I use a wiki and was exploring some of the extended character sets. I was startled to learn that the…
Monday Morning Update 9/22/14

”Behind the Curtain of the Healthcare.gov Rollout,” a report from the US House Committee on Oversight and Government Reform (the committee is wildly anti-Democrat, but still interesting) contains fascinating details of the internal panic once CMS realized they were in way over their heads right after Healthcare.gov went live and failed. It concludes that infighting between CMS and HHS forced the development team to work through US CTO Todd Park, with CMS attempting to hide security exposure, keep HHS in the dark, and insist on a full site launch instead of a phased approach. Some fun snips from internal emails the committee dug up as HHS and CMS people duked it out electronically, sometimes using their private rather than government-issued email accounts:
- [Unidentified HHS employee]” “Your leadership only wanted to hear beautiful music … clearly these people are not smart enough to pull it off … you could definitely see the CYA moves coming a mile away.”
- [Unidentified HHS executive, referring to CMS Deputy Director of IT Henry Chao]: “I grow wear of the bull#### passive/aggressiveness of Henry … the other way to do this is through a complete covert ops mission to unseat the CMS FFE rules engine.”
- [HHS CTO Bryan Sivak, pictured above]: “It’s all negative. I’m going to embark on a campaign to declare victory without fully launching.”
- [HHS CTO Bryan Sivak, responding to an email in which CMS admitted that the site could not handle more than 500 concurrent users]: “Anyone who has any software experience at all would read that and immediately ask what the f## you were thinking by launching.”
- [HHS CTO Bryan Sivak, responding to US CTO Todd Park’s claim that the site’s problems were all related to user volume even though officials knew that wasn’t the case]: “This is a f###ing disaster. It’s 1am and they don’t even know what the problem is, for sure. Basic testing should have been done hours ago that hasn’t been done.”
- [HHS CTO Bryan Sivak]: “1. Bad architecture. 2. Not enough testing. Pretty simply really.”
- [HHS CTO Bryan Sivak, replying to the former HHS employee who transferred to CMS and suggested she might not be much help]: “If you don’t get access, I’m probably going to start being a little bit of a d###, which will give you ample opportunity to badmouth me and gain the trust of people at CMS.”
- [CMS employee, in urging that Healthcare.gov code be removed from open source repositories]: “This Github project has turned into a place for programmers to bash our system, submit service requests (!), and now people have started copying Marketplace source code that they can see and making edits to that.”
Reader Comments
From LL Fauntleroy: “Re: Cerner shops. The number of major ones that have pulled the plug to go with Epic (the industry term is ‘Cernover’) is the best-kept secret in health IT since neither the company nor clients announce it. Some I know from the last couple of years. Loma Linda, Dallas Children’s, Stanford Children’s, University of Utah, John Muir Health System, Connecticut, etc. There are also hospitals pulling the Cerner plug in Australia (Royal Children’s) and elsewhere around the world. There are also a number of shops that run Cerner inpatient but Epic outpatient, or Epic rev cycle, and are rumored to be considering switching, such as Northwestern. Why doesn’t HIStalk write about this?” I’ve written about those of which I’m aware, which is most of these, but I have to depend on readers to tip me off since I’m not omniscient. HIMSS Analytics could verify this trend (if it is one) or identify other Cernovers (or “Epicstinguishes” since surely a few health systems went the other direction), but they aren’t about to tell me for free.

From SoCalSurfLegend: “Re: Prime Healthcare. Three of their southern California hospitals are implementing Epic. Prime is adamant that they will not use consultants. How long before they realize it can’t be done? I’ll set the over/under at three months considering that Prime’s ownership group is the cheapest bunch around.” Unverified. Prime Healthcare’s majority owner is Prem Reddy, MD, an India-born cardiologist who has made a fortune buying and operating financially aggressive hospitals and is known as a generous philanthropist. His wife, daughter, and son-in-law are doctors.

