I'd never heard of Healwell before and took a look over their offerings. Has anyone used the products? Beyond the…
Monday Morning Update 4/12/21
Top News

US News & World Report highlights the legal efforts of Hoag Memorial Hospital Presbyterian to leave the 51-hospital Providence system, saying the chain’s use of Epic to standardize treatments for cost effectiveness often conflicts with the judgment of Hoag’s clinicians.
A Hoag cardiologist says the hospital can’t set its own treatment choices and instead is “bogged down by a bureaucracy that requires 51 hospitals to vote on it.”
Providence says the hospital knew that collaborative standardization was part of the affiliation deal.
Hoag also says that Providence illegally imposes restrictions on reproductive care by adhering to tenets set by the Catholic church, which controls four of the country’s 10 largest health systems.
Providence doesn’t own the hospital, but appoints a legal majority of its governing body. It says it will allow Hoag to disaffiliate if it pays an undisclosed amount that Hoag says is unreasonable.
HIStalk Announcements and Requests
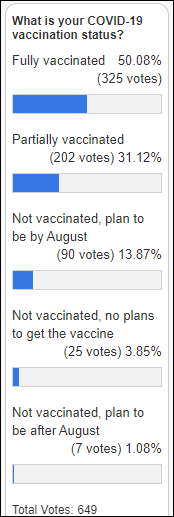
Eighty percent of poll respondents have received at least one dose of COVID-19 vaccine, while 95% plan to be vaccinated by HIMSS21.
New poll to your right or here: Which has contributed most to your overall health? Readers who resent the “one best answer from the list” form of a poll (as opposed to a survey or personal interview) will wail about not being able to choose more than one answer, that health factors are inextricable, or that the provided answer choices are subjective, but work with me.
Webinars
April 20 (Tuesday) noon ET. “The Modern Healthcare CIO: Digital Transformation in a Post-COVID World.” Sponsors: RingCentral, Net Health. Presenters: Dwight Raum, CIO, Johns Hopkins Medicine; Jeff Buda, VP/CIO, Floyd Medical Center. A panel of CIOs from large health systems will discuss how the digital health landscape is changing and what organizations can do now to meet future patient needs. Moderator Jason James, CIO of Net Health, will guide the panelists through topics that include continuum of care and telemedicine, employer-provided care delivery, consumerization of healthcare, and sustainability and workforce management.
April 21 (Wednesday) 1 ET. “Is Gig Work For You?” Sponsor: HIStalk. Presenter: Frank L. Poggio, retired health IT executive and active job search workshop presenter. This workshop will cover both the advantages and disadvantages of being a gig worker. Attendees will learn how to how to decide if gig work is a good personal fit, find the right company, and protect themselves from unethical ones.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock

Reuters reports that Microsoft is in advanced discussions to acquire Nuance for $16 billion, with an agreement possibly being announced on Monday. The reported offer is $56 per NUAN share, a 23% premium to Friday’s close.
A private equity publication sets the value of KKR’s acquisition of a majority position in Therapy Brands, which sells 19 behavioral health EHR/PM systems, at $1.25 billion.
Sales
- HHS extends TeleTracking’s COVID-19 hospital operating data collection and reporting for a third six-month term, presumably for another $10 million.
Announcements and Implementations
Varian and Google Cloud will develop a diagnostic platform for organ segmentation for radiation therapy, training Google’s NAS technology on Varian’s treatment planning image data.
FDA approves GI Genius, an AI-powered tool that highlights possible lesions in real time during colonoscopies.
MIT highlights the work of its Data to AI Lab on Cardea, an open source framework that uses FHIR to connect to EHR data to answer on-the-fly questions, for now focusing on resource allocation. The team notes that hospital decisions are too critical to simply present a black box answer, so Cardea will show the strengths and weaknesses if the model, then allow the user to start over.
COVID-19
CDC reports that 45% of American adults have received at least one dose of COVID-19 vaccine, along with 78% of senior citizens. Slightly interesting is that the three states with the lowest vaccination rates per capita are contiguous and are often challenged in other public health areas – Mississippi, Alabama, and Georgia, with Mississippi in particular being flooded with available vaccine doses that few residents want.
