Yes! Flip flops are essential as the back up for professional footwear. Plus they are easy to put into your…
News 3/27/20
Top News
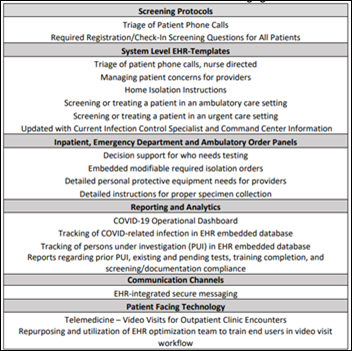
UC San Diego Health providers and researchers describe the tools they created in Epic to address COVID-19, including screening protocols, EHR templates, order panels, analytics, secure messaging, and video visit support.
HIStalk Announcements and Requests
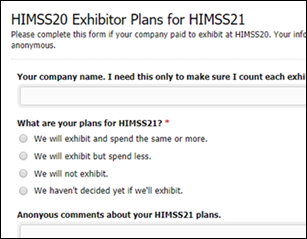
Three dozen companies that paid to exhibit at HIMSS20 have completed my survey to indicate their plans for exhibiting at HIMSS21. I’ll leave the survey open for another day or two, then summarize the responses — which include their detailed comments and observations — over the weekend. HIMSS20 exhibitors, please take a few seconds to jump in.
Listening: reader-recommended FKJ & Masego, who just fired up their instruments and free-styled a one-off electronic jazz composition that is pretty amazing and perfect for working from home background music. It gives me hope that while technology can enhance the creative process of talented individuals, it doesn’t have to replace it.
Webinars
None scheduled in the coming weeks. Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Moxi hospital robot maker Diligent Robotics raises $10 million in a Series A funding round.
People

Orlando Health names Marshall Denkinger, MD (Centura Health) to the new role of chief medical information and information technology / clinical engineering innovation officer.
Announcements and Implementations

In Australia, Melbourne Health postpones its $75 million Epic implementation at three facilities as it focuses on treating COVID-19 patients.
Government and Politics
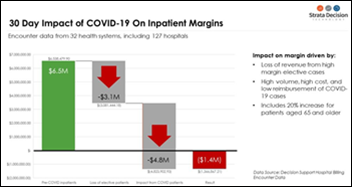
A Strata Decision technology model of US health system shows that health systems will lose an average of $2,800 per COVID-19 case without an increase in Medicare reimbursement, with some of them likely to lose up to $10,000 per patient. Some of the higher cost involves nurses having to help each other with personal protective equipment, expanded room cleaning requirements, higher use of radiology procedures, and increased drug and supply costs.
The US coronavirus shutdown triggered 3.28 million new first-time unemployment claims last week, five times that of the previous highest week in 1982. A former Department of Labor chief economist say she expects 14 million Americans to lose their jobs. The number of healthcare-uninsured surely went up quite a bit in tandem.
COVID-19
US COVID-19 deaths topped 1,000 on Thursday. Elmhurst Hospital Center (NY) had 24 deaths in 24 hours. New York EMS took 6,400 medical 911 calls on Wednesday, its highest number ever in exceeding the volume of September 11, 2001. New York State has 5,300 hospitalized patients and 1,290 ICU patients.
Epidemiologist Neil Ferguson, leader of the Imperial College London team whose grim COVID-19 projections got the attention of the UK and US governments a couple of weeks ago, issues brighter projections in which he expects that NHS will be able to cope with the expected peak of the epidemic in 2-3 weeks. His latest computer simulations — which take into account NHS’s capacity increases and restrictions on civilian movement – indicate that the country’s ICU beds will not be overwhelmed. Most remarkably, he has reduced his original UK estimate of 500,000 deaths to less than 20,000 and says that number could go much lower, adding that half of that expected total would have been older, sicker patients who would have died even without COVID-19. Ferguson had originally called for a quarantine of 18 months or more, but now says it looks like the virus spreads faster than expected, meaning that a lot of people have been infected without major issues. Ferguson was diagnosed with COVID-19 shortly after publishing the original report.

