The sentence was "most people just go to Epic UGM" - that's people going to Epic's annual user conference and…
Monday Morning Update 4/13/20
Top News
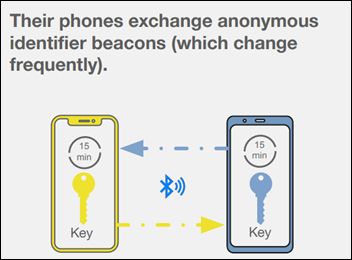
Apple and Google will enhance their mobile devices with an API that will use Bluetooth to perform coronavirus contact tracing to help detect outbreaks.
The companies will release APIs next month that create interoperability between Android and IOS devices using apps from public health authorities. Following afterward will be the release of the full contact tracing platform.
The use scenario is this:
- User One carries their phone any time they’ are in public. They leave the app running.
- User One is assigned an anonymous, frequently changed identifier beacon.
- User One has close contact with User Two, who is also carrying their phone and running the app.
- User One tests for COVID-19. They manually enter their result into an app provided by a public health authority.
- User One gives their phone permission to upload a 14-day history of the identifier beacons with which they have had close proximity.
- User Two’s phone regularly downloads a list of identifier beacons from contacts who have tested positive.
- User Two’s phone alerts them that they have been exposed to someone who tested positive and tells them what they should do.
Obvious weak points of cellphone-based contact tracing:
- Adoption in other countries that have tried this voluntary approach has been low (Apple and Google did not acknowledge that this technology wasn’t their original idea).
- The app must be left running and the user must carry their phone everywhere.
- The users must have smart phones; those with flip phones or no phones cannot participate.
- Each person who tests positive must remember to enter their result.
- Both contacts must be running the app. That means, given likely low adoption, that the odds of detecting a given exposure are tiny.
- Bluetooth can detect proximity, but not the chances of exposure. It could record a contact anyone in nearby car or everyone behind doors in a hospital hallway.
- People who don’t trust big companies like Apple and Google (especially the latter, given that its primary business model is using or selling user data), or who detest the concept of mass surveillance regardless of benefit, will likely opt out.
- Public health systems must participate.
- The US still lags in testing and results from some labs are delayed due to backlogs.
Reader Comments
From Code Jockey: “Re: Epic consulting. Demand for my skills has evaporated as health systems have suspended EHR projects and cancelled contracting engagements. Given the 95% reduction in air carrier routes through September, there’s no way to get to their sites even if they need contractors. I’m now unemployed and trying to get a $17 per hour job at an Amazon warehouse. I’m wondering what people like me are doing – taking a break, shifting to other industries, or working remotely? What will consulting look like when this is all over, the former Monday to Thursday travel or 100% remote work? You also have Epic continuing to elbow into the contracting space. I wonder how the many staffing firms that have lined their pockets on the backs of contractors will be affected by the absence of engagements?” I offered to create a short survey for consultants to anonymously share how the pandemic has changed their work. Your thoughts might relieve some anxiety for people who are cooped up with little work available short term.
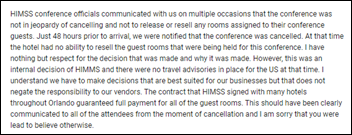
From Financial Cannula Insertion: “Re: HIMSS20 hotels. Marriott Orlando Village is not refunding guests because they claim they were contractually guaranteed full payment by HIMSS. They’re keeping my ‘deposit’ of the full four nights that I prepaid. Here’s the email I received from the hotel GM.” The hotel says that HIMSS told it on multiple occasions that the conference would not be cancelled and asked that the hotel not release or resell any booked rooms. The hotel add that since the US had no travel advisories in place at the time the conference was cancelled (two days before FCI’s scheduled arrival), the cancellation was a HIMSS business decision that does not relieve it of honoring its vendor contracts. The GM says HIMSS signed a contract with all the Orlando hotels guaranteeing the attendee’s full payment. It’s interesting that HIMSS can legally guarantee payment terms on behalf of the actual customer, presumably by the online reservation terms specified by OnPeak since HIMSS doesn’t handle room bookings directly.
