Thanks, appreciate these insights. I've been contemplating VA's Oracle / Cerner implementation and wondered if implementing the same systems across…
News 4/8/16
Top News
The Department of Defense christens its Cerner-centered EHR project as MHS Genesis. The functional project champion explains, “We want people to know MHS Genesis is a safe, secure, accessible record for patients and healthcare professionals that is easily transferred to external providers, including major medical systems and Department of Veterans Affairs hospitals and clinics. When our beneficiaries see this logo or hear the name, they’ll know their records will be seamlessly and efficiently shared with their chosen care provider.”
I might quibble that the DoD’s new logo incorrectly contains all capital letters in spelling GENESIS and looks like something a Photoshop newbie might design, but at least it uses the correct Greek mythology symbol of the wingless Staff of Asclepius – which denotes healing and medicine –rather than the oft-mistaken winged Staff of Caduceus, which is symbol of commerce. Still, I can understand how the latter is more appropriate than the former in our convoluted healthcare system, where the lines at the financial trough are often serpentine.
Reader Comments
From ZenMaster: “Re: Sandlot Solutions. Website down. Phone not working. Clients frantic. A cautionary tale for all the start up Population Health Analytics companies out there. HIE / Healthcare Data Aggregation / Population Analytics is hard. Proceed with caution.”

From A Vendor That Also Finds Email Tracking Slimy: “Re: vendors being informed when you open their spam email and then contacting you directly. Most of these programs function by embedding a one-pixel image into emails and tracking when that image is loaded. Disable the automatic download of images in your mailbox settings or contact your organization’s IT team about blocking or filtering items that are created using similar methods like Tout, Sidekick, Yesware, Streak, etc.” Promos for the Yesware tracker shows why aggressive companies keep using it for “prescriptive analytics” to pester prospects – unfortunately, it works, just like other sales techniques that range from cold calling to outright lying.
HIStalk Announcements and Requests
We funded the DonorsChoose grant request of Ms. S in Texas, who asked for five animation studio kits for her elementary school class to produce STEM-related movies.
Also checking in is Mrs. S from Connecticut, whose middle schoolers are using the Chromebooks we provided to publish and discuss their writing, with some of the most active participants being those students who don’t otherwise engage.
Speaking of Chromebooks, I decided to round out my little technology arsenal of everything I use to research and write HIStalk (a $300 Toshiba laptop and a $200 iPad Mini) with a Chromebook. The Asus C201 has an 11.6-inch monitor (perfect for traveling), 4 GB of memory, a 16 GB solid state drive, a very nice Chiclet keyboard (I’m not a fan of on-screen and tiny Bluetooth keyboards), and a battery life of around 10-12 hours. It weighs about 2 pounds and is 0.7 inches thick. It powers on and off almost instantly and took almost no time to set up, automatically updating itself as needed in the background with no third-party antivirus needed. The learning curve is pretty much zero – the only workaround I had to look up was how to regain Delete-key function since that key is omitted from most Chromebooks for space reasons. Best of all, it was only $200 complete with a nice padded sleeve and a wireless mouse with nano receiver. Chromebooks use the Chrome OS operating system instead of Windows or Linux, so they won’t run most desktop apps, but the Chrome browser is very fast (as are Google Docs and Gmail), Dropbox works fine, and thankfully my most valuable program LastPass works great on it for automatically logging me in password-protected sites I’ve saved, like Amazon. I even installed the Chrome OS version of Teamviewer in case I need to remote back into the laptop to do something. It’s not for everyone – for example, folks who rely on desktop versions of Office – but you might be surprised at how much of your work is online once you think about it and this is an inexpensive, lightweight, headache-free alternative to Windows or Apple laptops.
