I want to add the following. I'm an IT professional. In the course of my professional duties, I'm expected to…
Monday Morning Update 3/30/20
Top News
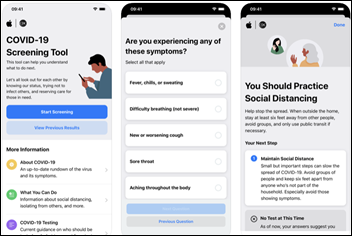
Apple develops a COVID-19 screening website and app that it developed in a partnership with the CDC, the White House’s coronavirus task force, and FEMA.
Reader Comments
From Think Outside the Box: “Re: HIMSS conference. Here is a novel idea.” Here’s what TOTB recommends, which I’m excerpting a bit:
- The vendor community could put on its own conference at cost.
- Vendors could set up a non-profit that any vendor could join for $25. The group would assign officers who use their own contracting, project management, and marketing groups to run the conference to remove the profit and just pass on the cost to participants.
- Include conference keynotes who matter, such as Bill and Melinda Gates, John Halamka, or Dr. Anthony Fauci, but no politicians and nobody who is selling a book.
- Offer educational events intertwined with the vendor booths in small presentation areas.
- Get hotels to participate and provide a reservation code, but allow participants to use whatever method they want to reserve rooms.
- Make the conference four days long and allow any member of HIMSS to attend for maybe $100-$200.
- Designate national and local non-profits to receive some of the proceeds, such as Doctors Without Borders, Red Cross, or groups providing healthcare for the homeless.
- The vendor community needs to take ownership and control of this event. If HIMSS is really about advocacy, let them prove it by focusing on that instead of marketing and event planning. We need change the paradigm and take control of what can be done versus just complaining about HIMSS.
HIStalk Announcements and Requests
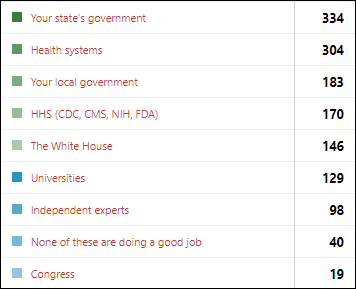
Poll respondents most often name state government and health systems as doing a good job with the COVID-19 outbreak, but federal government earns far fewer mentions and the White House’s actions polarize readers.
New poll to your right or here: for those working from home, what negative impact are you seeing?
I know COVID-19 is serious when Amazon tells me as a Prime member that my several items will take 3-4 weeks to arrive, which is probably longer than it took Sears to deliver catalog merchandise ordered on mailed order forms back in the 1960s.
The biggest worry I have about coronavirus is that frontline caregivers who are short on PPE, get little respect from their executive bosses, and expose their family members every day they come home from work will simply decide the job isn’t worth it and walk away. We can (eventually) figure out how to manufacture ventilators and lab tests, but they aren’t worth much without skilled, compassionate humans to operate them.
Webinars
April 15 (Wednesday) 1 ET: “Scaling front-line COVID-19 response: virtual education, screening, triage, and patient navigation.” Sponsor: Orbita. Presenters: Lawrence “Rusty” Hofman, MD, medical director of digital health, Stanford Health Care; Kristi Ebong, MPH, MBA, SVP of corporate strategy, Orbita. The presenters will describe how chatbots can be quickly deployed to streamline individual navigation to the appropriate resources, administer automated virtual health checks for monitoring and managing specific populations, increase access to screening and triage for high-risk populations across multiple channels (web, voice, SMS, and analog phone), and reach individuals in multiple languages.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Bright.md raises $8 million in a Series C funding round, increasing its total to $20.5 million. The company’s SmartExam automates 90% of a primary or urgent care visit in which patients answer clinical questions online and their information is assembled into a view that allows providers to complete their encounter asynchronously in less than two minutes. The company offers hospitals free use of its COVID-19 screening tool.
People

Cleveland Clinic promotes interim CIO Matthew Kull, MBA to the permanent job.
Announcements and Implementations

Cerner offers clients new COVID-19 services: remote two-way patient observation, telehealth, a 24/7 nurse line, remote patient monitoring, waived fees for increasing emergency bed capacity, a digital infrastructure for field hospital support, and temporary IT support help for health systems with resource shortages.
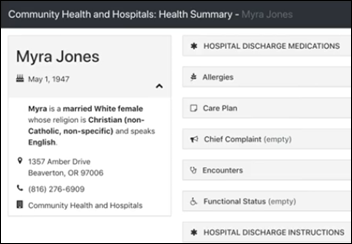
Kno2 offers free use of its patient record retrieval service to patient treatment organizations that don’t have a Carequality-connected EHR. The service requires only a browser and Internet connection to retrieve patient records in PDF and C-CDA formats or to send them to an EHR that supports Direct messaging.
