'Samantha Brown points out that, “Healthcare, like every other industry, gets caught up in the idolatry of the ‘innovators.’”' I…
Weekender 6/12/20

Weekly News Recap
- A new investment in workforce management software vendor QGenda values the company at $1 billion.
- Conversa, PatientPing, Wellsheet, and Kyruus announce significant new funding.
- Only three states have committed to using COVID-19 contact tracing apps from Apple and Google.
- GAO says the VA is doing a good job of getting clinicians involved in its Cerner implementation, but suggests choosing broader representation at its local workshops.
Best Reader Comments
If the medical record is not reconciled, then the source system is part of the problem. However, I have yet to see a system that has entanglement of the data that has been exchanged. Meaning that if Clinic A provides a referral for a preliminary diagnosis and the specialty adjusts the diagnosis and adds a new diagnosis, is the provider notified? That is the goal of 360x, but how many have implemented it — Cerner, Epic ? (Brody Brodock)
Once there are only a few EMR vendors left, then you can start telling your customers that they can’t do the thing in a way that prevents interoperability. The government could mandate that the EMR companies provide interoperability, but it either won’t work or will drive certain EMRs out of business. The situation is FUBAR in that respect. The problem is that healthcare delivery and organizations just aren’t that standardized and process oriented. They’ve never been exposed to the sort of environment that produces that. What we need isn’t a technology standard, it’s a process standard. As an example, accountants use GAAP so that they can calculate the revenues, losses, etc. for their company. When someone tells me their GAAP deferred revenue, I know what they mean and how they calculated it. When someone tells me that a patient has an active medication in their chart, I don’t have a good idea about what that means. (IANAL)
Due to my own illness that I’ve been dealing with for a decade plus, during the COVID surge, I’ve had five telehealth visits, one with PCP, others with specialists. Each started right on time, each accomplished what was needed effectively and efficiently. I dread the thought that there may be a retrenchment of telehealth and I’m forced back to in-person visits. I will resist. (John)
I’ve been in healthcare tech for over 30 years, sat on the HIMSS board, and been a member until 2016 when I came to the decision that HIMSS only cares about three things, money, promoting its own agenda, and removing alternate opinions from the dialogue. Until its membership and that of the vendor community wakes up and understands that those simple truths about what motivates HIMSS or its current leadership, nothing will change. I agree with HIStalk that HIMSS more than likely cannot afford to refund the money it collected without digging deep into the leadership’s compensation and its political machine lobbying Capitol HSill. It is my belief that its time to abandon HIMSS and allow it to either make it as a for-profit organization, which is what it really is verse it hiding under the veil of a non-profit, which it hasn’t been for decades. The educational aspects of HIMSS can be easily replaced by regional groups who can provide localized and national educational content by collaboration and by working with vendors who in lots of instances will pick up the costs. The vendors can form their own association with dues and hold an annual conference that they own, manage, and set the time and place. This would reduce costs all the way around facilitate greater transparency. (HIMSS Insider)
I’m pretty comfortable with a hospital firing a nurse who openly wishes for the death of people she doesn’t like. She is not able to fulfill her job functions. Not only did they do the right thing in firing her, if I were them, I’d also go back and do detailed reviews of all patient cases that she handled to look for irregularities or disparities in the care (“care”) she provided to people — before someone recognizes her as having been on a care team responsible for them or for a family member and starts asking questions about a bad outcome. (HIT Girl)
Watercooler Talk Tidbits

Readers funded the Donors Choose teacher grant request of Mr. H in California, who asked for a computerized scientific calculator for his high school class. He reported in mid-February, “Because of your donations, my students will be able to learn about how an advanced graphing calculator works and get experience using this technology that will be an important aspect of their future math classes. Our school does not have the resources to provide all teachers with class sets of graphing calculators, but with this project, I can begin to teach students about how to use this advanced technology and provide exposure to it they will remember in their future math classes. In order to support future students in STEM subjects, students need to be familiar and have experience using technology and your donations have made that possible in my classroom.”
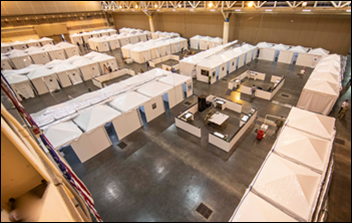
Creation and operation of a 1,000-bed COVID-19 field hospital in the New Orleans convention center cost $192 million, three-fourths of that provided by federal taxpayers. Occupancy peaked in early April with 108 patients and officials kept extending the contract even as patient count dwindled. Nurses who had nothing to do were paid $243 per hour with a guaranteed 98-hour workweek with time-and-a-half for overtime. The bored staffers volunteered to leave, but were told that it was a government contract and to keep showing up to sit around.
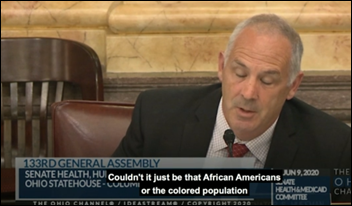
Healthcare staffing provider TeamHealth fires ED doctor Steve Huffman, MD, who is also an Ohio state senator, who asked during a public hearing on racism, “Could it just be that African Americans or the colored population do not wash their hands as well as other groups?” He defends his question as relevant to public health, and while admitting that he worded his question awkwardly, says “colored population” seems to be interchangeable with “people of color.”
Michigan’s Medicaid medical director is reprimanded and fined after admitting that he did not use the state’s prescription drug monitoring program system when prescribing opioids in his private practice.
UF Health Jacksonville suspends a 72-year-old doctor following complaints that he groped female patients, stashed money in their underwear, and undertook his examination of a 70-something woman’s neck mole by kissing it.

NBC News finds that Facebook’s feel-good TV ads that featured members of its Groups expressing support for healthcare and other frontline workers was faked, with none of the feature postings coming from actual Groups. Facebook admits that it mocked up the posts using stock photos and its own employees posing as group members, which it says was due to privacy concerns. The non-fake “Cheers For the Frontline!” group, unlike its happy TV counterpart, is struggling with spammers and trolls.

Doctors remove a mobile phone charging cable from the urethra of a man who told them, unaware of the anatomical impossibility of his declaration, that he swallowed it. Trust me that you do not want to watch the doctor’s Facebook-posted video of the removal procedure.
In Case You Missed It
- News 6/12/20
- EPtalk by Dr. Jayne 6/11/20
- Readers Write: An Interoperability Data Challenge — Out and Back Demonstrating Reflection
- News 6/10/20
- Curbside Consult with Dr. Jayne 6/8/20
- Monday Morning Update 6/8/20
Get Involved
- Sponsor
- Report a news item or rumor (anonymous or not)
- Sign up for email updates
- Connect on LinkedIn
- Contact Mr. H



Interesting comment by HIMSS Insider. Does it take you back about 30 years? The wheel just keeps going around and the more things change the more they become the same. Have a great day. Tim, I really enjoy reading your stuff. The only thing I regret, is that the names of people I recognize appear fewer and fewer times. I guess we are all going away.
Be well, and keep going,