“In extreme cases, I’ve seen vendors refuse to be on calls with the note-taking took turned on.” Rarely see a…
News 12/27/13
Top News
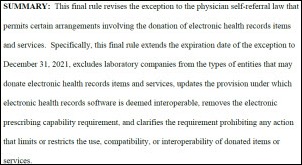
CMS adopts final rules that extend the Stark exception sunset date from December 31, 2013 to December 31, 2021. The amendment allows healthcare entities to continue subsidizing physician purchases of EHRs and includes additional rule modifications, including:
- The exclusion of lab companies from donating EHR items and services
- The elimination of the e-prescribing capability requirement
- Updates to the interoperable provision
- Clarification of the requirement prohibiting any action that limits or restricts the use, compatibility, or interoperability of donated items or services.
HIStalk Announcements and Requests
![]() Mr. H whisked away Mrs. H for a little holiday this week, but he should be back this weekend. We’re about to be in the midst of the pre-HIMSS fury so I am glad he took time for R&R with Mrs. H before the craziness begins.
Mr. H whisked away Mrs. H for a little holiday this week, but he should be back this weekend. We’re about to be in the midst of the pre-HIMSS fury so I am glad he took time for R&R with Mrs. H before the craziness begins.
![]() News was slow on HIStalk Practice this week but you’ll want to check out the letter Dr. Gregg sent to Digital Santa before St. Nick jumped on his sled. Thanks for reading.
News was slow on HIStalk Practice this week but you’ll want to check out the letter Dr. Gregg sent to Digital Santa before St. Nick jumped on his sled. Thanks for reading.
Acquisitions, Funding, Business, and Stock
The HIMSS Foundation and the National eHealth Collaborative merge their organizations and announce plans to create the HIMSS Center for Patient- and Family-Centered Care and to integrate NeHC’s educational and HIE programs with existing HIMSS resources.
PM and RCM service provider Medical Transcription Billing files a registration statement for a proposed IPO.
The Singapore government invests $500,000 in Ring.MD, a telehealth startup focused on improving access to high-quality physicians in Asia. The company was founded by Justin Fulcher, a 21-year-old entrepreneur who has been coding since he was seven and started his first business as a preteen.
Sales
Big Bend Hospice (FL) selects Allscripts Homecare software.
CareTech Solutions will provide consulting services to Medicine Bow Technologies (WY), which is developing a disaster recovery plan for services impacting Invinson for Memorial Hospital.
People
Cerner names former Indiana governor/current Purdue University president Mitch Daniels to its board of directors.
Family Health West (CO) hires Pam Foyster (Quality Health Network) as clinical informatics director.
Announcements and Implementations
Jamaica’s minister of health says his country will being implementation of an $50 million EMR system for hospitals and primary care clinics during the first quarter of 2014.
Maine Medical Center will increase its Epic EMR investment from $145 million to $200 million and dedicate about two-thirds of the funds for additional employee training. Health system officials admit they originally underestimated the resources required for training and may have made a mistake by starting the implementation at its 6,000-employee Maine Medical Center, rather than a smaller pilot facility. Earlier this year the hospital’s CEO said the Epic rollout and incorrect billing issues contributed to a $13.4 million loss in the first half of its 2013 fiscal year.
Weems Memorial Hospital (FL) goes live on its $450,000 EMR from CSS.
Sagacious Consultants launches Sagacious Analytics to help hospitals improve reporting and make better use of EMR data for performance measurement.
Vermont Information Technology Leaders makes radiology and transcribed reports from Fletcher Allen Health Care available to providers via the state’s Medicity-powered HIE.
Government and Politics
CMS announces the formation of 123 new accountable care organizations, bringing the total number of established ACOs to more than 360.
Innovation and Research
A new influenza forecasting method developed by Columbia University’s Mailman School of Public Health is proving almost twice as reliable as traditional approaches that rely on historical data. The system combines real-time estimates from Google Flu trends and CDC surveillance programs.
