"The US Immigration and Customs Enforcement (ICE) posts an anticipated future contracting opportunity for a correctional EHR for ICE detainees,…
Monday Morning Update 10/20/14
Top News
Texas Health Resources takes out full-page ads in local newspapers to bolster its community image, with CEO Barclay Berdan admitting that “we made mistakes” and adding that Thomas Duncan’s travel history was documented in the EHR but “not communicated effectively among the care team.”
Meanwhile, the cruise ship passenger that triggered an Ebola scare at sea (for questionable reasons) that resulted in the ship’s return to port has been identified as the lab director of Texas Health Presbyterian Hospital Dallas where Thomas Duncan died. The lab director voluntarily quarantined herself in her ship’s cabin and has since been found to be free of the virus.

In the aftermath of its mistakes (of both clinical and public relations varieties), Texas Health Presbyterian Hospital Dallas is reported to be a “ghost town” with two-thirds of its 900 beds empty and its average 52-minute ED wait time down to zero. THR spokesperson Dan Varga, MD states that doctors whose offices are near the hospital are having up to 60 percent of their appointments cancelled as patients refuse to get close to hospital property, treating it as though it were Chernobyl instead of the building that previously housed a contagiously sick patient as it does 365 days per year. The economic impact will probably be significant.
From British Bulldog: “Re: Ascribe. The UK-based company’s CEO and founder, Stephen Critchlow, has resigned, almost a year since Ascribe was acquired by EMIS. Rumour has it that this could spell the end for Ascribe’s Health Application Platform, its flagship software platform.” The company announced Critchlow’s departure to devote “more of his time to his other business interests” on September 29, 2014, while the rest of the statement is unverified.