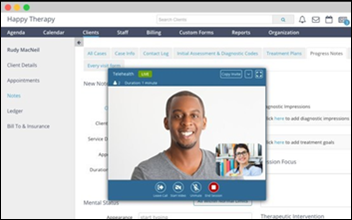
Mental health and behavioral practice software vendor Therapy Brands reports a one-week jump of 4,300% in virtual services as therapists move online for up to 100% of their sessions.
AMA adds new content for private practice physicians to its COVID-19 resource center: guidance for keeping practices in business, recommendations for managing non-urgent care services, and an update to its telemedicine guide.
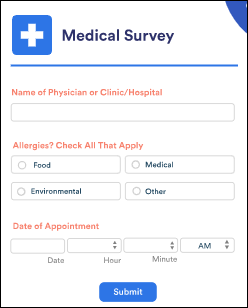
Online form vendor JotForm offers free accounts to coronavirus responders. The HIPAA-compliant online forms tool comes with a business associate agreement to allow collecting health information securely, obtaining patient signatures, sending files, and accepting payments. The regular subscription price is $29 to $79 per month.
MDmetrix offers hospitals a free subscription to its COVID-19 Mission Control, which uses a data extract to provide visibility into number of patients screened, ICU escalation, ventilator use, and demographic and medical profiles of patients who are in serious condition.
Government and Politics
CMS suspends its requirement that pathologists view slides from within CLIA-licensed facilities, opening the door to digital telepathology.
COVID-19

Abbott will start shipping a rapid detection COVID-19 test this week delivers positive results in five minutes and negative results in 13. The company says it can deliver 50,000 tests per day. The test runs on Abbott’s ID NOW platform.
Henry Schein announces GA of a rapid point-of-care COVID-19 antibody test that gives results in 15 minutes from a pinprick blood sample. The rapid immunochromatography IgM/IgG test does not require any instrumentation. The results can be used to guide therapy in later-stage infection as well as to clear those who were previously infected and may be immune.
Cardiologists report that patients who are later found to be infected with COVID-19 are reporting with cardiac rather than respiratory symptoms, with a new study finding that 20% of COVID-19 patients who were hospitalized in Wuhan, China had evidence of heart damage that quadrupled their death rate.
Johns Hopkins University launches a convalescent plasma study of using treating COVID-19 patients with blood plasma from donors who have recovered from it, a procedure that has shown promise in the small number of cases studied.
Ventilator experts in Southern California form the non-profit Co-Vents, which has mobilized a team and secured approved facilities to refurbish the estimated 20,000 warehoused ventilators that can be quickly returned to service. The founders have deep executive experience with Puritan-Bennett and other medical equipment vendors.
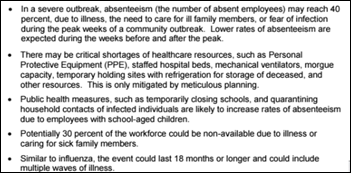
The VA’s coronavirus response plan predicts that staffing shortages may reach 40% at the peak of the outbreak. It warns that facilities may run short of PPE, beds, ventilators, and morgue space.
New York City’s 911 system is already overwhelmed with 7,000 COVID-19 medical distress calls each day, forcing first responders – who are sent out without adequate PPE — to make the call about who to transport to crowded EDs and who to leave at home on their own. Paramedics say that 911 calls mostly involved respiratory distress or fever three weeks ago, but now those patients who were sent home from hospitals are experiencing organ failure and cardiac arrest.
PeaceHealth St. Joseph Medical Center (WA) fires a contracted ED doctor who had worked there for 17 years after he refuses to take down social media pleas for protective gear. Interestingly in a “who’s the good guy if anyone” sort of way, the compassionate doctor works for private equity-owned TeamHealth and the firing came from a not-for-profit Catholic health system that has a half-dozen executives who make more than $1 million per year.
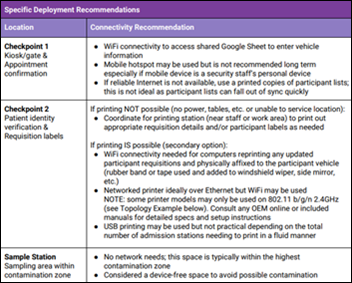
Verily’s Project Baseline issues a guidebook for running COVID-19 community-based testing sites under the a federally supported, state-directed program.

Decreasing case counts allow China to close the first inpatient ward of the two temporary hospitals that it built in Wuhan to handle COVID-19 cases.

