Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…
Readers Write: The Treatment for BCD (Big Company Disease): How to Streamline EHR Decision-Making
The Treatment for BCD (Big Company Disease): How to Streamline EHR Decision-Making
By David Butler, MD

David Butler, MD is associate CMIO of the Epic/GO project of NYC Health + Hospitals of New York, NY.
I’ll never forget it. I was presenting to a large group of physicians about how we need to implement, adopt, and standardize the EHR to meet quality metrics and decrease total cost of ownership. Before I could finish stating the “S-word” (standardization), a more senior physician looked over his glasses and declared, “Son, I’ve been in healthcare for over 30 years and I can tell you for a fact that this is simply not going to work.”
I had to agree with a portion of his statement. I also had a degree of skepticism about whether this would work or not. However, the former part of his statement caused me to pause and ask, “With all due respect, Doctor, have you been in THIS healthcare for 30 years?”
While I’m not sure he appreciated my Gen X retort, what I said was true. No one has been in today’s healthcare environment for 30 years. A senior executive mentor from McKinsey once told me, “If someone tells you that they understand healthcare today, they’re either lying or just have not been paying close enough attention.”
How We Got into This Mess
The US has wrapped technological advancements in healthcare around an antiquated legal and compliance system that was designed for the long-gone days of paper-based record keeping. We have essentially paved the cow path. Years after these technical infrastructures in healthcare have been hardwired and codified, we are now asking the question, “How can we unwind this and do it the right way?”
Unfortunately, much of the capital dollars and funding that attained the EHR are no longer available to optimize the EHR (understatement of the year). Very few practicing physicians have the time or legal prowess to navigate a fleet of internal compliance, risk, legal, and information technology “experts” who have all agreed that “x should not be turned on.”
All is not lost, though. We have figured out ways to map and execute the transition to digital healthcare, but we must do it together. EHR optimization starts with governance. In this article, I will share three guiding questions that physicians and physician executives can use to assure that their voices are heard and prioritized when EHR decisions are being made. Just as we do not triage a patient with a cough prior to one with chest pain, we must use this same approach when we collectively request changes to the EHR software.
BCD: Big Company Disease
Rule of thumb: The bigger the healthcare system, the slower it is to change.
At one large multi-hospital facility that shared a single instance of the EHR, a physician stated that it took three months for their EHR team to fix a misspelling on the after-visit clinical summary that we give to the patient. The road to EHR optimization is not a straight one, and you need a team to decide what you’re going to do every time you encounter a fork or a bend. Who makes decisions about EHRs in health systems? If you’re like most, this is a staggeringly complex and confusing process (and calling it a process at all might be generous). You’re likely suffering from BCD, or big company disease.
BCD is an epidemic. Hospitals and health systems must implement technology that helps them meet the goals of 2017 healthcare, Value-based purchasing, consumerism, MIPS/MACRA, ACOs … the list goes on. These goals require change in clinical and technology operations and this change must occur rapidly — or at least much more rapidly than the current pace at most organizations — to meet them.
BCD is fraught with complex requirements, departmental silos, poor stakeholder representation, and highly-educated and well-intentioned leaders whose decision-making authority has been stretched much further than their own comfort zones (and pay grades). As we’re working on the cure for BCD, these treatment options will alleviate many of its symptoms.
Three Questions to Establish Governance for EHR Optimization
1. Who makes the decisions about the EHR?
The first step of governance for EHR optimization is determining who the decision-makers are. If you employ a democratic philosophy of governance, then you must first decide what is your constitution (some call it a mission statement). This constitution drives every decision that you make, including who needs to be at the table from the key stakeholder groups: operations, clinical, and IT. These three functional branches of government compose the three-legged stool governance model. If you’re a large system, you’re also going to need three levels of stakeholders: site/local leadership, regional leadership, and corporate/system leadership. No matter how you answer this question, your governance model must be clearly defined and communicated throughout the organization.
2. What are your priorities?
Everything can’t be a priority. All optimization efforts, requests, and enhancements are certainly NOT created equal. After asking the two most critical questions—“can we?” and “should we?”—I often use and recommend adapting an impact effort matrix to determine the clinical impact and resource requirements for EHR project request prioritization:
- Quadrant 1: The “Just do it” quadrant. High clinical impact, minimal resources.
- Quadrant 2: The “Get the geeks, the execs, and the checkbook” quadrant. High clinical impact, high resources.
- Quadrant 3: The “That’s cool” quadrant. Low clinical impact, low resources.
- Quadrant 4: The “Diva” quadrant. Low clinical impact, high resources.
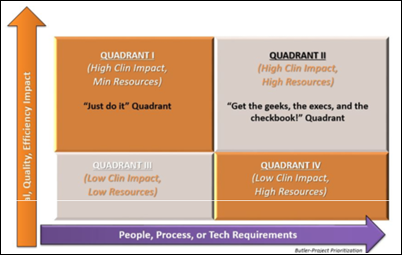
Before you do anything, make sure you know what quadrant you’re working in! Many organizations have found success building upon this simple framework with Lean or other process improvement methodologies.
3. How are we going to make this happen?
You have your governance model established with balanced representation or your three-legged stool. Now, how do you get these people together to actually use the framework to make critical EHR optimization decisions? This is one that plagues virtually every organization I work with. “I didn’t know WE decided that” or “when are the meetings even held?” are common stakeholder grievances.
When the governance group can’t all come together, you end up making decisions based on time constraints instead of thoughtful ones with the right people around the table. Keys to recovering from BCD include:
- Clear roles and responsibilities. What is each committee responsible for accomplishing at the end of the day? (Oh, this is called a charter.) These obligations should be fully defined and every committee member should know this for their committee, as well as the others in their organization.
- Effective meeting management and tools. Before each governance meeting, tackle these items. Determine which decisions, if any, can be made without meeting. Pre-plan the meeting – set the agenda for this meeting by highlighting what was discussed at the last meeting and the action items/decisions to be made at the meeting. Meeting polls — If your governance committee is large, this is a great way to determine consensus quickly. Virtual meeting tools exist that make interaction and measurement much easier.
- Transparent decision-making and prioritization. You have to share information and you have to share it often. Send out a post-meeting debrief to the committee and the other committees within your organization. Make sure everyone knows how the decision was made and how they can escalate an issue. IT should not be the first place to go to get an EHR solution fixed—physician leadership should determine this. Remember: EHR optimization is a clinical project, not a technical project.
Large-scale EHR optimization starts with an effective, mission-aligned, and accountable governance process. Nagging symptoms of BCD may linger longer than you care for, but with the treatment plan I’ve prescribed above, you’ll be in a much better state to move your organization forward.


Right on. Prioritize – can’t do it all. Ruth