Technology
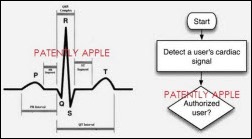
Apple secures a patent for an embedded heart rate monitor for smartphones.
Other
A USA Today article looks at how the adoption of HIT and preventative care are improving healthcare and lowering costs. David Blumenthal, MD highlights areas requiring more work, including moving from fee-for-service payment models to risk-sharing or team-pay systems; improving care coordination through the use of IT; educating consumers on how to choose better care based on quality and lower costs; and, increasing the use of standards to lower administrative costs.
Mount Sinai Hospital (NY) reports a 40 percent decline in its sepsis mortality rate since implementing an early warning system within its EMR. The system triggers an alert whenever staff enter vital signs that match the criteria for early sepsis.
Over two-thirds of HIT professionals participating in a HIMSS compensation survey report receiving a salary increase in 2013; the average reported salary was $110,269. Almost half of the 1,126 survey participants also received bonuses with the median bonus equal to three to four percent of annual salaries.
Sponsor Updates
- NextGen posts its January webinar schedule.
- Optum opens an on-demand health and wellness clinic in Overland Park, KS.
- Imprivata hosts its second user conference HealthCon 2014 May 4-6 in Boston.
- Forbes profiles Ping Identity founder and CEO Andre Durand.
- As the industry shifts to P4P and ACOs, API Healthcare VP of nursing Karlene Kerfoot predicts a shift in healthcare jobs from hospitals to home care agencies, outpatient surgery centers, and urgent care clinics.
- Info-Tech Research Group names Informatica a Champion in its Data Integration Tools Vendor Landscape.
- EDCO posts a video highlighting its point of care scanning process for clinical staff.
EP by Dr. Jayne
It’s a very slow week here since a good portion of our department took vacation days around the Christmas holiday. I’ve enjoyed the relative quiet and am glad to see that people are staying off of email. CMS shared some holiday cheer by emailing providers to remind them that if they didn’t e-prescribe in 2012 or 2013 they will receive their penalty in 2014. I don’t know why they insist on calling it a “payment adjustment” rather than a penalty. Penalties related to Meaningful Use will begin on January 1, 2015 so if you’re going to avoid them you need a solid strategy now.
I’m keeping my eye out for exciting opportunities in the New Year and was interested to see a couple of CMIO postings pop up at organizations that haven’t had a CMIO previously. Although it may be exciting to be the first CMIO and to be able to define the role, I don’t envy anyone taking a job at an organization that is just now figuring out they need one. A couple of the job descriptions were nebulous to the point where I’m wondering if the hospital even understands what they are looking for.
Medical Economics recently did a piece on the survival of the doctor-patient relationship. Physicians cite administrative burdens as the highest threat (41.9 percent) followed by EHR at 25.8 percent. I’m glad the article makes the point that some of the tasks could be assigned to other office staff members. I still struggle with physicians who insist on doing work that could be done by support staff including printing lab requisitions, tracking down test results, processing refill requests, and dealing with insurance paperwork.
The article addresses the EHR challenge more specifically – citing anecdotal stories of physicians who spend 10 minutes of a 15 minute appointment typing. I’m continually surprised by the number of my peers who refuse to learn to type. If you’re going to use free-text rather than structured documentation, typing skills are essential. I remind our physicians that if they mastered biochemistry and tying surgical knots they can learn to touch type but they still resist. I’ve even tried a games-based approach to try to harness their competitive natures, but haven’t had a lot of success.
Another physician states he spends “eight to 10 minutes per chart entering information not directly related to patient care, mainly tied to quality metrics.” Based on conversations with some of our providers I’d have to challenge that statement. We have a large employed provider base and it’s always a shock when someone thinks that a particular clinical quality element is “not my problem” especially in the ACO environment. We’re fortunate to have an EHR where the quality metrics are baked into the documentation – there’s not a lot of extra work to do. I know many sites don’t have this advantage but for us there’s no excuse.
