration, while one-third expect the government to offer incentives for providers who participate in information blocking rule fixes. Some of the PHM system vendors that score tops in customer satisfaction and loyalty are Azara Healthcare, Inovalon, I2I Population Health, Cerner, Datarobot, Casenet Trucare, and Epic MyChart.
Government and Politics
Oki Mek, recently promoted to HHS’s first chief AI officer, shares its AI plan, in which it defines its role as an AI regulator, investor, convener, and catalyst.
The state of Oklahoma rejects a protest from non-profit HIE MyHealth Access Network, whose $19.9 million software bid for a statewide HIE was turned down in favor of $49.8 million offer from Orion Health.
CACI wins a $96 million US Army task order to test, train, and deploy its MC4 battlefield EHR.
COVID-19
CDC reports that 26 million COVID-19 vaccine doses have been administered of 48 million distributed (54%).
A KHN report says that information about who has been given COVID-19 vaccine is only as good as the US’s 64 unconnected vaccine registries, which is to say not good at all since many immunization records are missing race, ethnicity, or occupation that might be useful in monitoring progress.
Seattle’s Overlake Medical Center & Clinics is chastised by the governor for emailing 100 big donors with a link to sign up for invitation-only COVID-19 vaccination even though its public-facing scheduling site showed no available appointments. The email said that the hospital had reserved 500 openings over a week and contained an access code for access. The hospital apologized and said the invitation was a quick fix that followed last week’s eligibility expansion to anyone 65 or over, with the demand that followed overloading its scheduling system. The hospital says it simply contacted the people whose email addresses were on file as an efficient way to open up slots that couldn’t be moved easily to the new scheduling system.
California will turn over its struggling COVID-19 vaccination program to Blue Shield of California, which will oversee distribution and most likely replace the state’s complex vaccine eligibility rules with age-based ones that aren’t dictated by where the individual lives or the jobs they hold. Governor Gavin Newsom had challenged state residents to hold him accountable for administering 1 million doses in 10 days, but two weeks later, found that coding errors and lags in reporting made it impossible to even know how many doses have been administered.
North Carolina’s state hospital association complains to the governor that the state’s Accenture-developed COVID Vaccine Management System is burdensome and ineffective, creating bottlenecks in vaccine delivery. The system, which will cost $7 million through May, does not provide vaccination scheduling or text message reminders as the state’s contract requires. One hospital says it takes 8.5 minutes to upload the data of a single patient, while another reports that a 1,000-shot clinic requires 5-6 nurses to perform data entry for two days afterward since the system requires entry of 14 fields that are required by the federal government and another seven that the state added.
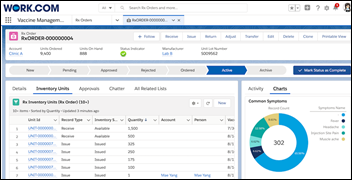
Salesforce announces Vaccine Cloud, which helps government agencies, healthcare organizations, and others deploy and manage their vaccine programs. Provider functionality includes inventory management, staff training, payment, and community communication for notifications and second-shot reminders.
The New York Times columnist Ezra Klein asks public health experts how to prepare for a 50% jump in COVID-19 contagiousness six weeks now because of the B117 variant, which could kill up to 300,000 more Americans:
- Increase the use of genomic sequencing to see how and where the virus is mutating.
- Don’t reopen restaurants and bars just because recent numbers are coming down.
- Avoid total lockdowns and instead get the FDA to speed up approval of rapid, at-home tests.
- CDC should give direct guidance on what kinds of masks to wear in various situations and the government should consider distributing high-quality masks.
Other
ECRI lists its top 10 health technology hazards for 2021:
- Managing medical devices that are marketed under FDA’s Emergency Use Authorization.
- Order entry mistakes caused by accepting partial names of drugs. ECRI recommends populating search fields only after the first five letters of the name have been entered.
- Revisit the quick rollout of telehealth to consider patient technology inequalities, user training, integration with other systems, and determining which patients are well suited for telehealth visits.
- Review imported N95 masks, especially KN95 masks from China, because they sometimes fail to provide the claimed level of protection.
- Avoid the use of consumer-grade monitoring devices in the acute care environment wherever possible, including pulse oximeters, blood pressure cuffs, and glucose monitors.
- Review the capabilities and use of UV disinfection devices, which are not usually regulated by FDA.
- Assess the capability of medical device vendors to manage the third-party software they use.
- Conduct a risk-benefit analysis of AI functionality to make sure that the data a system was trained on is representative of the organization’s population.
- Avoid remote operation of medical devices whenever possible in trying to conserve PPE, which can lead to less-frequent patient observation, placing devices where staff can’t see or hear them, and creating tripping hazards from hallway placement.
- Employ QA measures and clinician approval of 3D-printed devices.