Prisma Health (SC) receives emergency approval from the FDA to use an internally developed ventilator expansion device that allows one ventilator to be used for up to four patients. The health system has made the source code and 3-D printing specifications available for free here.
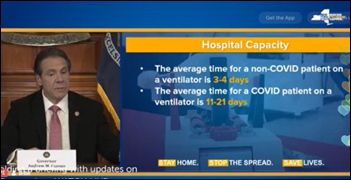
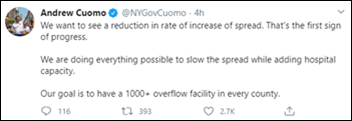
New York Governor Andrew Cuomo says COVID-19’s strain on hospitals should be thought of in “ventilator days” given that a ventilated patient may require intubation for up to three weeks.

Emile Bacha, MD, chief of Columbia’s cardiac, thoracic, and vascular surgery department, writes in a letter to colleagues that the hospital is struggling with being forced to ration care for pediatric cardiac surgery patients since the department has just one OR team, causing anxiety in the families of children who need surgery for septal defects a and heart valves. He says one cardiac surgeon and several cardiologists are sick with COVID-19 and that unlike long OR hours that create a positive result, the mixing of triage, ethics, and medicine is a mentally negative form of exhaustion.
The Federation of Sate Medical Boards offers free access to its physician database so that hospitals can easily verify physician credentials as they attempt to prevent staffing shortages.

In the UK, vacuum cleaner manufacturer Dyson develops a ventilator within 10 days of being asked by Prime Minister Boris Johnson to help out. The company says the CoVent can be manufactured quickly to fulfill the government’s orders for 10,000 of the ventilators. Billionaire founder John Dyson will also donate 5,000 more units.
A Premier survey of 260 health systems conducted from March 16-20 finds that N95 respirators are their most pressing supply need, followed by hand sanitizer and surgical masks. Shortages of isolation gowns, viral swabs, and ventilators were also areas of concern.
Hospitals consider making all COVID-19 patients “do not resuscitate” regardless of family wishes because of the risk to staff who don’t have access to protective equipment.
The White House is reportedly preparing to assign each US county a color-coded COVID-19 risk status of low, medium, or high, to be optionally used by state governors in assigning or reducing mitigation measures. President Trump has said that business should return to normal in areas that haven’t had outbreaks and that it’s not necessary to perform widespread testing in those states.

New York State seeks IT volunteers for COVID-19 technology SWAT teams, specifically looking for expertise in product management, development, hardware deployment, and data science. The state is hoping to recruit teams from tech companies, universities, non-profits, and research labs for 90-day service deployments.
A ProPublica investigative report finds that the CDC’s early response to coronavirus was chaotic and inconsistent, when it issued incomplete or conflicting guidance to public health agencies, rolled out buggy electronic questionnaires for screening airline passengers, and resorted to using Google Translate in airports due to a shortage of interpreters. A January 28 email from CDC Director Robert Redfield, MD said the virus was not spreading in the US and thus CDC concluded that the risk to the American public was low.
Other

Cleveland Whiskey pivots to producing hand sanitizer for Cleveland Clinic.
Developers come together to create a Slack channel for physicians who are eager to share experiences and advice during the pandemic.

Epic partners with a local childcare provider to convert the use of its former headquarters in Madison, WI to childcare space for UW Health employees. The company will also provide food services.

The Scripps Research Translational Institute partners with health data aggregation company CareEvolution to launch an app-based study that will use health data from wearables to more quickly pinpoint the onset of viral illnesses like the flu and coronavirus.