From Government Mule: “Re: ONC chief medical officer. Jon White from AHRQ took the job according to his LinkedIn profile.” Actually he lists his position as interim CMO (at least in the current version of his profile), which was announced early this month as a part-time commitment while the search is underway.
From GoVols: “Re: [company name omitted]. The CTO resigns, then gets talked out of it by board member. Sales, marketing, and BD team, once 15 strong, is now down to just a few and more layoffs are rumored. No significant sales this year and the fourth sales VP was recently fired. Everyone still here wonders what the BOD is thinking.” I’ve removed company and executive names since no company is going to confirm statements like these, but I’ll keep an eye on what happens there.
From Insidehr: “Re: athenahealth’s Ebola screening tool. Good to hear the athena clients are ready to treat those Ebola patients when they show up for the primary care visit. Sometimes that group would benefit from the concept of less is more.” It’s interesting that everybody is rushing to cobble together electronic tools that perform the most basic function – display a warning if a feverish patient says they’ve been to Africa lately. I think we can assume that even the least-competent nurse in America would go on alert in that case even without an EHR prompt, so its main value isn’t evaluating the patient’s response, it’s reminding someone to ask them the question in the first place, which is also probably not really necessary.
Additionally, the value of crude tools like online questionnaires will be eliminated if the virus starts spreading from people who haven’t traveled but instead were exposed to someone else who has, perhaps unknowingly. It’s like those early HIV/AIDS questions that asked about same-sex contact, blood transfusions, or exposure to prostitutes – they helped make a few diagnoses in the absence of anything more accurate, but the real accomplishment was developing specific lab tests since patient reports aren’t always reliable, symptoms are vague, and other transmission methods may be involved. A lab person can jump in, but I think the ELISA test works for both HIV and Ebola, the main difference being that a two-day wait time for positive diagnosis is OK for HIV but potentially disastrous for Ebola. When it comes to stopping pandemics, it’s at least equally important to develop diagnostic as well as therapeutic technologies.
HIStalk Announcements and Requests
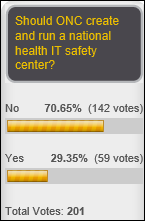
More than two-thirds of poll respondents don’t like idea of an ONC-run health IT safety center. Reader lgro said in a comment that ONC struggles with the logistics of its current areas of responsibility and worries about another HIPAA-like program that doesn’t add value, while Doug points out that the health IT safety center was proposed as a public-private partnership rather than an ONC-controlled body and may provide value in preventing FDA from stepping in due to lack of progress. New poll to your right or here: should the names and medical details of Ebola patients be divulged publicly?
Last Week’s Most Interesting News
- The American Medical Association sends CMS a blueprint for a redesigned Meaningful use program, adding its criticism of document-based interoperability protocols such as C-CDA.
- Several groups add to the drumbeat urging CMS to slow down the Meaningful Use program and to refocus certification on interoperability, privacy and security, and quality reporting.
- Texas Health Resources executive Daniel Varga, MD says the organization modified its Epic setup and workflow after Ebola patient Thomas Duncan was discharged from one of its EDs, adding little clarity to the original report and subsequent denial that the nurse’s documentation was missed because of an EHR setup problem.
- A paper from the National Bureau of Economic Research says that HITECH was largely ineffective for spurring hospital EHR adoption since most hospitals were already using them.
- HITPC agrees that current document-based interoperability approaches should be replaced by programming APIs provided by vendors of certified EHRs. That would be a dramatic shift, especially if ONC requires such access for EHR certification.
- California HealthCare Foundation releases a report covering health accelerators, find that they are excessive in number, unproven in benefit, and potentially harmful in hyping startups that have a minimal chance of market success.
- Alameda Health System (CA) says a disastrous $77 million Siemens Soarian-NextGen implementation has exhausted its cash and available credit.
Webinars
October 21 (Tuesday) 1:00 p.m. ET. Electronic Prescribing Of Controlled Substance Is Here, What Should You Do? Sponsored by Imprivata. Presenters: William T. “Bill” Winsley, MS, RPh, former executive director, Ohio State Board of Pharmacy; Sean Kelly, MD, physician, Beth Israel Deaconess Medical Center; David Ting, founder and CTO, Imprivata. Providers are challenged to use EPCS to raise e-prescribing rates for MU, improve physician productivity, reduce fraud and errors, and meet New York’s March 2015 e-prescribing mandate. Hydrocodone painkillers such as Vicodin have moved to Schedule II, with the higher CS prescribing volume adding another reason to implement e-prescribing. This webinar will describe why organizations should roll out EPCS, presented from the perspectives of pharmacy, compliance, physicians, and technology.
November 5 (Wednesday) 1:00 Eastern. Keeping it Clean: How Data Profiling Leads to Trusted Data. Sponsored by Encore, A Quintiles Company. Presenters: Lori Yackanicz, administrator of clinical informatics, Lehigh Valley Health Network; Randy L. Thomas, associate partner of performance analytics, Encore, A Quintiles Company; Joy Ales, MHA, BSN, RN, senior consultant, Encore, A Quintiles Company. Data dictionaries, organizational standards, and pick lists for data entry fields may describe the intent of a particular data field, but don’t guarantee that the data captured in the source system actually reflects that intent. Data profiling is the statistical analysis and assessment of the data values in source systems for consistency, uniqueness, and logic to ensure that the data landing in a data warehouse or analytic application is as expected. Attendees will learn which projects benefit from data profiling and the resources needed to accomplish it.
Acquisitions, Funding, Business, and Stock