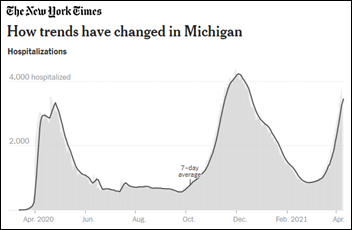
Hospitals in COVID-overwhelmed Michigan are banning visitors, cancelling elective procedures, and re-implementing pandemic surge plans, as two dozen hospitals have reached 90% capacity and 15% of the state’s hospital beds are housing COVID-19 patients. Six counties in metro Detroit are reporting their highest numbers of COVID-19 patients since the first weeks of the pandemic last year. State health officials received 58 outbreak reports from restaurants and stores in the past week, warning bluntly that “indoor dining is one of the riskiest things you can do.”
Meanwhile, the White House says it won’t surge COVID-19 vaccine supplies to Michigan because population-based distribution is the only fair way to allocate supply, especially since new outbreaks could occur elsewhere.
Pfizer requests that FDA expand the Emergency Use Authorization for its COVID-19 vaccine to those who are 12-15 years old, citing Phase 3 clinical trials data of its effectiveness.
A large study finds that people who have had COVID are 84% less likely to be re-infected over at least seven months.
Early reports showed that few people with chronic respiratory disease were being admitted with COVID-19, leading to speculation that inhaled glucocorticoids might be an effective treatment. A small randomized trial concludes that early administration of inhaled budesonide to COVID-19 patients reduced the need for urgent interventions and reduced recovery time.

The New York Times profiles 66-year-old Kati Kariko, PhD, whose early messenger RNA work at Penn failed to draw research dollars and resulted in her moving from lab to lab and never earning more than $60,000 as a low-level, untenured PhD whose job was always at risk. Moderna and Pfizer finally took notice and used her technology to develop their COVID-19 vaccines.
Other
In Canada, a man has struggled since January to remove an incorrectly entered drug overdose from his electronic medical record after the real OD patient, who didn’t have ID, gave paramedics a name and birthdate similar to his own. The health authority says it has removed the entry, but Kevin Robinson says that while the overdose no longer appears on his patient portal display, his doctor says they can still see it.
Cape Cod Healthcare (MA) goes through the technical and legal steps that were necessary to accept donations in bitcoin, as requested by a donor who has transferred $800,000 to the hospital in two transactions. The hospital converts the bitcoin to dollars that it banks immediately, concerned that unlike other forms of donations, its value could swing dramatically.
Sponsor Updates
- PatientBond completes its study on COVID-19 vaccinations.
- PatientPing publishes a new white paper, “Real-time, Right Partner: How One SNF Chain Uses Real-Time Alerts to Succeed in Value-Based Care.”
- PerfectServe publishes the complete guide to “Clinical Collaboration Systems for Hospitals.”
- Pure Storage is a 2021 Customers’ Choice in the “Gartner Peer Insights Voice of the Customer: Distributed File Systems and Object Storage” report.
- Spirion wins three gold wards in the 2021 Cybersecurity Excellence Awards and four Globee Business Awards in the 2021 Cyber Security Global Excellence Awards.
- The Chartis Group names Michael Brown (MD Anderson Cancer Center) director in its Oncology Solutions Practice.
- Vocera earns Cyber Essentials Plus Certification in the United Kingdom.
- Waystar earns HITRUST CSF Certified status.
- Wolters Kluwer Health launches the open access journal Otology & Neurotology Open as part of its publishing collaboration with Otology & Neurotology Inc.