Sponsor Updates
- WellSky-owned CarePort’s Interop interoperability solution is made available in Epic App Orchard to satisfy CMS’s April 30, 2021 Conditions of Participation requirement that hospitals notify a patient’s other providers of ADT activity.
- The HCI Group VP of Provider Delivery Will Conaway celebrates two years on the Forbes Technology Council.
- MHS will integrate its CareProminence platform with the Healthwise Care Management Solution for health education.
- LexisNexis Risk Solutions wins CyberSecured Awards from Security Today in the categories of fraud protection and threat intelligence.
- Cerner receives a fourth consecutive perfect score in the yearly Corporate Equality Index.
- Optimum Healthcare IT and the University of Colorado Denver partner to offer recent college graduates an apprenticeship pathway to high-paying healthcare IT jobs.
- Ellkay features Meditech’s Helen Waters in its Women in Health IT series.
Blog Posts
- Industry Alert: Urgent Care Named as Key Venue in Biden’s Vaccine Distribution Strategy (Experity)
- Four Predictions for Diabetes Management and Technology in 2021 (Glytec)
- Physician On-Call Scheduling is Changing – What You Need to Know (Halo Health)
- 2021 Revenue Cycle – What to Expect? (Healthcare Triangle)
- 5 key differences between consumer and enterprise biometrics (Part 1) (Imprivata)
- Vaccine Administration – And All That It Requires – Is Overwhelming Health Systems (HCTec)
- Healthcare Process Improvement: Six Strategies for Organizationwide Transformation (Health Catalyst)
- Scottsdale Institute CIO Summit Examines New Alignment for IT (Impact Advisors)
- Exploring the need for patient data normalization (Intelligent Medical Objects)
- How to Simplify Your Healthcare Worker Vaccination Program (LiveProcess)
- The 2021 JP Morgan Healthcare Conference & How Hospitals Stay Relevant After COVID (Loyale Healthcare)
- COVID-19 vaccination self-scheduling – why we’ve released our own vaccine management solution (Lumeon)
- Improving Operating Room Utilization (Medhost)
- Anticipate the unimaginable: 5 steps to mitigate crises (Meditech)
- 4 Essential Physical Therapy Themes to Watch in 2021 (MWTherapy)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.




“CACI wins a $96 million US Army task order to test, train, and deploy its MC4 battlefield EHR.”
Doesn’t the Army already have an EHR? Feels like something that would make Joe say “C’mon man!!!”
A country with “64 unconnected vaccine registries” must have at least 8 EHR for its army.
Vaporware?,
CACI contract is for support services, including integration, testing, training and implementing upgraded MC4 battlefield EHR, the Army EHR . At same time, efforts being made to integrate DoD and VA systems.
As a veteran of these HIS battles, and as a former Air Force Child too. 100% Integration seems like a no-brainer, right? So let’s go through the checklist, first the case For:
1). All the Armed Services ultimately report up through the Pentagon and the Joint Chiefs of Staff. There is a common chain of command and service integration, however that looks in detail;
2). There is a good case, IMO, for common functionality in an EMR/EHR. It should be possible to reconcile any differences too, without too many compromises;
3). The Armed Services have the money and skills to pull off a common EMR/EHR system;
4). The tech would fundamentally appear to be ready. In fact, the real world deployments of such tech also looks ready.
Now the case Against:
1). This is a big job! And in the IT world, bigger systems come with increased Project risk;
2). There are turf battles and culture differences between the various Armed Services. A lot of this boils down to ego competitions, the struggle for money and resources, and history;
3). A Battlefield EMR/EHR system, eh? This is a wrinkle. Your system will have security requirements and fault tolerance requirements. Maybe a bit more than usual, but honestly? This still looks entirely within reach. The architecture needs are not pie-in-the-sky;
4). The current VA system uses old tech but it’s familiar and safe. There are culture issues with upgrading to a newer system;
5). The new DoD system addresses the old tech of the VA system, but my understanding is, it’s not ready for battlefield deployment? My impression is, it’s only 20% or less deployed, and likely a LOT less than that. But I could be wrong.
My totally bogus and uninvolved assessment? Do it. Integrate the whole thing. It’s within reach and the benefits will outweigh the risks. Also, don’t deploy on the VA platform because that is designated Legacy. Cerner is the future here and you’ll avoid having to migrate to Cerner later.
Assuming you have been watching the DoD and VA deploy Cerner Millennium and HIE. This brings a consolidated EHR between them. VA just started their transition and rollout in Spokane.
Re Allscripts lawsuit – Ridiculous they had to go thru this kind of lawsuit. A recommendation is means nothing! Did someone get an offer they could not refuse? Or an Ultimatum? Now that would be something to deal with.
I can’t comment on the legality of Athenahealth’s actions, but athena absolutely offered both sponsored trips for prospects and referral deals with vendors of sunsetting EMR products. The only one I was unware of during my time there was payments for prospect referrals (although that’s hardly uncommon in the industry).