From BJ Hunnicutt: “Re: BJC. My sources say Cerner won the demo round. Allscripts lacked functionality and the reps interrupted their own demo team to inject irrelevant information, while Epic seemed stale and self-important. BJC uses Allscripts inpatient at two academic campuses, Allscripts ambulatory for the medical school faculty clinics, the FollowMyHealth portal, NextGen for employed physicians, McKesson Horizon at the community hospitals, both Cerner and Horizon lab, and Soarian financials. They also have a homegrown clinical data repository and a massive interface support staff to keep it running. The McKesson Horizon situation is probably a key driver. I make Cerner the favorite because of their strong demo and existing relatively new Soarian backbone, plus the two other major health systems in town (SSM and Mercy) have Epic and BJC won’t want to look like they’re jumping on the bandwagon late.” Unverified. BJC’s site says the IT department has a $200 million annual combined budget and 800 employees who specialize in “clinical-based software solutions, integration of disparate systems, and expert systems intended to support caregivers in clinical practice.” Headcount assigned to that middle one seems entirely justified given the apparently lack of appetite for standardizing systems.

From The PACS Designer: “Re: Windows 9. Microsoft announces September 30 as Win 9 day, with a new Start menu, a virtual desktop feature, and a notification center.” Better get out early to camp out a spot in line. Oh, wait, that’s Apple. It’s pretty bad when the most exciting new feature of a highly touted new release is to restore functionality idiotically removed in the previous one.
HIStalk Announcements and Requests
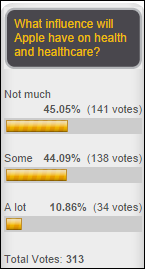
It’s a 55-45 respondent split on whether Apple will have any influence on health and healthcare. Steven Davidson, MD added this comment to his vote: “Apple is the baby boomer tool of choice. Consumers, aka activated, engaged patients are growing in number and power and will adopt tools that enable/enhance their power. Apple wants to be that tool vendor and is the first major (well maybe Nike, but they’re giving up) consumer brand to offer a mostly complete as it is tool set. I think their presence is important and I think the hospitals still don’t get it–with a small number of notable exceptions.” New poll to your right or here: should the MU 2015 reporting period be reduced to 90 days?
Welcome to new HIStalk Gold Sponsor Phynd. The Kearney, NE-based company offers a cloud-based platform that synchronizes provider data from all of a hospital’s IT systems into a single profile, allowing hospitals to accurately answer the question, “Who are your doctors?” that includes billing address, communications preferences, licensing, internal system IDs, exclusionary lists, and contracting. It uses a patent-pending Universal Provider Profile (UPP) for all 3 million US providers, making it easy for frontline users to add a new provider on the fly, also supporting custom fields and taxonomies on any topic and from any IT system. Data quality can be easily determined by each provider’s UPP Score. Folks at Yale-New Haven Health recently did a presentation on how Phynd solved their problems involving 7,000 Epic users and 40,000 referring physicians: outdated credentialing information, endless calls to get updates, manual lookups, and lack of auditability of updates. Thanks to Phynd for supporting HIStalk.

Mr. Fraustro, the California teacher whose classroom got a 3-D printer courtesy of HIStalk readers, provided some photos of it in use. He says the students were excited when they fired it up for the first time and saw the flashing lights, heard the sounds, and smelled the printing filament and realized it exists beyond YouTube videos.