This week on HIStalk Practice: KAI Innovations acquires Trimara Corp. Family physician Kim Howerton, MD stumps for direct primary care in Tennessee. DuPage Medical Group expands relationship with PinpointCare. Cable and home security business Connect Your Home gets into the telemedicine business. Culbert Healthcare Solutions VP Johanna Epstein offers advice on improving patient access (and ROI to boot). Kaiser Permanente Northwest puts medical record access at patient fingertips. Tribeca Pediatrics founder details the drastic steps he took to revitalize his failing practice. Biotricity CEO Waqaas Al-Siddiq offers his take on what’s holding physicians back from making the wearables leap.
Webinars
April 8 (Friday) 1:00 ET. “Ransomware in Healthcare: Tactics, Techniques, and Response.” Sponsored by HIStalk. Presenter: John Gomez, CEO, Sensato. Ransomware continues to be an effective attack against healthcare infrastructure, with the clear ability to disrupt operations and impact patient care. This webinar will provide an inside look at how attackers use ransomware; why it so effective; and recommendations for mitigation.
Contact Lorre for webinar services. Past webinars are on our HIStalk webinars YouTube channel.
Acquisitions, Funding, Business, and Stock
Andover, MA-based National Decision Support Company opens a research and development headquarters in Madison, WI.
Population health management systems vendor Lightbeam Health Solutions acquires Browsersoft, which offers an HIE solution built with open source tools.
Digital check-in vendor CrossChx raises its second $15 million round in two years, increasing its total to $35 million.
Sales

Tampa General Hospital (FL) will implement the Voalte Platform for caregiver communication.
Universal Health Services will replace the former Siemens Invision revenue cycle solution with Cerner’s revenue cycle solution, integrating with UHS’s existing Millennium products. For-profit hospital management company UHS operates 25 hospitals.
The Department of Defense awards a five-year, $139 million contract to McKesson’s RelayHealth for patient engagement and messaging solutions. I assume that’s an extension or expansion since the military was already using RelayHealth.
Ernest Health (NM) will expand its use of NTT Data’s Optimum Clinicals suite in four facilities. The organization uses Optimum RCM in its 25 locations.

Queensland, Australia’s Metro North chooses the referrals management system of Orion Health.
People

Influence Health names Michael Nolte (MedAssets) as CEO. He replaces Peter Kuhn, who remains as president, chief customer officer, and board member.
Announcements and Implementations

Franciscan Alliance (IN) uses InterSystems HealthShare to create a vital signs viewer for legacy data that can be accessed from inside Epic by its 140-physician group.

India-based doctor finding and appointment scheduling app vendor Practo begins answering medical questions from India, the Philippines, and Singapore at no charge via Twitter using the @AskPracto account.
Government and Politics
National Coordinator Karen DeSalvo, MD, MPH says of information blocking in a Wall Street Journal interview, “We don’t have all the authority we need to really be able to dig into the blocking effort. We have put forward a proposal to Congress asking for more opportunities to address the issue.” She says that it’s a big step that the major inpatient EHR vendors have pledged to not participate in information blocking vs. a year ago when “people said blocking is a unicorn and not happening.” She adds consumers are interested in third-party apps that can extract data from elsewhere to create their own longitudinal health record and says that person-centric medical records will shift “very deliberately away from the electronic health record as being the source or center of the health IT universe.”
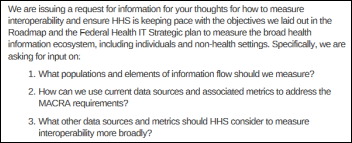
HHS asks for ideas about how to measure interoperability within MACRA objectives, with responses due June 3. The most interesting part of the information published in the Federal Register is that ONC is considering analyzing the audit logs of EHR users to determine how often they exchange information.
AMIA says proposed HHS changes that would give drug and alcohol abuse patients more control over their medical records aren’t adequate and fail to address electronic information exchange. AMIA wants HHS to revisit the idea of giving patients granular sharing control over their entire medical record, saying that managing substance abuse data differently is “a dated concept and flawed approach.” Doug Fridsma, MD, PhD, AMIA president and CEO, said in a statement, “Clearly, the trend in healthcare is to make patients first-order participants in their care. This means giving them complete access to their own medical records, and it should mean giving them complete control over who sees their medical information.”
