It’s long been known that women make many healthcare decisions for their families, if not the majority of healthcare decisions. A study published last month in JAMA Network Open shows that patients who are female or who have chronic illnesses are more likely to use telehealth. The data in question is from 2002 and was part of a cross-sectional study of 5,400 adults where 43% had telehealth visits during that year. Video visits were less common among patients aged 65 to 74 and those without Internet. The authors found no differences when patients were segmented by education, race/ethnicity, or income. Other interesting tidbits included the fact that nearly 20% of patients reported technical difficulties and that 30% of telehealth visits were conducted using only audio connections.
From Doomsday Prepper: “It’s not just the bulging cans anymore. Did you see this writeup about the CDC investigating counterfeit Botox that’s giving people botulism?” I have to admit I don’t spend as much time in the epidemiology literature as I once did, but it looks like patients in the pursuit of youthful appearances may be turning to low-cost or unlicensed providers who are placing them at risk of serious illness. The Centers for Disease Control announced that it is looking into incidents in nine states where 19 people have reported serious illnesses following botulinum toxin injections. Affected patients may have visual changes, trouble swallowing, or even breathing problems. Symptoms were severe enough in 60% of the patients to warrant hospitalization. Patients can protect themselves by asking if providers are licensed and trained to administer the injections, and whether they’re using FDA-approved products obtained from a reliable source.
I’ve spent more than a decade working with organizations that span multiple time zones, so I’ve had to be continuously conscious about how I schedule meetings. Ideally, employees will specify their working hours in the organization’s calendar application, but I’ve seen several articles recently about whether “8 am meetings” should be done away with. The phrase implies that the time would be 8am for the majority of employees, but in a distributed organization 8 am on the east coast could be 5 am on the west coast, or even earlier for employees in Hawaii. Early morning meetings can make for difficult childcare arrangements – as someone who used to have to round at 6:30 am, I feel that pain acutely. Although healthcare organizations run 24×7, I’ve seen more of them opting to avoid early morning or late afternoon meetings in order to create more flexibility for employees.
Although I’m supportive of making team operating agreements around meeting hours (and even banning meetings at certain times, like Friday afternoons, when everyone’s out of brain cells) I think it’s even more important to make sure meetings are necessary, well-planned, and well-executed. One of my favorite organizations to work with has questions people have to walk through before scheduling meetings. For example, if there are multiple people from the same team invited, do they all have to be there, or can one person represent the team? Is there an agenda that includes expected discussion points and anticipated outcomes? Who will document minutes and action items so that those who are not in attendance know what happened? It seems simple, but the majority of organizations I work with have little to no framework for productive meetings. That same organization has also implemented a policy where meetings are scheduled in 20- or 50-minute increments, allowing people to check email, take care of personal needs, or just decompress when they’re subjected to back-to-back meetings. With those breaks in place, there’s an expectation that meetings start and end on time, which I’m sure everyone appreciates.
In the spirit of “what goes around comes around,” telehealth company Cerebral gets hit by the Federal Trade Commission with a multimillion dollar fine for deceptive practices around data sharing, security, and cancellation policies. In addition to the fine, Cerebral will be prohibited from using health information for advertising purposes. Cerebral is widely regarded by physicians as having contributed to overprescribing of ADD and ADHD medications and a subsequent shortage of those medications for patient use. Although they’re not getting the smackdown for that, they are being penalized for providing sensitive information to third parties including patient demographics, medical and prescription histories, IP addresses, and more.
They were also cited for mailing postcards to patients that included language revealing diagnosis and treatment information for anyone to see, allowing former employees to continue to access health records, allowing non-providers to inappropriately access patient records, and having a faulty single sign-on process that allowed patients to see the sensitive health information of other patients during simultaneous logins to the company’s patient portal. The company will pay $5 million for consumer refunds, a $10 million civil penalty, and a $2 million penalty due to inability to pay the full amount. The company will also have to place notices on its website about the allegations and its ongoing mitigation plans. It feels a little like putting Al Capone in jail for tax evasion rather than other crimes, but given the damage this company has caused to patients and their families, we’ll take it.
The American Medical Informatics Association is conducting a survey on documentation burden among health professionals. The AMIA website lists the primary goal of the survey as being “to capture perceptions of excessive documentation burden across various healthcare disciplines frequently (e.g., every six months) to trend changes over time.” The survey is open through April 26 and will reopen in August. Licensed and unlicensed health professionals who provide patient care and document in an EHR are invited to participate. The survey took less than two minutes to complete.
I didn’t know much about public health informatics until I began to prepare for the initial Clinical Informatics certification exam more than a decade ago. As I read a couple of textbooks that covered the field, I found myself fascinated by the ability to use data to drive health outcomes. Fast forward a few years and we found ourselves living in a public health research project, and informatics efforts in the field accelerated dramatically. The CDC recently updated its Public Health Data Strategy to include addressing gaps in public health data and to reduce the complexity of public health data exchange. Although we’re seeing improved funding for public health informatics efforts at the federal level, it’s still a patchwork when you look across the states. Some of the state-level efforts in public health are pathetic, which is a sad commentary on how those states value the individuals living and working within their boundaries.
What is your community doing to support public health? Leave a comment or email me.

Email Dr. Jayne.




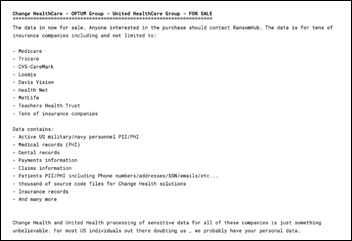




















RE: Change HC/RansomHub, now that the data is for sale, what is the federal govt. or DOD doing to protect…