Blog Posts
- How provider orgs need to respond to 2021’s cybersecurity threats (Capsule)
- Leveraging AI to improve patient safety in the emergency department (Nuance)
- ONC 2021 Annual Meeting: Moving towards meaningful communication (Nordic)
- 5 Steps to Take Now: FCC Released 7 Day Application Window for $250M COVID-19 Telehealth Funding (Pivot Point Consulting)
- Reduce Claim Denials with Real-Time Eligibility (PMD)
- After COVID-19, Many Challenges Will Remain (Medsphere)
- Switch to Value-Based Model Saves California Hospital $7 Million (Premier)
- How Smart Rules Can Help Close the Gap Between Clinical Documentation and Coding (RCxRules)
- How New Rules Enable Informed Decision-Making and Patient-Centered Care (RxRevu)
- HIPAA-Compliant Messaging in the Age of COVID-19 (Spok)
- How COVID-19 is Changing Search Marketing (Krames)
- A Health IT Expert on Navigating the System to Find the Best Drug Cost (Surescripts)
- Niagra Health Reduces Number of Injuries in Code White Emergencies by 20% – Staff Feel Safer While They Work (Vocera)
- 5 Fast and Cheap Ways to Fix Your Clinic’s Marketing (WebPT)
- Time Consuming Administrative Processes Cost Healthcare $39 Billion Annually (Vyne Medical)
- Making the Case for Evidence-Based Chronic Condition Management Clinical Decision Support (Zynx Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



RE: Meanwhile, the White House says it won’t surge COVID-19 vaccine supplies to Michigan because population-based distribution is the only fair way to allocate supply, especially since new outbreaks could occur elsewhere.
Seriously? Am I missing something here? If one state has a higher population, but lower Covid rates and positivity and another state has lower (or even same) population but rising Covid cases/positivity, why would you not get ahead of the problem and send an increase supply of vaccine to the state with rising Covid cases?
I’m sure somebody on this blog will school me if I’m missing something here!
What I’m thinking here is Just In Time supplies.
I don’t know either. I think Michigan has low per capita positivity compared to most states. But they have a large number of new infections. In some sense they are catching up to the rest of the country in per capita infections.
At this point, allocating more vaccines to Michigan means either taking them from a state who would have made effective use of them or taking them from a state that doesn’t use them but is governed by the opposing political party. Ideally vaccine distribution does not become a political process.
This is a tricky issue and I definitely advocate for fair distribution regardless of political affiliation. However, I have a good friend in Michigan as I type this, saying that many residents are essentially ignoring the pandemic.
In my opinion, states or counties that have not kept mask mandates, or limited gatherings, or taken other advisable precautions despite the vast body of evidence that it would reduce infection rates, cannot justify being given the vaccine supply of other states that have done those things consistently. There are millions of people across the country following distancing guidelines, not eating in restaurants, not having parties, etc, and still awaiting their vaccine. I don’t see a way to take supply from states diligently working through vaccinating their population to more quickly protect people who are disregarding safety measures.
Those maskless people are turning into reservoirs of virus mutation though, so the fallout of their behavior isn’t limited to them. As satisfying as it might be (and I am as guilty of it as anyone) to sit back and be smug about people “bringing it on themselves” the reality is we are all going to pay the price for their negligence. Until and unless we can seal them into a bubble with each other, we’re stuck with the outcome of their reckless and frankly sociopathic behavior. I’d rather not have to go through this exercise every six months while various mutations cut through the global population like a scythe, so from a purely selfish perspective, I’d think we would all want vaccines in the arms of the people in hotspots.
Here’s what I think you are missing.
Imagine Covid like a fire. There are 2 houses on fire, one that is really blazing away, and one that is really small. Tiny in fact. Where do you allocate resources?
You send the majority of your firefighting resources to the big fire. It’s the greater danger, even if the house is lost. The fire can spread, and it will spread.
“Getting in front of” a Covid outbreak is actually a great idea. When you have lots of vaccine. That’s the deal-breaker; we don’t (yet) have enough vaccine to do those sorts of things. Eventually we may be able to implement ideas like that but not now.
Re: Hoag.
A hospital in Orange County (with cash–rich patients who are willing to come up out of pocket to pay for healthcare) has more ability to consumerize healthcare and give patients every option and ultimately, deliver what the patients want.
Providence has facilities that can’t do that.
But does that really change the ‘standard’ of care?