Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…
Monday Morning Update 6/10/19
Top News
A physician’s New York Times opinion piece says corporatized healthcare is cynically taking advantage of the professionalism of doctors and nurses by assuming they will work extra hours without extra pay, with the biggest overtime culprit being the EHR.
The article concludes,
In a factory, if 30% more items were suddenly dropped onto an assembly line, the process would grind to a halt. Imagine a plumber or a lawyer doing 30% more work without billing for it. But in healthcare, there is a wondrous elasticity — you can keep adding work and magically it all somehow gets done. The nurse won’t take a lunch break if the ward is short of staff members. The doctor will “squeeze in” the extra patients. The EMR is now “conveniently available” to log into from home. Many of my colleagues devote their weekends and evenings to the spillover work.
The author, internist Danielle Ofri, MD, PhD, also notes that the number of healthcare administrators increased 3,200% from 1975 to 2010, leaving healthcare with 10 administrators (and their salaries) for each doctor.
The always-thoughtful reader comments, many of them from clinicians, nearly all criticize the EHR and the transformation of healthcare from a calling to a greedy business dominated by mega-corporations whose richly compensated executives are rarely clinicians.
HIStalk Announcements and Requests
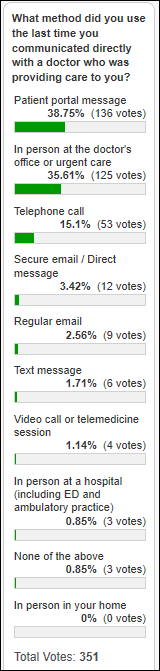
The most recent method use by most poll respondents to communicate directly with their doctor was patient portal messaging and in-person conversation, with telephone calls coming in a distance third and all others methods registering a negligible number of responses.
New poll to your right or here: What college education would be required of a candidate for your job title? I upset the longstanding apple cart at a previous employer by requiring two of my managers – hired before I came on board — who did not have college degrees to either start a degree-seeking program or accept a demotion since their job descriptions required it. It’s either a requirement or it isn’t, and in our case, it was, even though a wishy-washy predecessor had promoted them without it. On the other hand, good job candidates don’t necessarily possess degrees and employers often require those credentials only to reduce the number of applications they have to read. Worst of all are companies that waffle their job description language with “should have” or “preferred” rather than “must have” – the job description should describe only those credentials required to earn further resume review or an interview.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre for information.
Acquisitions, Funding, Business, and Stock
Switzerland-based medical Internet of Things vendor Medisanté enters the US market with the opening of an office in Bridgewater, NJ.
Sales
- Integris Health chooses Health Catalyst’s Data Operating System for enterprise-wide performance improvement.
Decisions
- The Mary Black campus of Spartanburg Medical Center (SC) will go live on Epic this month.
- Baylor Scott & White Medical Center – Grapevine (TX) will go live on Epic in 2020.
- Surgeons Choice Medical Center (MI), which replaced CPSI with Athenahealth in December 2017, will move back to CPSI this month.
- Advanced Surgical Hospital (PA) will remain with CPSI instead of moving to Cerner because of cost considerations.
These provider-reported updates are supplied by Definitive Healthcare, which offers a free trial of its powerful intelligence on hospitals, physicians, and healthcare providers.
People

Scott Hill (Allscripts) joins Change Healthcare as VP of strategic accounts.

Geisinger hires David K. Vawdrey, PhD (New York – Presbyterian Hospital) as chief data informatics officer.
Announcements and Implementations

Mobile Heartbeat adds secure mobile video chat to its MH-CURE clinical communication platform for face-to-face team member collaboration. Use cases include diagnosis, specialist consults, remote huddles, and staff training. It supports cross-platform use between Android and IOS devices. Meanwhile, Yale New Haven Health’s Bridgeport Hospital goes live on MH-CURE in all units, integrated with caregiver assignments in Epic and alarm management with Connexall.
Clinical Computer Systems, Inc., which offers the Obix perinatal data system, announces the BeCA Fetal Monitor and the Freedom wireless transducer solution that allows cable-free monitoring during labor.
Healthcare Growth Partners summarizes the health IT funding themes for May 2019 as fitness technology manufacturers, telemedicine-related companies, and vendors of patient engagement technology.
Other