The Army Corps of Engineers will turn Chicago’s McCormick Place convention center into a 3,000 bed COVID-19 hospital that will open by April 24.
The COVID-19 spending bill contains nearly $200 billion worth of hospital aid, to be administered by a small team at HHS that has experts worried about how efficiently and how equitably the taxpayer money will be handed out.
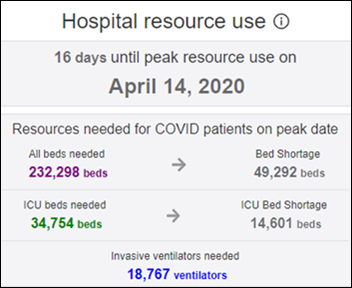
A University of Washington tool projects the COVID-19 peak for each state and predicts that the national peak for hospital resource use will be April 14, with a national shortage of 49,000 beds and 14,600 ICU beds. New York’s peak resource use is expected next week on April 6, when it is predicted to experience a shortage of 35,000 hospital beds and 7,000 ICU beds. The projection says the US will see a total of 81,000 COVID-19 deaths if social distancing is continued, with the first wave of the epidemic ending by early June. My question would be whether we can trust the data that is being recorded and submitted for public use, especially given inadequate testing and patients who convalesce or die outside of hospitals. I also note that beds and ventilators are not allocated among hospitals from a central pool – regardless of the total supply in a given area, your chances of living or dying are affected by what’s inside your hospital’s four walls.
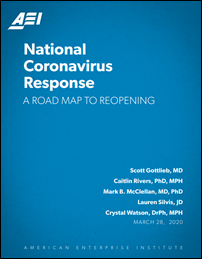
The American Enterprise Institute think tank and former FDA Commissioner Scott Gottlieb, MD lay out a detailed plan for getting the country through the COVID-19 pandemic:
- Phase I, where we are now, focuses on slowing the spread of coronavirus with school closings, working from home, and closing public spaces.
- State-by-state reopening happens in Phase II, allowing normal life to resume in a phased approach with some degree of social distancing, improved public hygiene, limiting public exposure of high-risk patients (including those over 60), sending sick people home as point-of-care diagnostics make widespread testing available. People will be asked to wear non-medical face masks to reduce their risk of asymptomatic spread.
- Phase III involves lifting distancing measures once broad surveillance is in place and COVID-19 drug treatments or a vaccine are developed.
- Phase IV is to make sure the US isn’t as unprepared for the next infectious disease threat as it was for this one.
Florida Governor Ron DeSantis bars a reporter from a state coronavirus update after she asks for social distancing at the briefings.
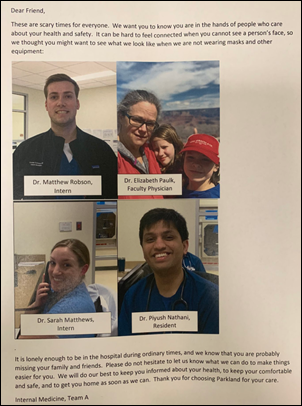
A hospital thoughtfully gives patients a handout that shows what their caregivers look like without their masks, reassuring them that they care about them even if their faces can’t show it.
Other
An article by family medicine doctor Megan Babb, DO says the COVID-19 pandemic is exposing the health system’s dirty secrets that lurk inside fancy buildings with state-of-the-art equipment. She concludes that non-doctors – healthcare administrators as profiteers or “wardens” — have controlled the healthcare narrative for too long and it is time for a takeover by “those who march in, not those who actively run out” during a crisis. She quotes anonymous doctors who report:
- Hospital executives ordering caregivers to remove their masks when seeing patients.
- A doctor who was placed on indefinite leave for complaining about a lack of instruction on how to separate infected and uninfected patients.
- Hospital executives telling an ICU doctor that they are too busy to create a policy of which patients will get ventilators if there’s a shortage.
- Hands-on clinical employees wondering why highly paid administrators aren’t missed when working from home.
- An administrative team with no clinician members who announced that they alone will decide who gets PPE.
- For-profit hospital administrators who said in January that money was too tight to buy PPE, but who were telling people to sell off stock because of what was coming.
- A hospital CEO who told surgeons that no matter what the Surgeon General recommends, elective surgeries are not to be rescheduled under penalty of termination.
- A doctor who overheard a hospital CFO telling the CEO that their bonuses would jump with higher COVID-19 insurance payments.
PatientKeeper VP Barry Gutillig found the 150 “Coronavirus Pandemic Kits” that the company had ordered for HIMSS20 and delivered the mask and sanitizer packages to Carney Hospital (MA), the country’s first dedicated COVID-19 care center.