I recently went a couple of rounds with a surgeon who said the patient’s morbid obesity was “not my problem.” I countered that if he plans to do any procedures on her, it certainly is his problem because of the risk of complications directly related to the obesity, not to mention the need to find out if there is diabetes related to the obesity because that alone can complicate wound healing. The same thing applies to our orthopedic surgeons who don’t want to check blood pressures. Fortunately our organization has made measurement of vital signs part of the required elements for physicians to receive bonus payments, so it makes it easier for me to push back at them.
I know there are a lot of EHRs out there where the documentation isn’t so simple and having used a couple of them I’d encourage physicians to look for alternate strategies to make it easier. I did a stint as a locum tenens where the physicians dictate using voice recognition and then staff post-loads the discrete data elements that the system doesn’t recognize. It worked well and the physicians had a high level of satisfaction. Essentially the extra two patients a day they could see by using voice recognition allowed them to pay for the extra staff needed to load the data. It was revenue neutral but the physicians felt better not clicking as much as they used to.
I think the key to managing quality indicators is having a plan on when they are going to be addressed. I see a lot of physicians struggling to try to address every indicator at every visit and it’s just not necessary. My EHR allows me to filter and only see those items that are due in the next three months, six months, etc. so that helps somewhat. Our group also has policies about when the indicators are to be addressed. For example, patients in for an annual preventive visit should have all preventive services due during the next 18 months addressed. This covers them for the next year and a little bit extra should their return appointment be delayed.
The article also cites the amount of time needed to have a conversation with the patient about screening services as a barrier. We provide extensive training to our medical assistants (no nurses in our world) on how to address preventive services with patients during the intake and rooming process so that the patient knows it will be a topic of discussion. The staff can provide educational materials for the patient to read before the physician enters the room, which can make some of those conversations easier and faster. Additionally, providers are not expected to address all preventive services on acute visits. We rely on our automated outreach mechanisms to catch those patients who don’t come in for preventive visits or who have lapses in care. This has been a major physician satisfier because the acute visits remain fairly quick and they don’t have to spend time worrying about patients falling through the cracks.
Having policies on when to address what kinds of services doesn’t have anything to do with the EHR – we actually had these policies in place in the paper world – but they’ve made a great deal of difference. We also provide training for support staff on completing pre-authorizations and pre-certifications so that work can be handed off even in a small office that doesn’t have dedicated referral staff. Looking at the operational workflow and staff training has helped physician satisfaction and hopefully will be one of the things bolstering the patient-physician relationship in our organization. Does your organization have any secret recipes for success? Email me.
Contacts
Mr. H, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis, Lorre
More news: HIStalk Practice, HIStalk Connect.









If the Maine Medical Center is adding another $55 million to its Epic budget and two thirds of that is going to installation costs, that’s $36 plus million in additional installation fees. At $180 dollars an hour that is an additional 200,000 hours to install the Epic system. Assuming the original budget was $36 mil for installation, that makes the total 400,000 hours to install the system or approximately 200 person years.
I have worked inHIT for nearly 40 years and am having a difficult time understanding how new systems, which are intended to be intuitive to use, can require this much effort to install.
Carl I think you’re intentionally distorting. The bulk of that money funds backfill staff while nurses go to training. In a safety critical world where patient lives and hundreds of millions in malpractice, not to mention business disruption are at risk if you mess up and go live all at once without being reasonably trained this makes good sense.
Would you fly in a 737 with a pilot who had never flown one before, but had logged many hours on a Cessna? Or would you prefer he or she sat through a day or so of training on it first? Now let’s assume no one on that 737 had ever stepped foot on that plane before. How much would you value training then?
“which are intended to be intuitive to use”
This is the problem. Few, if any of the current generation EMR’s are designed to be intuitive to use. I have heard many, many things said of Epic (both good and bad), but intuitive to use is not one of them.
“Would you fly in a 737 with a pilot who had never flown one before, but had logged many hours on a Cessna? Or would you prefer he or she sat through a day or so of training on it first?”