Bloomberg looks at the ways physicians are using social networks to share information about COVID-19, sometimes straining Facebook’s capacity to the point that its engineers have to fix click-to-join group codes.
The Onion works best under time pressure, and in this case, it was prescient – GoFundMe’s coronavirus-related funding requests jumped 60% in a handful of days with requests from families who are unable to afford coronavirus-related hospital bills and funerals as well as those from the newly unemployed.
Sponsor Updates
- Pivot Point Consulting names Andy Palmer director of its EHR practice.
- Hayes Management Consulting postpones its 2020 MDaudit User Group Meeting to October 29-30 in Chicago.
- InterSystems releases a new version of its Iris Data Platform.
- CPSI offers users a COVID-19 Toolkit, which includes chatbots and WHO/CDC information, that it developed by QliqSoft.
- CalvertHealth monitors coronavirus cases using Meditech’s Business and Clinical Analytics Solution.
- Imat Solutions offers customers real-time data reporting and analytics in response to COVID-19.
- Intelligent Medical Objects makes IMO Precision COVID-19 value sets freely available to customers.
- Wolters Kluwer Health publishes an interactive COVID-19 search intensity map using its UpToDate clinical decision support tool.
- Impact Advisors posts audio from a teleconference titled “Operationalizing Telehealth for COVID-19.”
- Elsevier launches Veridata Electronic Data Capture for clinical trial research, and offers free access to help researchers studying COVID-19.
- Nuance offers Dragon Medical users free COVID-19 documentation templates
Blog Posts
- TeleVisits: How Fast Deployment Helps (EClinicalWorks)
- Case Management and Discharge Resources During the Coronavirus Pandemic (Ensocare)
- Dr. Bruce Bode Looks Back and Forward at Automated Glucose Control Systems in Hospital Settings at ATTD20 (Glytec)
- How to Report on Remote Worker Activity and Key Performance Indicators (Goliath Technologies)
- Google Cloud Named a Leader in the Forrester Wave for Public Cloud Development and Infrastructure Platforms (Google Cloud)
- Mastering Digital Distance with Daily Huddles (The HCI Group)
- Mission: Not Impossible (Healthfinch)
- Managing Anxiety During the COVID-19 Outbreak (Healthwise)
- COVID-19 Telehealth Considerations (Optimum Healthcare IT)
- What does a messy basement have to do with information management? (Hyland)
- COVID-19: Best Practices from the Front Line (Impact Advisors)
- COVID-19 – Our house is on fire (Imprivata)
- Supporting our employees while navigating the new normal (Intelligent Medical Objects)
- Meditech stands with providers in the fight against COVID-19 (Meditech)
- How TeleVisits Can Help During a Health Crisis (EClinicalWorks)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



NY bed shortage??
For over forty years the State of NY (and many other states) has beaten hospitals up via a payment system that pushed/ punished them to close beds. The mantra from Cuomo (father and son, and other Govs) was close those excess beds or be financially punished.
Well the Govs got their wishes… be careful what you wish for, or better yet….what goes around comes around!
That’s a fair point. But I think the way to be prepared for a once-every-100-year event is not by maintaining a large, expensive and underutilized permanent bed capacity, but having detailed plans and the necessary supplies/materials to expand temporarily in an emergency.
In spite of clear history and warnings from epidemiologists, we don’t seem to have done a very good job preparing for this eventuality at the organization, state or national level. I’m not saying the challenges aren’t herculean – just that they should not have come as a surprise.
Hospitals for decades ran at 60% occupancy, based on commercial standards (85%) this was deemed terribly wasteful, so pressure mounted to eliminate beds, even tough the beds were not staffed and were only a minor fixed expense.
Regulators at both the federal and state level claimed this would save billions of healthcare dollars. Beds were eliminated but the savings never materialized. So the question now is are we spending more to create ’emergency virus’ beds than we saved? I believe that is what is happening.
In healthcare a big fixed expense is always the standby costs. If you eliminate these costs in the interest of reaping immediate savings then the adage: Pay now or pay latter, but you will pay…truly applies.
I don’t remember that happening. An alternative way to phrase what happened: Regulators pointed out that some care that was happening in hospitals was also happening in ambulatory or outpatient settings and that the care was being delivered in a much more cost effective way outside the hospitals. So regulators lowered reimbursement levels for that care towards the outpatient cost and hospitals cut those services in response. A more charitable interpretation is that regulators did not claim to be eliminating beds but rather trying to improve access to care across the system by lowering overall costs as costs are the primary barrier to access in the US healthcare system.
I agree with Surprised that there are more efficient ways of dealing with pandemics than maintaining hospital beds. For example, we’ve know that airborne viruses are the most likely to become pandemics and a large subset of airborne viruses will require us to have stockpiled ventilators and protective equipment. If we can’t do even do that pretty easy task, I don’t think we have the capacity to maintain large numbers of unfilled hospital beds.