Andy Spooner, MD of Cincinnati Children’s Medical Center wrote another great “CMIO Rant” posts on HIStalk Practice, this one rebutting the AMA’s list of EHR problems with things they could be doing instead of complaining about technology.
Listening: new from Train, complete with their trademark clever lyrics despite a dangerous turn into “background music for work” territory. Extra points for the jangly “I’m Drinkin’ Tonight.” Decent for a band that’s been plugging away for 20 years and is down to just two original members.
Last Week’s Most Interesting News
- Congresswoman Renee Elmers (R-NC) introduces a bill that would allow providers to choose any three-month reporting period in 2014 for Meaningful Use reporting instead of the full-year mandate otherwise scheduled to begin October 1.
- Apple pulls HealthKit-dependent apps from the App Store after finding unannounced bugs in HealthKit that will take at least two weeks to fix.
- The American Medical Association and then its president take shots at poor EHR design and usability.
- Former Kaiser Permanente CIO Phil Fasano joins insurance company AIG in the newly created position of EVP/CIO, with KP VP named as interim CIO as the national search for Fasano’s replacement begins.
- Outsourcer Cognizant announces plans to acquire TriZetto for $2.7 billion.
- An app developer trade group asks HHS via Congressman Tom Marino (R-PA) to make it easier for them to understand and comply with HIPAA requirements, some of which predate the iPhone.
- Epic holds its UGM with over 18,000 attendees on hand in Verona, WI.
- Illinois-based systems Advocate Health Care and NorthShore University HealthSystem will merge to form the state’s largest health system, with a stated expected benefit being the sharing of electronic medical records between their respective Cerner and Epic systems.
Webinars
September 25 (Thursday) 1:00 ET. Using BI Maturity Models to Tap the Power of Analytics. Presented by Siemens Healthcare. Presenters: James Gaston, senior director of maturity models, HIMSS Analytics; Christopher Bocchino, principal consultant, Siemens Healthcare. Business intelligence capabilities are becoming critical for healthcare organizations as ACOs and population health management initiatives evolve in the new healthcare marketplace. The presenters will explain how BI maturity models can help optimize clinical, financial, and operational decisions and how organizations can measure and mature their analytics capabilities.
September 26 (Friday) 1:00 ET. Data Governance – Why You Can’t Put It Off. Presented by Encore, A Quintiles Company. Presenters: Steve Morgan, MD, SVP for IT and data analytics and CMIO, Carilion Clinic; Randy Thomas, associate partner, Encore, A Quintiles Company. In this second webinar in a series, “It’s All About the Data,” the presenters will review the pressing need for data governance and smart strategies for implementing it using strained resources.
Acquisitions, Funding, Business, and Stock

Providence Health & Services launches Providence Ventures, a $150 million venture capital fund that will invest in companies focusing on online primary care access, care coordination and patient engagement, chronic disease management, clinician experience, analytics, and consumer health. It will be led by a former Amazon publishing executive. Providence will also create an internal innovation group to help it collaborate with early-stage companies, run by newly hired VP Mark Long (above), who was formerly CTO of Zynx Health.
Identity and access management technology vendor Ping Identity receives $35 million in venture funding, bringing its total to $110 million.
Announcements and Implementations
The Tel Aviv, Israel-based McKesson Cardiology development group earns CMMI Maturity Level 5, the only FDA-regulated medical device software organization to achieve the highest software process improvement rating. I assume that’s the former Medcon that McKesson acquired for $105 million in 2005.
Other
Cerner and athenahealth say they, like Epic, are working on integrating their systems with Apple’s HealthKit. People seem excited about that for some reason.
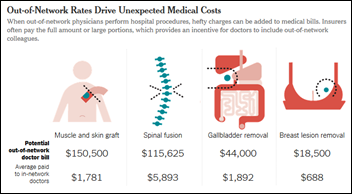
A New York Times article calls out “drive-by doctoring,” where surgical patients receive bills from clinicians called in without the patient’s approval, often billing them at out-of-network rates. A disk repair patient was billed $117,000 by an out-of-network “assistant” neurosurgeon he had never met. Another patient complained that plastic surgeons billed him $250,000 to close an incision and a “parade of doctors” dropped by regularly post-op without mentioning that they were billing him every time they said hello. The article points out that the US has more neurosurgeons per capita than other countries and Medicare is paying them less, so they attend seminars on “innovative” coding and convince other surgeons to fraudulently declare emergencies that require their services. This is bizarre to me: the hospital sent a surgical patient’s blood tests and ECG to an out-of-network lab.
New York Times reporter Elisabeth Rosenthal, who is a Harvard-educated physician (and who also wrote the article above about drive-by doctoring), rightly calls out the silliness (and profit-seeking motivation) of entrepreneur Vivek Wadhwa proclaiming that, “I would trust an A.I. [artificial intelligence]” over a doctor any day” since AI provides “perfect knowledge.” Leave it to technologists to utter some of the stupidest imaginable statements about healthcare, exhibiting their lack of knowledge about medicine and putting unwarranted faith in the inaccurate perception that given endless amounts of unaudited data and enough computer horsepower to churn through it, better outcomes will automatically be obtained (let’s match Watson against a skilled physician instead of a “Jeopardy” contestant in treating an elderly patient with multiple chronic conditions and see who wins). Rosenthal makes great points: (a) slick technologies, including fitness trackers, haven’t affected outcomes or costs; (b) “health” can’t be easily defined with the knowledge we have today; (c) it’s easier to collect data than to know what it means, such as whether low testosterone levels in men are relevant; (d) people die even when their data points are perfect; and (e) it’s easy to find measurable abnormalities in patients who are fine, leaving the choice of treating the measurement or the patient. She concludes that some but certainly not all medical outcomes can be affected by collecting more information:
One central rule of doctoring is that you only gather data that will affect your treatment. There are now devices that track the activity of your sympathetic nervous system as a measure of stress. But what do you do with that information? Other devices continuously monitor breathing for wheezing that isn’t noticed or audible. Does that matter? Some studies have shown that continuous monitoring isn’t useful for children hospitalized with bronchial infections.
If you were dieting, would stepping on the scale 1,000 times a day help you lose weight? Or consider the treatment of an abnormal heart rhythm. It’s true that constant monitoring for a few days can be highly useful to identify the pattern and what provokes the attacks. After that, though, for many patients a wearable cardiac tracker might simply record normal beats that normal people experience all the time, increasing anxiety for many patients.
The Minneapolis paper profiles Peter Kane, founder of two failed healthcare IT businesses (ProcessEHR and Phase-1Check), who since started a co-working space.
Weird News Andy has thoughts about this story, in which a since-fired 33-year-old female nurse is accused in a lawsuit of initiating “unsolicited sexual relations” with a 60-year-old male ICU patient waiting for a heart transplant, which the man claimed had happened with other patients. WNA’s analysis: “Was she so inept that his heart rate didn’t go up, or did alarm fatigue prevent someone from investigating?”
Sponsor Updates
- Validic will announce new clients, integration partners, and connectable fitness devices at the Health 2.0 Fall Conference this week. The company will sponsor a Codeathon and participate in panel discussions.
- Wellcentive will demo its population health management solution at the Health 2.0 Fall Conference.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.