Privacy and Security
MedStar Health (MD) disputes earlier Associate Press reports indicating that an unpatched JBoss server allowed hackers to take its systems down with ransomware. MedStar says Symantec, which it hired to investigate the attack, has ruled out unapplied 2007 and 2010 JBoss patches as the problem. The AP stands by its earlier report and adds that experts say that the Samsam ransomware that infected MedStar can be prevented by keeping updates current.
Google’s Verily Life Sciences biotechnology company comes under fire for awarding a research contract to a company its own CEO owns and for failing to tell its Baseline health study volunteers that it is planning to sell their data to drug companies for a profit.
Metropolitan Jewish Health System (NY) announces that an employee of one of its participating agencies responded to a phishing email in January 2016, with the unidentified hacker gaining access to the email account that contained PHI.
Other
Leapfrog Group finds that CPOE systems still miss a significant number of drug ordering errors, failing to warn the prescriber of potentially harmful orders 39 percent of the time and also missing 13 percent of potentially fatal orders. Leapfrog collects voluntary CPOE test results from hospitals that use its testing tool.
The AMA publicly supports AllTrials, a global campaign that calls for every past and present clinical trial to be registered with their methods and summary results reported. The campaign says it’s not fair to study participants to hide study results that are inconclusive or unfavorable to the sponsoring organization, such as a drug company buying a study that finds one of its products ineffective. Commendably, the AMA’s involvement came from a proposal from its Medical Student Section.

The COO of BCBS of North Carolina, promoted from CIO four years ago, resigns abruptly after the botched rollout of a billing and enrollment system last November during Healthcare.gov’s open enrollment period. The company is scrambling to rewrite the system in time the next open enrollment that starts November 1. It found an unspecified “fatal problem” in its software before last year’s open enrollment began, but continued anyway thinking it could fix problems as they arose, causing 147,000 customer calls on November 1 alone and 500,000 in the first week. The company imposed emergency measures in January 2016 after projecting that it will lose $400 million in North Carolina Healthcare.gov business, turning off the ability for consumers to apply online since they had no way to determine whether the applicant was actually eligible to purchase insurance.
The always-hustling Newt Gingrich pens an editorial criticizing his home state of Georgia for proposing to outlaw people doing their own eyeglass exams at home via a company’s app. USA Today got the assurance of Newt’s people that he had no financial interest in any related firms before running his op-ed piece, only to find out afterward that he’s running a $100 million tech fund with a private equity firm.
I missed a great April Fool’s prank by MedData, who announced the April 1 hiring of Hayden Siddhartha "Sidd" Finch as chief experience officer, slyly referencing a 1985 George Plimpton April’s Fool fake story in Sports Illustrated involving a Tibetan pitcher with a 168 mph fastball. The brilliant Plimpton even led off the 1985 story with a clever clue in spelling out “Happy April Fool’s Day” with the first letters of each word in the opening sentence, but still duped a significant number of people who should have known better (including a Senator, reporters, and Mets fans looking for hope).
An article questions whether it’s OK for sexting-comfortable teens to send genitalia photos to their doctors for diagnosis, wondering whether those images should be sent securely or whether the doctor receiving them might even be charged with possessing child pornography.
A woman who recorded her hernia operation with a hidden recorder captures OR staff making fun of her belly button and calling her “Precious” from the movie about an overweight teen. Harris Health System (TX) declined to comment citing HIPAA, but told the woman they had reminded OR staff to watch their comments and that was enough. She says she was racially profiled and is considering suing.
A primary care physician at Massachusetts General Hospital (MA) says the lack of patient narrative in EHRs dehumanizes patients and hampers the diagnostic abilities of physicians, noting that the story of Cinderella, if entered into the hospital’s newly implemented Epic system, would be a problem list consisting of “Poverty, Soot Inhalation, Overwork, and Lost Slipper.” She describes Epic (and thus EHRs in general) as:
Epic features lists of diagnoses and template-generated descriptions of symptoms and physical examination findings. But it provides little sense of how one event led to the next, how one symptom relates to another, the emotional context in which the symptoms or events occurred, or the thought process of the physician trying to pull together individual strands of data into a coherent narrative. Epic is not well-suited to communicating a patient’s complex experience or a physician’s interpretation of that experience as it evolves over time, which is to say: Epic is not built to tell a story.