Something tells me that the cockpits of airplanes are a heck of a lot more standardized than the displays of EHRs. With EHRs colors, icons, locations and just about everything else in the user interface is different (“custom”) from system to system, implementation to implementation.
Airplanes and airplane cockpits are also tested for usability, specifically freedom from “use error” or aspects of the UI design that could induce users to make mistakes. EHRs not so much.
And we wonder why it costs to so much to implement and train people on these systems.
Users blame the vendors and IT department. The IT department blames the clinicians and vendors. The vendors just say that they’re doing what the people who buy their systems want.
What do we do to move forward?
The Maine Health headline should read..”Local Health System throws more good money after bad in EHR Debacle” or if I was from Maine (which I’m not) it probably should have read “Loud sucking sound at Maine Health, limited local financial resources displaced to Wisconsin, bolster Billionaire’s ego”
I’m so sick of hearing the exact same things come up whenever MH is mentioned. I worked on the project for 4+ years, and I can tell you that we humans don’t have enough fingers to point out all of the parties that deserve blame.
Trainers – We all lost track of how many trainers and came went during the course of the project.
Epic People – They couldn’t quit the company fast enough, and every replacement was younger or less experienced than the ones that left.
Epic Project Management – Changes happened on the top ranks of the Epic side of the project.
MH Project Management – Changes happened on the top ranks of the MH side of the project.
I’m more than happy to address some questions here (maybe not all…?) but I have a feeling both Epic and MH won’t like their laundry being aired…
Cockpits are wildly different in many ways.
https://www.google.com/search?hl=en&site=imghp&tbm=isch&source=hp&biw=1462&bih=686&q=airplane+cockpits&oq=airplane+cockpits&gs_l=img.3..0j0i24.1692.5682.0.6682.17.13.0.4.4.0.130.1058.11j2.13.0….0…1ac.1.32.img..2.15.850.RQHLqSiFQrs
Search google images for “airplane cockpits” and marvel at the vastly different arrays of instruments, switches, indicator lights, etc.
Are some instruments standard? Certainly. But different planes have different capabilities, systems and controls. And, they require an operator to have a basic understanding.
Pilots are checked out on airplanes before passengers put their lives in their hands. When they aren’t trained enough, you get situations like this: https://www.youtube.com/watch?v=OAwMOeAQxCw
The NTSB clarified that the pilot flying, in the left seat, was in training and that the instructor pilot, in the right seat at the time of the crash, was the “pilot in command”.[21]
http://en.wikipedia.org/wiki/Asiana_Airlines_Flight_214
Oh, so Ron, your question – “What do we do to move forward?”
That’s a good question. I’m not certain where “vendor bashing in blogs” should be on the list, but I’m not thinking it’s the most helpful thing we could be doing.
Using industry wide common vocabularies is already starting to have an impact. It would be nice if we settled on one national drug standard with alert files and contraindication files we all agreed upon with a sensitivity by specialist so we don’t have to blast people to death with alert fatigue.
We could standardize a few more workflows through some of our specialty societies so EMRs could behave “as expected” or more “intuitive” as users moved from one institution to another.
We could agree on a standard patient header / addressograph type display.
Many things on a productive path. Let’s start simply and move!
Broken Record, I think you’re comments are invaluable… people rarely want to share what really happened during implementations, but that’s the only way we learn and get better. What are your thoughts on what was driving all the turnover? Was there something about MH, or do you think that is typical for Epic implementations? Any other factors you can share with us?
Airplanes – while there is certainly plenty of variation in cockpit display systems, there’s plenty of standardization (where it matters, especially for safety). There is active commitment and collaboration between Boeing and Airbus (among others) on critical aspects of cockpit standardization in new systems.
In aviation, crashes rarely occur and there is an NTSB in place to investigate and gain understanding of what factors contributed to the crash. While not perfect, lessons (whether they be issues with the human-machine controls that induced error or issues with training or maintenance) are made public, widely disseminated and acted on (where appropriate) by regulatory bodies.