What do you call a Siemens hospital that switched to Epic? Glücklich.
Hey, WNA. Rape jokes? Not that funny.
Epic drones love to make jokes (Cern-over, whatever). Petty, childish, exactly what you’d expect out of a ‘my team’ mentality. As a user of Epic or Cerner you’re faced with essentially the same workflow, the same UX clunkiness, the same menial tasks, roughly the same (massive) cost of ownership.
I fear that both companies are losing sight of innovating within the core EHR (and this spells major opportunity). We’ll see how Intermountain’s costing project shakes out.. and with Mayo on deck things are about to get interesting in the market.
Re: BJC, a Cerner edge would not be entirely surprising. I believe BJC uses Cerner’s iBus for lab instrument interfaces on a fairly large scale. There have been rumblings of broader Cerner opportunities within BJC for a couple years now. Cerner is becoming very good at drumming these deals up once established with a strategic footprint (as with iBus). See also Parkland’s new hospital in Dallas, they’ll be using iBus to interface medical devices to their Epic EHR. No chance of displacing Epic but there are many other avenues Cerner can forge new business. Anyway…
BJC: The list of applications is accurate that is mentioned above, and to vendor_neutral – BJC has previously signed a Cerner Lab deal for the enterprise and uses term positive patient ID which came from Cerner. Neal will also be giving the software away to get the largest Missouri health system on their books.
But so will Allscripts. And Allscripts is already in the academic hospitals, notoriously much harder, longer and more costly to implement.
Regarding the demo rounds going to Cerner, Deloitte is leading the selection process and they always lean Epic. I would say it’s probably a toss up and it will come down to cost. Don’t forget BJC laid off workers and charged co-pays for patients that can’t pay this year, all bad press in STL. A $500+ million EMR install will go over like a lead balloon.