From the athenahealth earnings call:
- Jonathan Bush says the company is growing, but with growing pains.
- Epocrates is a turnaround in progress and it’s taking longer than the company expected to improve the situation due to major cultural and technical issues.
- Epocrates is moving toward “more of an edutainment relationship where we’re constantly rotating through a set of FDA-approved and clinically appropriate messages for doctors that makes a business act more like a recurring venue business and one-off.”
- The company added 2,800 athenaClinicals physician users, but at a high expense.
- Bush says the challenge of the Enterprise business – which he calls “bipolar” since the company never knows when a big organization will finally sign up – is that internal hospital departments aren’t nearly as interested as the outpatient areas in opening up patient access.
- Bush says it’s hard to sell to academic medical centers: “Nobody gets fired in academic medical. There is no financial mandate. They have got many, many revenue sources, many, many reasons for revenue — the research, the teaching. So that clarity of bottom line is not there. There is somebody in charge of the bottom line who is very clear, but they have grown up an institution that is used to money showing up … an open healthcare network doesn’t help you if you happen to have the highest rates in town … You are not thrill that the doctor and the patient can see the other ones, click on it and rob you of that high-margin encounter … the guys who resist us the most are institutions like Partners, Mass General, where they have historically high rates … and they are terrified of being picked apart.”
- “We are right now in the midst of trying to seed a couple of the major national consulting firms with the idea that its time to change lily pads. That you don’t want to be the last strategic consultant that advise the board of directors to plump down $0.5 billion on a closed system. The problem is there’s a lot of revenue that goes to those firms that way and so we have been working it.”
- Bush expresses frustration in working with (and ultimately bypassing) hospital CIOs, declaring, “Typically the CIO has worked very hard to build board-level access and a great huge budget surrounding the idea of his own data center and his own servers and his own programmers. He is sort of craft brewing milky beer and doesn’t want anybody to compare him with the pros from Dover.”

Above is the one-year share price chart for ATHN (blue) vs. the Nasdaq (green).
People

University of Virginia Health System hires Michael Williams, MD (North Shore-LIJ Health System) as its first CMIO.
HealthMEDX names Chris Dollar (Henry Schein) as COO.
Government and Politics
A HIMSS response to NIST’s cybersecurity RFI says healthcare providers are too focused on HIPAA compliance and should evaluate their overall security instead, adding that NIST should publish a target state for providers to measure themselves against.
Former National Coordinator David Blumenthal, MD says that Texas Health Resources, in first stating but then denying that an EHR flaw caused it to discharged Ebola patient Thomas Duncan, is part of an “inglorious pattern in human behavior” that causes providers to seek scapegoats when something goes wrong. He also says EHRs are the lightning rod for provider challenges because they use them constantly in daily work while other problems seem to be “distant thunder,” but he adds that users are justifiably frustrated with EHR usability and interoperability.
Other
I don’t automatically believe reports from Black Book Rankings, especially when they don’t itemize their methodology, but their survey of 14,000 RNs who use hospital EHRs claims the following results that I don’t doubt a bit:
- Hospital nurse EHR dissatisfaction stands at 92 percent.
- EHR workflow disruption reduces job satisfaction, according to 84 percent of respondents.
- Nine of 10 nurses say CIO and their executive peers choose EHRs based on price or Meaningful Use performance rather than their usefulness to nurses.
- Nine of 10 nurses say the EHR interferes with nurse-patient interaction and 94 percent say it hasn’t helped nurses communicate with other clinicians.
- Three-quarters say the EHR has failed to improve the quality of patient communication.
- More than two-thirds of RN respondents label their IT departments as “incompetent” in their EHR knowledge.
- A hospital’s EHR is one of the top three criteria for choosing a workplace according to 79 percent of respondents, with top-rated systems being Cerner, McKesson, NextGen, and Epic. The lowest satisfaction scores were for Meditech, Allscripts, eClinicalWorks, and HCARE. This statement alone raises a red flag given that eCW doesn’t offer an inpatient EHR, HCARE is (I believe) HCA’s implementation of Meditech, NextGen’s EHR is used mostly by very small hospitals and isn’t likely to have had enough respondents to be judged on inpatient use alone, and McKesson’s users weren’t broken out among Horizon, Paragon, and its other products. The survey’s biggest flaw is not breaking out practice site – ED, ICU, surgery, ambulatory, general med-surg nursing, etc., all of which use broadly (and often incorrectly) labeled “EHR” systems differently.