From Spumoni: “Re: HIMSS. I’m struggling with a path forward, as exhibitors seemed to be saying in your survey. Will travel return? Do I really want to sit shoulder-to-shoulder in sessions? Was the conference a boondoggle all along that was self-aggrandized by vendors along with their own importance? Meanwhile, I’m being bludgeoned by the pivot to online content delivery and life in the glow of Webex on a laptop.” It’s hard to predict the pent-up, post-isolation demand for big conferences in the potential absence of a coronavirus vaccine. People were always returning home sick even in past years, as my post-HIMSS18 poll found that 50% of respondents came home with a cold, flu-like symptoms, stomach problems, fatigue, headaches, or muscle aches. Beyond that is the economic question — is the considerable cost of attending and exhibiting worth it, especially given a year off to contemplate the value received? Or will it go back to exhibitors who mostly show up for fear they will look bad competitively if they don’t? Or will the conference irrecoverably lose critical mass with the near-certainty of fewer attendees, a sparser exhibit hall, and attendees who have grown comfortable conducting all aspects of their work remotely?
From Allscripts Sunset: “Re: Allscripts. Appears that it just hit five straight quarters without selling a Sunrise new logo deal.” Unverified.
From Allscripts Cuts: “Re: Allscripts. Word is that the board gave Black and Poulton six months in early March to cut $100 million per year in expenses. There was an expectation of laying off 1,000 to 1,500 people, but they likely used COVID to cut pay and travel to get layoffs into the 500-600 range. That will work only until full salaries return and travel picks back up.” Unverified.
HIStalk Announcements and Requests
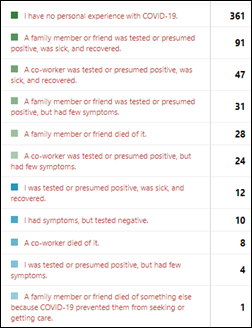
Most poll respondents have no personal experience with COVID-19, and thankfully few report the death of a family member, friend, or co-worker.
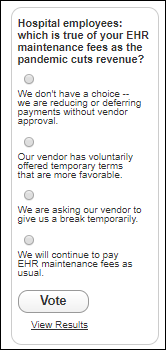
New poll to your right or here, for hospital employees: which is true of your EHR maintenance fees as the pandemic cuts revenue? Click the poll’s Comments link after voting to explain.
Listening: Bachelor Girl, which I discovered while creating another playlist for my young friend (it includes Dua Lipa, James Bay, Florrie, Sia, and Hazel English). Bachelor Girl is an Australian duo that has been around for nearly 30 years, and what caught my attention was 1999’s “Lucky Me,” a cynical take on success that sounds more Nashville than Melbourne (it’s amazing that the lyric way back then says, “I’ve got so many friends on the internet, I could never be alone.” I’m also thrilling to the new album of the amazing Public Enemy and the best voice in rap, Chuck D, who raises goose bumps on 2007’s “Harder Than You Think.”
A third-hand acquaintance (well educated, upper class, long list of health conditions) is experiencing cough, fever, and fatigue and was reluctantly sent home by his employer. Some of his co-workers – who as essential workers spend their work days in close office contact — have since tested positive for COVID-19. He has dawdled in sending in his own test samples and continues to convene multi-generational family and neighborhood gatherings and takes regular, unmasked trips to grocery and hardware stores. Bill Gates was right in describing STDs – it would be easy to stop communicable disease outbreaks if those who practice bad behaviors suffered the consequences immediately instead of later or didn’t harm others in the process of doing something stupid.
Health-Related Technologies That the Pandemic Has Made (Or Will Make) Mainstream
- Telehealth and its integration with EHRs.
- 3D printing of medical supplies.
- Chatbots that can help keep the worried well out of the ED (instead of the previous model of hoping to bring them in as paying customers).
- Remote patient monitoring and clinician backup.
- Videoconferencing and team collaboration platforms.
- Patient engagement for monitoring patients who are recovering at home or who can be discharged to lower-acuity settings.
- Patient check-in and waiting room avoidance.
- Public health reporting and data aggregation.
- Online education.
- Predictive models for hospital resource needs, patient outcomes, and pandemic spread.
- Virtual conferences.
- Clinician collaboration platforms for sharing best practices and crowdsourcing treatment options.
- Robotics for contact-free hospital room deliveries.
- Rapid online publication of research findings.
- Syndromic surveillance.
- Virtual mental health services.
- Medical equipment clearinghouses.
- Contact tracing.
- Virtual programs for home exercise, rehabilitation, and wellness.
- Imaging AI for detecting specific conditions.
- Analytics and predictive modeling.
- Supercomputer-powered rapid drug and vaccine research.
- Wearables and mobile devices for the rapid assembly of clinical study cohorts and collection of study data.
- Platforms to connect people with social services.