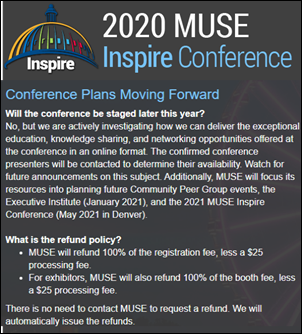
Medical Users Software Exchange cancels its 2020 MUSE Inspire Conference that was scheduled for May 26-29 at Maryland’s Gaylord National Resort & Conference Center, offering full refunds to attendees and exhibitors minus a $25 processing fee.
Several hospitals are laying off significant portions of their workforce – as much as 25% of their headcount – as their business declines while waiting for an expected COVID-19 surge.
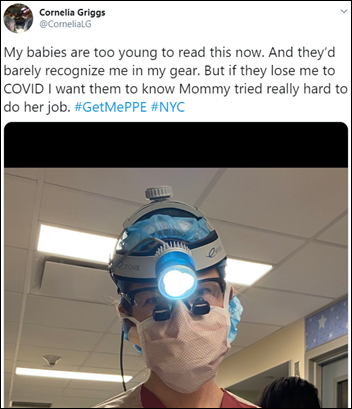
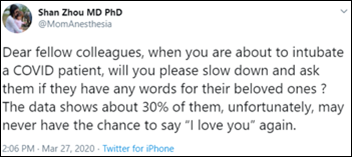
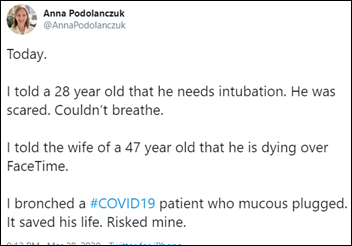
Sobering tweets.
Mirko and Valerio, 12-year-old twins from Sicily, entertain the world with some Coldplay during their quarantine.
Sponsor Updates
- CI Security adds a work-from-home security policy assessment to its managed services offering.
- GeekWire profiles the way in which University of Washington Medicine is using TransformativeMed’s Core Work Manager app to screen COVID-19 patients, monitor symptom checklists, track lab results and test status, and submit data to departments of health.
- CarePort Health launches the COVID-19 Transitions of Care Hub as an educational resource for care teams.
- Health Catalyst reports that multiple customer sites are already using its new COVID-19 solutions, and its open Data Operating System’s capabilities to meet evolving COVID-19 care demands.
- Spok offers its current customers free licenses for some of its solutions during the COVID-19 crisis.
- Redox releases its latest podcast, “COVID-19: Can Digital Health Help?”
- StayWell partners with the American Heart Association to release a new video, “Coronavirus: What heart and stroke patients need to know.”
- TriNetX prepares its Real-World Data Platform and global network of healthcare organizations to support COVID-19 clinical research.
- Vocera’s Smartbadge wins the silver 2020 Edison Award in the medical communications and connectivity category.
Blog Posts
- Risk Assessments Help Pre-Screen Home Care Patients for COVID-19 (Meditech)
- Navigating Uncertainty: CMS Signals that Value-Based Care is Here to Stay (Lightbeam Health Solutions)
- Tips on Quickly Implementing Telehealth in Your Physical Therapy Practice (MWTherapy)
- Why Data Interoperability is Critical in the Fight Against the Pandemic (NextGate)
- Asking the right questions to protect patient identities (Experian Health)
- How to More Effectively Communicate with Patients Who Self-Diagnose (PatientBond)
- Webinar Recap: Healthcare organizations discuss their use of telehealth and technology in the COVID-19 crisis (Nordic)
- Care Coordination for COVID-19 Patients (PatientPing)
- We’re Offering Complimentary Support to Clients for COVID-19 Best Practices (PerfectServe)
- Care Coordination Vendors Addressing Social Determinants of Health (Redox)
- Be Productive at Home During the COVID-19 Pandemic (ROI Healthcare Solutions)
- Managing a Suddenly Remote Staff (Summit Healthcare)
- Marketing During a Public Health Crisis – Touchpoint Podcast Feature (SymphonyRM)
- Let’s Talk About Visage’s COVID-19 Response (Visage Imaging)
- How One PT Clinic Adopted Telehealth in Response to COVID-19 (WebPT)
- Keeping up with COVID-19 (Wolters Kluwer Health Language)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



https://nypost.com/2020/03/28/mount-sinai-hospital-leaders-holed-up-in-florida-vacation-homes-during-coronavirus-crisis/
Amazing to see the sacrifice of countless people and companies in this very challenging time while the “leading” healthcare organization is silent and refuses to address the many disturbing comments about their outright thievery. Disgraceful is too kind a word. No self respecting organization should attend next years clown show in Las Vegas.