An interesting article by Clinovations SVP Steve Merahn, MD says that “unstructured” is a bad term when referring to data because it contains the built-in bias that all data should be structured, when in fact the only reason “structuring” data into convenient pigeonholes is necessary is because our ability to analyze information is otherwise limited. He draws a parallel to earlier observations about Internet content vs. data, which is similar to EHR-contained checkbox results vs. useful clinical information:
- Content has a voice. It is written to communicate ideas, make a point, convince. It is personal.
- Content has ownership. Someone created the note from their perspective of authorship as defined by their levels of authority and responsibility.
- Content is intended for a human audience, for human senses to process.
- Content has context. Even the most objective content contains lexical, syntactic, and semantic clues about where the reader should focus their attention — what was important and what was not.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.



I usually roll my eyes at 1/2 of what JBush has to say, but his assessment of academic medical centers could not be more accurate. Perfectly described.
Let’s face it. The EHR at the Dallas hospital was an impediment to the effective and timely thinking by the clinicians. Sure, the information was all there, but, how long does it take to scroll through multiple screens of mind numbing monotony and legible gibberish to find potentially relevant data?
What has yet to be explained is how there could be a temp of 103F after Tylenol and have a doctor’s note state “no fever or chills” as reported by Kevin Sack in the NY Times. Is that an EHR glitch or typo?
Here are questions I would love to learn the answers to concerning the THR Ebola situation: 1. Of the affected nurses, what is their specialty of care? Are they certified RN’s or LPN’s, nurse techs? 2. What area of the hospital was the isolation area, med surg, ICU, infectious disease? 3. Was Duncan their only patient during that time or did they have other patients? What is being done to contact those other patients and their families who might have come in contact? 4. In addition to restricting travel and movements of US citizens who are being actively monitored, why not restrict foreign citizens from W. Africa from entering US?
Excellent recap and balanced analysis on the RN survey of EHR’s on Black Book. The results appear to be far too broad to draw fair conclusions on specific software preferences/satisfaction, though the fact RN’s don’t care for the EHR is not at all surprising. To me, a key itemization point would be the experience of each RN on an EHR platform. Thanks for sharing!
RE: Clinovations remark “unstructured” is a bad term when referring to data. My usual download of this type of content is “string data.” It could be a word, several words or sentences requiring terminology mapping to some target SDO. Just saying…
My wife has been in the hospital for the last three days. The hospital she is in, is a Meditech shop and I have to say it has to be one of the most user un-friendly systems I have ever seen. The nurses have to click through multiple screens in order to perform just one activity and the five-rights process is painful to administer medications. As I go past the nursing station for the floor, I see nurses spending inordinate time in front of a computer screens instead of being in front of patients, despite there being a workstation in every patient room.
Having been on the front end of EHR deployment, it is disappointing to see how ineffective some systems are and yet they have met the criteria for meaningful use, meaningful to what end? I don’t mean to disparage Meditech, but am just relaying my observations as the spouse of an ill wife. Who happens to know something about EHR’s.
What have we done in moving forward with electronic documentation? At some point we need to take a step back and evaluate whether the care we are providing to the patients is better or worse and in whose eyes. The benefits of reduced drug to drug interactions and having evidence-based alerts is all positive outcomes, but have we lost the human touch of a caring nurse who is more concerned about the patient than entering data into a system.
Something to think about an ponder as we as an industry move forward.
Regarding the nurse dissatisfaction with EMR’s. What is the answer then? With this global condemnation of their use, what do nurses want to use, given that the documentation MUST move off paper onto a system. I am not disagreeing with EMR’s not working as well as they could. But with positions that are so cynical (Nine of 10 nurses say CIO and their executive peers choose EHRs based on price or Meaningful Use performance rather than their usefulness to nurses.) what do they want and what are they doing about it as an industry?