- Voice assistants, such as Alexa and Siri, that have been enhanced with tools to answer specific health questions or to allow summoning help.
- Apps for relaxation and mindfulness for people who are quarantined and anxious.
- Ordering and delivery apps for food, supplies, and prescriptions.
- Platforms for matching clinicians and volunteers with hospitals in need.
- Internet-connected digital thermometers for outbreak detection.
Got more to add?
Webinars
April 15 (Wednesday) 1 ET: “Scaling front-line COVID-19 response: virtual education, screening, triage, and patient navigation.” Sponsor: Orbita. Presenters: Lawrence “Rusty” Hofman, MD, medical director of digital health, Stanford Health Care; Kristi Ebong, MPH, MBA, SVP of corporate strategy, Orbita. The presenters will describe how chatbots can be quickly deployed to streamline individual navigation to the appropriate resources, administer automated virtual health checks for monitoring and managing specific populations, increase access to screening and triage for high-risk populations across multiple channels (web, voice, SMS, and analog phone), and reach individuals in multiple languages.
April 28 (Tuesday) 1 ET: “COVID-19: Managing an evolving patient population with health information systems.”Sponsor: Intelligent Medical Objects. Presenters: Julie Glasgow, MD, clinical terminologist, IMO; Reeti Chauhan, senior product manager, IMO. IMO recently released new novel coronavirus descriptors to help clinicians accurately record diagnoses and also created free IMO Precision COVID-19 Sets to help identify and analyze patients with potential or documented infection. The presenters will discuss these new tools and describe how to use them optimally.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
People

MaineHealth SVP/CIO Marcy Dunn died last Monday. She was 65.
Announcements and Implementations
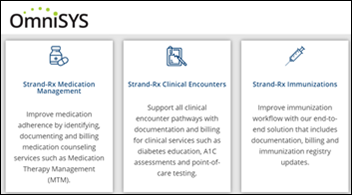
OmniSys offers all pharmacists — who can now administer COVID-19 tests as authorized last week by HHS — free online training that describes how to order tests, apply for a state license, perform the nasal swab, bill payers, submit positive cases, and share the results with the patient’s other care providers. The company has also enhanced its cloud-based retail pharmacy EHR with tools for documentation, reimbursement, and care plan communication.
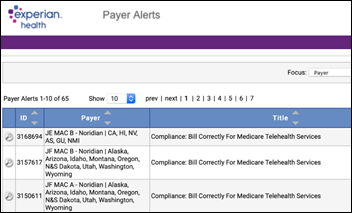
Experian Health offers a free, regularly updated list of COVID-19 and telehealth payer polity alerts for hospitals, medical groups, and pharmacies, describing 1,140 changes in medical coverage policy changes.
COVID-19
New York City reports that only 18,500 of its hospital beds are being used versus the 140,000 that experts feared would be required during the pandemic’s peak resource demand that happened this weekend. Hospitals are seeing declining ICU bed occupancy, hospitalizations stand at under 19,000, and the 2,800-bed emergency hospital that was created at Javits Center is treating just 300 patients. Officials credit residents of New York and nearby states for slowing the tide by staying home. Statistical experts say their surge projection models were likely thrown off by unreliable data from China and shorter than expected ICU stays. Meanwhile, physicians worry that the big drop-off in patients who normally seek hospital care for heart problems and strokes may indicate that they are fearful of going to the ED and are just suffering at home instead, possibly to their long-term detriment.
Mayo Clinic says that a COVID-triggered freeze on elective surgeries will trigger a $3 billion loss this year, forcing it to implement pay cuts and furloughs for salaried employees, freeze hiring, lay off contract employees, and stop some construction.
Politico reports that Democratic lawmakers have written to White House Senior Advisor Jared Kushner to express concerns about the patient privacy implications of his rumored discussions with technology companies to collect COVID-19 public health surveillance data. A White House task force wants to develop a national coronavirus surveillance system that would provide a real-time view into hospital ED visits and bed capacity using “multiple private sector databases,” raising fears of a Patriot Act type encroachment on privacy. A government spokesperson says that neither Kushner nor the White House are aware of such a project, but Politico uncovered a memo written by three companies – Collective Medical, PatientPing, and Juvare – that Politico says was in response to an administration request on the feasibility of quickly gaining visibility into how many patients are seeking hospital care.