In EHRs there is no standardization. The color red means equal and opposite things in two different systems. Vendors have no appetite for collaboration, even in areas that are safety critical.
While we know that they occur, we have precious little data on the frequency or severity of health IT related harms. There is no NTSB for health IT (or healthcare). Vendors contractually block the sharing of information that could result in better, safer products, training programs, implementation processes, etc. There is no regulation of EHR systems beyond voluntary certification.
Vendors point fingers at their customers (they implemented it badly). Healthcare organizations point fingers at their vendors (the product is poorly designed, complicated to interface, buggy and implemented by teen-agers). Both point fingers at the government (there’s simultaneously too much / too little regulation and the billions of dollars of stimulus money handed to the industry has ruined the industry). Patients (and users) suffer. The status quo continues.
What is keeping the collective stakeholders from collaborating on a standard patient header / addressograph type display?
A few of my opinions (strong emphasis on the ‘my’ and ‘opinion’ part) on your question about turnover and other factors from my view of the project.
Some of the turnover on the Epic side seemed to be standard issue company departures of employees around the 3 year mark who were burnt out as well as the newbies who became burnt out after learning their job would require 60+ hour work weeks in addition to traveling more than they were initially told about. Other departures ranged from freak accidents (the sudden death of a 22 year old new hire) to MaineHealth not feeling an Epic person was the right fit and having them removed from the project. On the MaineHealth side, a number of people came and went on the project team as we discovered that Epic training and certification didn’t actually prepare us for what we needed to do, or that some people were selected for the project based on knowledge of how the system ‘should’ work, but not any knowledge about technology or how to build a new system.
Actionable lessons learned or suggestions about avoiding burnout and putting the right people on the team: Epic is hard. Learning Epic is harder. Learning how to customize and build an Epic system is the hardest. If I were building a new hospital-side project team for an Epic project, I’d be looking for the best and brightest of my staff that is technologically savvy, NOT the people in my organization who know the most old clinical workflows, old billing procedures, or registration workflows. Installing Epic is not a simple copy/paste job and will require intensive logic and operational thought processes as you rebuild the END PRODUCT of your old system. Note the bold words. One of the problems we ran into at MaineHealth was that we rebuilt the old system in the new system, but this time around it didn’t account for all of the bandaids and patchwork solutions that were apparently happening as data flowed across each of the legacy systems.
As for training related topics recently discussed by MaineHealth leadership and on this site – it is true that MaineHealth did not give the right priority to training during the installs. On the Epic side of things, it was very clear that training was an afterthought by the Epic ACs as they became more and more overworked with their three different customers. On the MaineHealth side, there were a number of trainers that came and went over the years. From what I have gathered most assumed we were using standard Epic Model workflows and didn’t customize very far from the Epic ‘Training Wheels’ material. Instead we did very little that was ‘Epic Model’.
Actionable lesson learned: Integrate your trainers into your integrated testing, unit testing, and bring them to project team meetings when applicable. Do not isolate them. Make them familiar faces with your operational leadership. MaineHealth made the mistake of hiring and finalizing its trainers much later into the install when some of these things weren’t possible.
Other thoughts: Despite what you may read on this website’s comments section, Epic DOES know what they are doing and many of their recommendations come from years of its success AND failures. We made a decision years ago to have multiple service areas across each of our physical locations. We then decided to bring everything under a single service area right before a go live and had to delay as a result. They told us the implications of each option and let us make the decision, but didn’t completely stand in our way and stop us from making a decision that would ultimately get in our own way. We did eventually make a choice that they recommended, but after it was too late. There are other instances during the course of the install that are very similar. Epic attempted to keep a strict schedule for us with the build of our CDM, but as we debated and discussed just how many organizations we were consolidating from, the deadline was pushed further and further back. No CDM, no Build. No Build, no Testing. No Testing, no Integrated Testing. No Integrated Testing, no Training. Some of the dominos that fell after go live were placed many many years before anyone actually saw the action.