Another female novelist’s New York Times editorial calls for curtailing the wellness industry:
The diet industry is a virus, and viruses are smart. It has survived all these decades by adapting, but it’s as dangerous as ever. In 2019, dieting presents itself as wellness and clean eating, duping modern feminists to participate under the guise of health. Wellness influencers attract sponsorships and hundreds of thousands of followers on Instagram by tying before and after selfies to inspiring narratives. Go from sluggish to vibrant, insecure to confident, foggy-brained to clear-eyed. But when you have to deprive, punish, and isolate yourself to look “good,” it is impossible to feel good. I was my sickest and loneliest when I appeared my healthiest.
A women and children’s hospital in Australia doubles its antenatal pertussis vaccination rate after changing the optional “did you offer the vaccine” clinician EHR dropdown field from optional to mandatory.
Sponsor Updates
- Gartner includes Lightbeam Health Solutions in its report, “Healthcare Payer CIOs, Leverage Vendor Partners to Succeed at Clinical Data Integration.”
- Waystar will exhibit at the Homecare Homebase Annual Users Conference 2019 June 12-14 in Dallas.
- NextGate publishes a new case study, “Enterprise Patient Matching Helps KeyHIE Establish Integrated Network of Accurate, Accessible Health Records and Drive Down Duplicate Record Rate to Less than 1%.”
- Nordic, Surescripts, and Vocera will exhibit at the Epic Michigan User Group Conference June 10 in Ypsilanti.
- Clinical Computer Systems, developer of the Obix Perinatal Data System, adds Stephanie Martin, DO to its executive advisory board.
- Recondo Technology partners with analytics vendor VisiQuate to reduce claim denials and shorten the process of correcting and resubmitting them to payers.
- DoD program Employer Support of the Guard and Reserve honors CloudWave with its Pro Patria Award for its support of Guard and Reserve employees.
- PreparedHealth will exhibit at CMSA June 10-14 in Las Vegas.
- Redox will exhibit at the Innovation Conference 2019 June 13 in Santa Fe.
- Relatient publishes a new case study, “Seven Hills Women’s Health Centers Recover Over 1,300 Patients to Bridge Gaps in Care Using Automated Health Campaign.”
- Sansoro Health releases a new 4×4 Health Podcast, “America’s Opioid Crisis: How IT Enables Better Care.”
Blog Posts
- Triple Threat: How Technology, Training, and Tenacity Transformed a Hospital Contact Center (Spok)
- The Big Money is Betting on Healthcare. What That Means for Providers and Patients (Loyale Healthcare)
- 6 easy ways physicians can use social media to advance their practice (Meditech)
- EHR Flaws and Fixes (Medicomp Systems)
- Are You Ready for Reimbursement Changes? (Netsmart)
- The Case for Outsourcing Your Level 1 Support: Why it Helps (CereCore)
- Are you giving too much care away for free? (Experian Health)
- How to Win Over Millenial Patients (PatientBond)
- Care Coordination Spotlight: Helping At-Risk Patients Stay at Home (PatientPing)
- A Five-Star Payment Experience is Something to Strive For, Especially in Health Care (Patientco)
- Case Manager Leans on “Patchwork Quilt” of Services to Address Social Determinant Issues (PreparedHealth)
- AI and Cybersecurity: Are We Fueling Hackers’ Fire? (SailPoint)
- Why It Matters: Prescribers Can Now Access Accurate Medication History Data for Virtually Every American (Surescripts)
- Founder Letter: How to Win Patients for Life (WebPT)
Get Involved
- Join my Rolodex to provide occasional news reaction or ideas
- Contribute regularly as a provider CIO, IT director, or informatics nurse (anonymous or not)
- Be interviewed (providers)
- Deliver an educational webinar (providers)
- Sponsor
- Report a news item or rumor (anonymous or not)
- Sign up for email updates
- Connect on LinkedIn
- Contact Mr. H





NYT op-ed piece. Generally EXTREMELY sympathetic to clinicians and the burdens placed on them, but, out of touch much OP?
After reading the article I feel for clinicians that are experiencing burn out. I can only imagine what it is like to get the “calling” for the medical field only to be disgruntled about the way they are forced to practice medicine.
One issue I see here is the move away from private practice to one of employed physicians by large healthcare corporations. This model removes all of the day-to-day decisions that physicians can make to determine their own path or business model. They relinquish control of their practice for more money and less headache in dealing with the issues of running your own practice. I would like to see a study looking at the difference in attitude between those physicians employed by healthcare corps to those still running a private practice. Do they experience burn-out at a rate less than their employed counterparts? Are they happier with the freedom of running a private practice?
As for the continued drum beat of a single payer health system……….we would only be trading one corporate master for another “master”, one run by politicians with ever changing motives. At least corporate healthcare companies have a single motive in mind…..profit. Politicians care about votes and they will be taking money from these large corporate healthcare companies to insure they get those votes. The only way out is for physicians to take matters into their own hands and move away from the employed physician model.
Politicians already take large amounts of money from corporate healthcare companies. It is really strange to hear someone say that they prefer their health care provider to be accountable to profit seeking shareholders rather than being accountable to politicians who care about votes/voters. .
I think the comment may have (too?) quickly stepped through single payer on the way to the ultimate worthy conclusion.
Physicians have chosen employment because the capital and contracting issues of maintaining a practice in recent times. In so doing, they may have lost sight of their leverage: these corporate overlords cannot hold the medical license to practice.
The scale of practice required for supporting IT may not be under 5 FTE MDs, maybe not even 10, but it is not hundreds of doctors attached to a hospital. Contracting is another matter, but it shouldn’t require hospital affiliation either. In the rush to employment, a space has opened up for right-sized physician groups to do it better. (though payer-owned community practices may be sliding into it).
Single payer could simplify the business demands of many payment regimes, BUT it would not be going back to the “good old days.” Value-based payment schemas and quality reporting, pre-authorization and formularies would continue, surely. I am not even sure there would truly be one, unitary system governing those mechanisms.
Physician groups practicing independently from hospital-centered health systems would still have headaches, but they could be in charge of their own destiny.