The federal government’s distribution of the first $30 billion in emergency hospital grants raises the ire of some hospitals because payments are based on the volume of past Medicare billing amounts, not their coronavirus burden. Hospitals in lightly hit states, some of which continued to perform rofitable elective procedures, are being given 25 times the amount of money per COVID-19 case as those in New York. The formula also provides payments to providers who aren’t on the front lines, such as podiatrists and ophthalmologists. HHS said the goal was to get the money out quickly and it will focus the next round on providers who were most impacted by coronavirus.
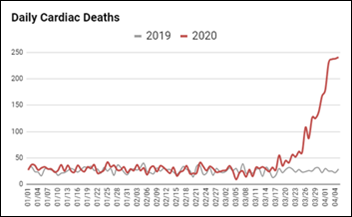
More evidence that New York City is unintentionally undercounting COVID-19 deaths – FDNY reports that cardiac arrest calls and DOAs have risen six-fold over the same period last year, which probably means that people who die of COVID are being counted instead as cardiac deaths. Italy saw the same six-fold increase in deaths, far more than the official COVID death counts.
A single long-term care facility in Virginia has recorded 40 deaths that are linked to COVID-19, with the medical director blaming lack of staff and equipment, low funding, and trying to isolate positive cases when people have lived in the same room for years. The facility is owned by private equity firm Tryko Partners, which operates 3,000 skilled nursing beds.
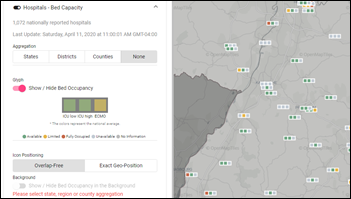
The US federal government is using daily, e-mailed hospital worksheets to visualize bed capacity, but Germany has a live map.
Florida is underreporting COVID-19 deaths because the state health department has decided to count only deceased state residents, omitting snowbirds and tourists who die in Florida.

United Airlines and basketball player Steph Curry honor the 20 USCF clinicians who volunteered to serve on the front lines of New York City hospitals.
Other

The 3,000-bed temporary hospital that was created in Chicago’s McCormick Place convention center will use Epic in a partnership that involves Epic, Rush University Medical Center, and the City of Chicago. Chicago’s Department of Health reached out to Epic early in the planning.
This seems HIMSS20 related and perhaps could be instructional to HIMSS. Burning Man Project cancels its annual Black Rock City gathering for 2020 due to coronavirus and will instead run a virtual version that it says “will likely be messy and awkward with mistakes.” It asks ticket-holders to consider donating part of their full refund to the project so it can continue to support its key programs, noting that “things are looking a little grim” in trying to run year-round programs when 90% of the project’s annual income comes from Black Rock City. Tthe group has already undertaken layoffs and pay cuts. Burning Man also observes that rolling over this year’s ticket sales as a credit for next year’s event is not practical because that simply “punts the financial challenges to a future date.” The group had cancellation insurance, but it doesn’t cover pandemics. The CEO recorded a personal, heartfelt message to explain the situation, an approach of unscripted humility and openness that stands in contrast to the HIMSS “strictly business” approach that makes it feel more like an us-versus-them vendor than a non-profit that wears its lofty societal aspirations on its suit sleeve. I’m not sure how many HIMSS members and exhibitors feel a personal attachment or loyalty to the organization or its goals as its global ambitions and expansion strategy has made it impossible to define a typical member.
Sponsor Updates
- MDLive reports visits and user registrations increase to all-time highs with virtual healthcare as first-line defense in fight against pandemic.
- Clinical Computer Systems, developer of the Obix Perinatal Data System, launches the “Clinical Concepts in Obstetrics” podcast.
Blog Posts
- The Downstream Impact of COVID-19: Building a Strategy with Telehealth and Chronic Care Management (Lightbeam Health Solutions)
- Using LiveProcess for COVID-19 Response: Real World Tips from Our Customers (LiveProcess)
- Healthcare organizations implement remote testing in light of COVID-19 (Meditech)
- Remote Healthcare Work: Best Practices amid COVID-19 (Health Catalyst)
- Leveraging Virtual Care Amid COVID-19 (Netsmart)
- Building a Healthcare Data Strategy with Big Rocks (Omni-HealthData)
- Social Distancing and the Power of Patient Engagement (PCare)
- Automation can help track active coverage during the COVID-19 chaos (Experian Health)
- 12 tips to manage a remote contact center in healthcare (Spok)
- Backfilling for clinical team members redeployed to the front lines (Nordic)
- Tips for Educating & Communicating with Patients During the COVID-19 Pandemic (PatientBond)
- Pivot Point Perspective: 6 Strategies to Accelerate EHR Build Outs for Drive-Thru Clinics (Pivot Point Consulting)
- Enabling Workforce Continuity – It’s Time to Rethink Identity (SailPoint)
- How to Improve Physician EHR Adoption During an Implementation: Part 2 (Santa Rosa Consulting)
- 6 ways to maintain your well-being during a pandemic (StayWell)
- Healthcare’s catastrophic revenue gap is here. Accelerate recovery now. (SymphonyRM)
- Cloud-hosted communications for makeshift care areas. (Voalte)
- COVID-19: 6 Simple Tactics for Safer, More Efficient Communication (Vocera)
- How to Deliver, Document, and Bill for Different Types of Remote Rehab Therapy (WebPT)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



One small item to your wish list…healthcare for all, from birth to grave.