A Boston Globe article ponders why the medical schools of Harvard and nine of its prestigious peers like Yale, Johns Hopkins, and Columbia don’t have a department of family medicine. Harvard blames lack of costly participation by its affiliate hospitals to support a residency. However, a Harvard medical student says doctors specializing in internal medicine and pediatrics often bolt for more lucrative subspecialties while most family medicine practitioners remain in primary care, adding that Harvard Med thinks, “You’re less competitive or you’re less rigorous if you’re interested in primary care.” Ironically, Harvard launched one of the first family practice residencies in 1965, but the federal government ended its funding 10 years later due to poor quality. The chair of the recently created family medicine program at Icahn School of Medicine says bluntly, “It’s bizarre to me that you have these institutions that don’t really feel that there’s a requirement to introduce their students to the second-largest specialty in the United States.”
The department of physical and occupational therapy at Massachusetts General Hospital (MA) create a video just before its April 2 go-live with Epic.
Sponsor Updates
- CloudWave joins the Microsoft Cloud Solution Provider program.
- Experian Health will exhibit at the SE Managed Care Conference April 7-8 in Charleston, SC.
- PeriGen publishes its annual review of labor and delivery malpractice awards.
- Red Hat announces the winners of its 2015 North American Partner Award Winners.
- The SSI Group will exhibit at the Texas Ambulatory Surgery Center Society 2016 Annual Conference April 7-8 in San Antonio.
- Streamline Health will exhibit at the 2016 HASC Annual Meeting April 13-15 in Dana Point, CA.
- Surescripts announces its 2015 White Coat of Quality Award winners for excellence in e-prescribing quality.
- Iatric Systems will exhibit at the Hospital & Healthcare IT Reverse Expo April 13-15 in Atlanta.
- RTLS technology from Versus earns Cisco Compatible Extensions certification.
- A record number of attendees gather at InstaMed’s annual user conference.
- InterSystems will host its annual Global Summit April 10-12 in Phoenix.
- Intelligent Medical Objects will exhibit at HealthCon2016 April 10-13 in Lake Buena Vista, FL.
- Netsmart will exhibit at the Texas Public Health Association Conference April 11 in Galveston.
- Obix Perinatal Data System will exhibit at the SSMHealth Annual Perinatal Nursing Conference April 14 in Fenton, MO.
Blog Posts
- Medicity Highlighted in KLAS HIE 2016 Specialty Report (Medicity)
- Healthcare Security, Part 1: More than a Firewall (CloudWave)
- 6 Reasons to Choose Secure Text Messaging for BYOD (Spok)
- Platform Openness and the Art of Integration (PatientSafe Solutions)
- Change the Paradigm (PatientKeeper)
- Reimagine traditional business models to fix healthcare (Lexmark)
- How will I-STOP Affect Specialty Prescribing? (Point-of-Care Partners)
- 5 Tips for Designing Efficient Epic Workqueues (Sagacious Consultants)
- Moneyball Meets Cost Modeling (Impact Advisors)
- How are Companies Managing Risks in the New Data-Centric World? (Liaison Technologies)
- Banishing CDs: A Two-Pronged Approach to Streamlining Outside Image Management (LifeImage)
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Send news or rumors.
Contact us.










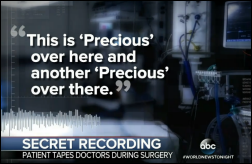
RE: A woman who recorded her hernia operation with a hidden recorder captures OR staff making fun of her belly button and calling her “Precious”…
OK, this is just weird, and the word “Entrapment” comes to mind. I mean why would anyone even do that? Did she have reason to believe she would be made fun of? Or just victim mentality? I don’t get this one.
