Amazing that the takeaway is that its easier to buy a gun than to get credentialed as a physician is…
Curbside Consult with Dr. Jayne 11/23/15
I’m still tunneling out after having been at the AMIA conference and then on site with a client who scheduled an emergency board meeting to discuss pulling the plug on their EHR. They’re a mid-sized multispecialty group that is physician-owned, so the entire board is made of physicians. The board meetings can be extremely contentious.
Apparently this one was in response to some agitation among doctors who recently joined the group and are not happy with having to give up their previous EHR, so they’ve united with some other unhappy doctors to push the idea that the entire group should change platforms.
My role was largely to support the IT department and the rational members of the physician leadership who don’t want to throw the baby out with the bath water. They’ve had some bumpy upgrades in the last year, but the group is also experiencing growing pains courtesy of some physician acquisitions as well as general growth in their geographic market. They’re also experiencing some Meaningful Use-related challenges with workflow (which is how they came to be my client).
With all of that swirling around, it’s hard to lay blame on the vendor. Unfortunately, the vendor hasn’t had good communication through all of this and hasn’t been as participatory in troubleshooting some of the issues, so they already have a black eye.
Although the board meeting ran nearly three hours, we were able to achieve a reasonable resolution. I’m going back in a few weeks to do not only a workflow assessment, but also some stakeholder interviews to try to get to the root of what is going on as well as to try to uncover any other factors that haven’t fully bubbled up yet. Once we have the full picture from all the physicians (including those who are happy and therefore weren’t at the meeting screaming), we’ll be able to put together an action plan and make some interventions to improve things.
I did a follow-up call with the vendor on Friday. I don’t think they know what to make of a consultant who is not only a physician, but also knows her way around infrastructure. I left them with a to-do list of troubleshooting that they hadn’t even looked at yet, so I’m sure we have additional amusing (for me) and/or uncomfortable (for them) conversations in our collective future.
Also on Friday I listened to the Athenahealth Leadership Institute webinar, “An Interview with Dr. John Halamka and Jonathan Bush.” Although they had some audio troubles at the beginning, it was a good interview. I enjoyed John Halamka’s comments on information blocking and the perception that vendors, hospitals, and health systems are charging too much for interfaces. Halamka cited one survey that said physicians would be willing to pay $5 per month for information exchange, which is a far cry from the hundreds to thousands it may cost to implement an interface. Having seen it from both sides myself, it’s a great topic that needs further exploration.
They also discussed Halamka’s genome since it’s been sequenced and available, and how knowing his genetic status makes a difference in the screening services he should receive. I’m not sure if it’s recorded or available, but if it is, it might be worth a look.
I spent most of Saturday doing a community service project, which was a great way to reset after being gone for the week. I’m a mentor for a local youth organization and it’s particularly nice to see teenagers out serving the community, even if it means being in the snow and slush when they could be home watching TV and texting each other. This is my tenth year doing this particular project and some of the kids I started with are now old enough to drive, which is a bit of a scary thought. It does give me hope for the future, though.
As most of you know, I left my CMIO position some time ago. My hospital, however, still has not removed me from the email distribution lists, a fact which continues to provide ongoing entertainment. This week’s email gem (sent on November 19) outlined all the changes that took place in the system on November 17. I know I wasn’t perfect, but at least I got the change notices out before they happened. I know they’re in the middle of a system replacement and whoever is responsible for the communications now is probably distracted, but I still feel for the physicians and end users.
I also feel for all the employees who are going through open enrollment right now. Several of my friends have been cursing the rising premiums and shrinking benefits even with self-insured employers. I’m eligible for benefits through my clinical position, which thank goodness has no change in medical premiums and only 1 percent change in dental with the same level of benefits for both. I don’t know what kind of good karma we’re riding, but I know it’s making our employees very happy.
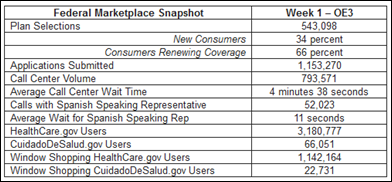
Looking at the open enrollment statistics for the federal marketplace, the happiest callers might be the Spanish speakers, who averaged an 11-second wait for a representative vs. the average four and a half minute call center wait time. That’s still a lot better than I get with either my Internet provider or my cellular carrier. Looking at the data, there are a lot of window shoppers out there as well.
In other CMS news, I’ve seen several headlines about the Affordable Care Act leading to $2.4 billion in consumer rebates on health insurance premiums. This sounds like a lot of money until you realize how many patients it is divided among. My clinical employer was a recipient of one of those rebate checks, which ended up dividing out to $0.48 per employee – not even enough to cover a stamp. I’m sure our administrative staff spent a lot more than $0.48 per person dealing with questions and helping people understand how tiny it was. Personally I was in favor of taking the refund and donating it to a local food pantry, but they did go ahead and post the amount to each person’s paycheck. The CMS press release claimed $470 million in rebates for 2014 alone, averaging to $129 per family. Based on the math, some people might have gotten some nice rebate checks.
How’s your open enrollment process going? Email me.

Email Dr. Jayne.


How’s it going? I knew it was going to be bad when we received a notice that Highmark was discontinuing the plan covering my wife and I at year end. This was an individual silver plan purchased on the marke,t but not in a Marketplace as no subsidy for our income level. I expected at least a thirty percent rate increase in a new comparable plan, as I had seenearlier this year that PA’s Department of Insurance had refused the requested rate hike. Just found out that the replacement plan from Highmark would cost us almost $1600 per month, up from $969 per month under the old plan, both silver level. The cheapest available, bronze level with outrageous deductibles and coinsurances would be over $1200. So I’d say it is going badly.
I continue to ask why we need this plethora of “plans” in the first place, let alone “marketing” departments. But then I am a believer that those in power will continue as long as possible to keep their noses in the trough with so-called market driven solutions.
Ultimately it reminds me of the similar situation where consumers in PA and other states have the choice of electric or gas suppliers. How does the average consumer know the futures price of electricity next summer. or gas this winter to choose wisely? Likewise, how do we know when we will suffer “the big one” and what it will cost at the time, let alone how long will that time be?
We are thankful for your blog, Dr. Jayne! Have a wonderful Thanksgiving!
Thanks, Tom!