The total $ cost of such a plan is going to be small change in comparison to the COVID costs.
The relative cost of universal healthcare to COVID remediation is only relevant if universal healthcare would have prevented the spread of the coronavirus. Last I checked, everywhere with universal healthcare is also struggling with this pandemic.
Universal healthcare doesn’t have much impact on the spread of disease, but it is certainly nice to know you won’t go bankrupt from bills or lose your job. Many in the United States will lose their insurance coverage because of COVID, or need to pay for COBRA without having a job. This summer I fully expect a series of articles on people got surprise bills for COVID-related treatment, or at least treatment in the time of COVID that they thought was supposed to be covered. Countries with universal healthcare also tend to have other strong social programs. Compare the unemployment rate in the US v Europe right now. It will be interesting to compare the economic recoveries.
I think (/hope) we can all agree that this episode highlights the inherent weakness in chaining health insurance to employment.
IMHO the Federal and State Governments should be picking up 100% of the tab for this one.
How about the cost of COVID treatment under universal systems vs the us system? Not many people have gotten the bill from their doctor or insurer yet.
Cardiac vs COVID death count.
In these cases COVID was the ‘straw that brook the camels back”. I would give both maladies equal weight. It’s likely the person would not have died with out either problem. Once this pandemic passes it would be very enlightening to analyze the impact co-morbidity and complications, versus none.
To add to your list of technologies that (we hope) will mainstream: Truly interoperable health records that don’t require any additional burden for providers and use technology to fill the gap
Add to list
* Workflow automation tools
* Virtual medical assistants
* Virtual primary care
* Physical exam proxy (eg mobile phones for vitals, stethoscope, otoscope, and of course pictures and video)
* AI based diagnosis tools via mobile phone data (sounds, pictures, utilization), eg Depression, Covid cough, Sinus infection, Rashes…
* Home-based lab testing (direct at home or send in)
etc…
How about Patient Contact Management, but perhaps this already exists? The study of which physical surfaces a patient touches, and the elimination or modification of that surface to reduce disease spread. Yea, this already must exist…right?
A form of immunity status/ serology/ vaccination status digital passport, for work, school, travel, public event participation
As someone in a country with universal healthcare, I am looking at the US and seeing a country with an economy that may well collapse as a result of a healthcare system that has long been considered by outsiders as bizarrely expensive and horribly inequitable. From here, you look to be in real trouble. Your time as a/the global superpower may actually soon end as a result of the nation’s failure to provide healthcare for everyone who needed it. Big stuff, yes, but am I wrong? I hope so.
And your economy is currently thriving?
The presence or absence of universal healthcare is not the determining factor in what is going on right now; the determining factors are the complete absence of a scientifically-informed Federal response, and an economy that relies on hourly wage labor in service industries, and minimal to no infrastructure to support us when those industries evaporate overnight.
People’s ability (or inability) to pay for the treatment they receive if they become infected is a separate factor, and is significant in its own right, but is not the reason our economy just cratered.
I agree with what you (both) say. Certainly our economy is screwed for similar reasons. But – bear with me – at least we know the health system will take care of us. It’s hard to describe how grateful we are to have free healthcare. Throughout our lives we have been able to go to the GP or hospital and receive free, high quality care, without question. Years ago my grandmother received a hip replacement and radiology for age-related breast cancer in her 80s – for free, of course. She lived healthily well into her 90s. I was deeply moved at that time and felt it showed that we were a kind country. It provides genuine comfort. I wish you had it in the US. You have a right to it, especially given your healthcare expenditure. Wishing you all the best.
We do have that. It is just only for old people and the military. The rest of us have to fight for whatever scraps the large corporations throw to us.