'Samantha Brown points out that, “Healthcare, like every other industry, gets caught up in the idolatry of the ‘innovators.’”' I…
EPtalk by Dr. Jayne 11/21/19
I wrote a few weeks ago about my adventures with flu vaccines and how the charges are handled by my insurance. Kaiser Health News dug into the phenomenon this week, going farther in noting the differences in costs among one payer’s own employees. The payments ranged from $32 in Washington, DC to $85 in Sacramento.
This illustrates the results of negotiations between payers and providers, the madness of which leads to the need for entire segments of the healthcare IT industry to keep up with it. Anyone who has worked with practice management or revenue cycle systems has experienced the phenomenon and the layers of code needed to wrangle it, and I salute you. It remains to be seen whether the government will be successful in forcing providers and payers to disclose this information publicly. Efforts to do so will likely be in the courts for some time.
I’ve been doing some behind-the-scenes work on clinical guidelines, and recently tried to track down data on a drug that is supposed to be available as a generic that we couldn’t find. The Wall Street Journal made note of the problem this week as well, observing that multiple factors keep those drugs from making their way into patients’ hands. It’s a disappointing phenomenon, but an interesting read.
In other drug news, a serious outbreak in pigs is likely to cause a shortage of the critically necessary blood-thinning drug heparin. African swine fever is on the march, killing nearly 25% of the world’s pig population, particularly in China, where the majority of heparin is produced. The World Health Organization is recommending that governments stockpile heparin, so be on the lookout for extra alerts and clinical decision support needs in EHRs.
Mr. H already reported on the AMA’s call for inclusive EHRs for transgender patients, but I want to throw in my two cents. Several years ago, I worked on some focus groups with a vendor who was trying to get this done. It can be complex, because there are many variables to document, including legal status, legal name, preferred name, surgical status, hormonal status, anatomical status, genetic status, etc. The vendor was focused and had several physician advocates who would continually explain to business analysts and developers why this was important. They ultimately they got the job done.
I’ve heard rumblings from other sources that this is a big lift for a small number of patients. But without the ability to document key clinical data and use it at the point of care, it results in a subpopulation being treated differently and in ways that might actually be counter to good clinical care.
The AMA also adopted a policy to promote education on health issues related to sexual orientation and gender identity for medical students and residents. I didn’t know much about the transgender population until medical school, where I had a professor who was public about their transition. It was a tremendous opportunity for learning and understanding and made a great impact on me, ultimately leading to me having a good number of transgender patients in my practice. I’m fully supportive of efforts to make EHRs inclusive for everyone, whether it’s based on differences in gender, age, race, ethnicity, or any other characteristic that may influence health. To be the most effective, we need to be able to meet our patients “where they are” and this is one way to work towards that goal.
Measure-palooza: The American Heart Association (AHA) and the American College of Cardiology (ACC) have released updated Clinical Performance and Quality Measures for adult patients with hypertension. The new report includes 22 new measures and expands focus from blood pressure measurement to care delivery systems and approaches. Their goal is to look beyond individual provider performance.
That’s great in theory, but it’s not how most other clinical quality measures programs work. It may also add workflows to EHRs, resulting in poor usability that will be blamed on the EHR rather than an explosion of guidelines and measures. There are also mismatches in the quality numbers used by AHA/ACC, CMS, and the National Committee for Quality Assurance. I’m sure EHR requirements writers are wringing their hands at this point. The report also includes a focus on digital health, including remote monitoring for hypertensive patients.
Maybe the EHR isn’t so bad: A recent study conducted at the University of Pennsylvania Health System showed an increase in orders for certain cancer screening tests when a “nudge” alerted users from the EHR. The alerts were targeted to medical assistants who created the orders for licensed clinicians to review and hopefully discuss with their patients. Despite the increased orders, there were not significant changes in the number of patients who completed the recommended screenings within a year-long time frame.
I recently worked with a practice that raffled off a big-screen television to patients who completed home colorectal cancer screening kits within a specified time frame. I’m not sure how legal it was, but it was certainly effective at motivating patients to submit a sample.
Kudos to the clinical informatics team at Oregon Health & Sciences University, who recently implemented a drug pricing comparison tool within Epic. It factors in data points such as co-pays, deductibles, and the need for prior authorization. The information has been available to dispensing pharmacists for a long time, but moving it to the point of care is key. It doesn’t matter how effective a drug is when it’s never going to be taken because the patient can’t afford it.
My clinical practice offers cash-only prescriptions at the point of care, which simplifies things for patients who know what their co-pays are (most of our drugs are either $15 or $30). However, many of our patients have no idea what their co-pay might be and are unable to make an informed decision. Having a tool like this at the bedside would be a benefit for the rare cases when we have to prescribe more costly drugs.
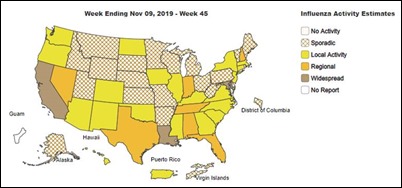
Flu season is getting well underway, particularly in the South. My practice is running low on vaccine and expects to be out by the end of the month. If you’re thinking about getting vaccinated but haven’t done it yet, time is of the essence. Three children have already died this season. If you still have plenty of vaccine, maybe an outreach campaign using those expensive population health tools is a good idea.

Email Dr. Jayne.



Re: Heparin and China.
Tip of the iceberg and a lot of the basic chemical precursors necessary for pharmaceutical manufacturing are also made today only in China.
A protracted conflict or even a scenario where there was a complete disconnect, however unlikely as it may seem right now, would mean shortages in a lot of controlled meds and other people medications people need daily to survive.