Hard agree, and not just because I'm a spreadsheet nerd. Why are we all here? Isn't it in the service…
EPtalk by Dr. Jayne 6/20/19
There is hope: The US House of Representatives voted last week to lift the ban that keeps the Department of Health and Human Services from funding efforts for a national patient identifier. The ban began in 1999 and blocks HHS from participating in private sector initiatives involving a unique identifier. HIMSS, CHIME, and other organizations have been lobbying for two decades to have the ban overturned in hopes of improved patient matching. The language was added as an amendment to the 2020 HHS appropriations bill and was introduced by both a Democrat and a Republican. Getting appropriations bills passed and signed into law can be tricky, so I won’t be holding my breath waiting for it to continue its journey on the hill.
Telehealth provider American Well has partnered with Cisco for a solution which enables virtual visits through television technology. Participating patients would use a set-top device that integrates with American Well. The solution is targeted to patients with chronic medical conditions as well as to older patients who might need regular visits. Many baby boomers are perfectly happy using smartphones and laptops and I’m not sure having one more device is necessary. People assume the older generations are “digitally dark,” but they are more savvy than you think. My own mother has a cooler, newer phone than I have. Years ago when I finally gave in to joining Facebook, the first friend suggestion I received was my then 87-year-old grandmother.
Lots of chatter in the physician lounge recently about media reports on the inclusion of “burnout” as a diagnosis in ICD-11. The World Health Organization says that media have it all wrong, that it hasn’t been recognized officially as a medical condition. ICD-11 includes burnout under “factors influencing health status or contact with health services” The chapter also includes indicators such as “contact with health services for reasons associated with reproduction” and “presence of device, implants, or grafts.” The American Psychiatric Association also states that burnout is not a medical diagnosis or a disease. Either way, being able to categorize burnout with a standardized code will allow for data gathering and better analytics. You can’t manage what you’re not measuring, but it will be a long time before we see ICD-11 in the US, so I’m not going to get too excited.
Speaking of mental health, clinicians in California are testing an app that tracks everything users do on their phones. The goal is to identify when a user is about to experience an emotional crisis. Various cities and counties are involved in the project, which is being tested on patients using the Los Angeles County public mental health network. It looks at historical use data to determine whether behaviors are changing and sends a message to the user. About half of initial pilot users dropped, citing technical issues or lack of interest. It’s an interesting concept, but one which would have to balance the loss of privacy with the potential benefit to users. For those with significant health conditions or risk for self-harm, it might be worth it, but for others it might be too invasive.
My practice has both x-ray and CT scan capabilities. Although the CTs are read immediately by a radiologist, we’re responsible for the primary reads on our plain films and often the radiology over-read doesn’t happen until our shift is over. Especially in that context, I’m excited about using AI to help interpret radiology studies, and frankly for some of our films, it can’t come fast enough. Although some films are grossly abnormal, other findings are subtle. Sometimes the quality of the studies is limited by the physical size and bulk of the patient. It would be great to have some support for those of us that are reading films in the field. Needless to say, I was excited to hear about the FDA approval of Zebra Medical Vision’s product that assists with CT studies that are looking for brain bleeds. The solution can reduce turnaround time, which is always good for the front lines. Zebra already has FDA approval for a chest x-ray product that specifically looks for pneumothorax. Maybe sometime before I retire I’ll have a virtual radiology assistant that pre-reads my films.
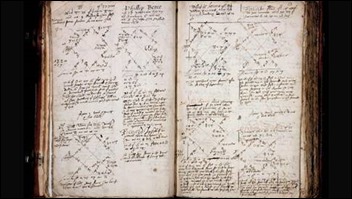
Like many of my peers, I enjoy learning about the history of medicine. I crossed an item off my bucket list a couple of years ago when I visited the Mutter Museum and admired Albert Einstein’s brain along with the Hyrtl Skull Collection. I’m also a fan of literature, so I couldn’t contain my excitement when I learned about a treasure trove of clinical notes from 400 years ago. The collection contains handwritten notes on more than 80,000 patients in early 17th-century England, kept by two healers who were known to cure their patients by using cues from astrology. The notes include treatments with tobacco and horse manure and cover conditions from depression to gonorrhea. Researchers at the University of Cambridge have put transcriptions of more than 500 cases online and its been great entertainment to learn about a patient whose “spleen was not sound,” as diagnosed by the presence of “black stuff that comes from by his excrements.” Another patient complained of “fretting & choleric & melancholy.” Other hot topics include childbirth, infertility, and witchcraft. My favorite treatment apparently involves avian slippers with “a pigon slitt & applied to the sole of each foote.”
Telehealth is officially the fastest growing place of service, growing 53% from 2016 to 2017 in comparison to 14% for urgent care centers and 7% for retail health clinics. Emergency departments experienced a 2% decline. This data comes from New York non-profit Fair Health, which hosts a claims database. Their annual white paper on place of service trends shows that organizations that are not thinking about how to incorporate telehealth might be missing out. Telehealth is still a small portion of all claims – 0.11% in 2017 data compared to 2.6% at emergency departments and 1.2% at urgent care clinics. This will only grow now that payment parity has arrived and telehealth or virtual visits are covered similarly to in-person visits.
I recently joined the ranks of telehealth providers and was surprised by how satisfying it can be. The patients are genuinely grateful that you’re there to take their call at 11 p.m. even if it just results in self-care recommendations. My previous proposal for being a dedicated after-hours telehealth provider for one of our local health systems was met with lack of interest and I still think they’re missing a major opportunity. I care for plenty of their patients in person at my urgent care, so we’ll have to see how long it takes for one of them to turn up in my online queue.
Have you ever used telehealth services for yourself or a loved one? Leave a comment or email me.

Email Dr. Jayne.



I haven’t had a telehealth appointment. I think that we’ve all been in video or conference calls in which the users can’t get it together. They are on mute or they can’t get their laptop microphone working or they can’t keep their phone an appropriate distance from their head or they type while talking or they can’t get their video to show up etc etc. I think the advantage of the TV top decide is that you can get your grandkid or the friendly girl that carried your groceries in to set it up once and then have it work until you get a new TV. It’s sort of the vcr player approach to telehealth.
Dr. J–
Your comment on radiology AI is a breath of reality in the AI buzz. In front line care, I don’t necessarily need an answer, but I do need a plan. An AI raising a question about something on a film can be enough. How many times do meat-based radiologists see something that “needs clinical correlation” to rule in or out something on a film? If questions remain, I can immobilize until a radiologist reading–or more likely follow-up–gives a best answer. Incidental findings are by definition not the problem of the moment, but it is much better to plan leave the patient with a plan to follow-up, rather than calling them back with an “oops.” The CFO’s eyes may be shining with thoughts of replacing radiologists, but the clinician who can make an expeditious plan is real value.
On your telemedicine foray, please update when you accumulate a run of data. My big hesitation: how much expectation is there for unnecessary prescribing (particularly of antibiotics) from patients, and more importantly, from management? In addtioin, the default to “now go have a ‘real’ visit,” while not new in retail/ urgent care, seems unsatisfying. Also curious how the telemedicine doctor is equipped to follow a case for a couple of days when needed, for clinical, liability and professional satisfaction purposes.
Keep up the good work,
rb