Regarding the Cerner announcement about UHS. Is Invision being replaced by Soarian or Cerner’s revenue cycle product? (FKA ProFit)
.
Email tracking is actually really important when doing email marketing. It’s impossible to figure out if email campaigns are effective or useful to people without it. Knowing who just deletes your email also lets you know who to stop wasting time/effort emailing.
With regard to your current survey about who to trust with your personal health information – don’t ALL of those vendors/sites have parts and pieces of your information already? A related but somewhat separate question is what rights do you have to address and/or correct false information contained in your record. I have a close relative who had a bad encounter (okay it is a somewhat cantankerous elderly aunt…) with a provider during a hospital stay and then noticed that the primary diagnosis given for that particular stay was alcoholism secondary to Borderline Personality Disorder. Nice. Simple but formal requests questioning the diagnosis (this was a surgical stay BTW), have gone un-addressed. Reminds me a little of the problems encountered with credit reporting databases when they get something wrong.
Re: lack of patient narrative in EHRs
If you want narrative in the EHR, type it.
Re: Patient narratives in EMR.
I am served by a health system that uses Epic, and I actually seek specialists in that same network when I need other care (ex: allergist) BECAUSE there is a common health record for me that is consistent across all doctors and they all have the same info when they treat me, and the same meds lists and can see any lab results on file. Each time I have an appointment, the nurse first interviews me to validate the info in the system as to meds, etc., so the record is kept as accurate as possible.
I don’t do this because of Epic (I’m not a big fan of theirs actually), it is just that Epic (as some other HIS vendors, I would imagine) makes the EMR info available to all “owned” physician practices.
In this system I am able to go in and mark pharmacy that I no longer take (thus taking it off the list, where it remains on an inactive list with a reason it is inactive), and can add more medical conditions should they arise – with the caveat that until a physician validates the condition, it just remains as patient reported. But in some ways, I am able to participate in keeping my medical record accurate.
This gets my vote as the PHR model has failed (actually never really got going), and letting me update and/or contribute to a real EMR record kept by a health system provides the best of both worlds. Obviously, patients who don’t have such access due to where they live don’t get this benefit.
IF ONLY there were true interoperability (remember the failed promises of RHIO/CHIN and now HIE?) where my record in ANY EMR-type system would be compiled and available to the treating doc (and also let me do similar edits/comments as I can in Epic) – – but then again, there goes the dream I’ve tried to solve for the past 15 years . . .
#narrative absence
Simply another reason for the failure of EHRs to improve outcomes and reduce costs.
Do other hospitals allow physicians (or other clinical users) make changes to their own records? Does this get audited? I am surprised that your institution allows this. At my health system, we won’t allow anyone to edit their own record. In fact, it is pretty easy to set up with Epic. We have set up “break the glass” feature when any clinician is accesses clinical record of another hospital employee when outside of normal appointment/admission.
Responding to Epicalista Editing from April 9 – I may not have been fully clear – I am not an employee of the health system, just a patient. As a patient, they provided me with a password protected account in MyChart (that took initial security to get my account and password to me) that I log into to get lab results, use the internal system to email my clinicians (and yes, they do respond), order refills, etc. I can’t modify my record – such as deleting something or changing wording. But I can check a current med as ‘inactive’ and give a reason. The med stays on the list but moves to the “inactive” portion of the list
When I go for an office visit, that doctor/staff have the rights to see my record since they are treating me. The first 5 minutes of the visit is the nurse taking BP, etc, asking how I am and “anything to report” type questions, which they document in the system while talking to me. Each time they also go down my the meds list in the system and ask “are you still taking ‘X’?” to validate it is a current med.
I’m sure that the other HIPAA precautions are in place – if I’m not your patient, you can’t access my record. So note this is not a “break the glass” issue since I’m not an employee of the health system. And I’m not changing anything in the system, just making notations.