Hard agree, and not just because I'm a spreadsheet nerd. Why are we all here? Isn't it in the service…
News 3/8/19
Top News
Amazon, Berkshire Hathaway, and JPMorgan Chase decide to call their healthcare venture Haven.
The bare-bones website launched along with the brand is light on concrete details about the company’s plans, though visitors can glean a few details about its goals and structure if they dig deeply enough:
- Haven will focus on offering employees of the founding companies easier access to primary care, easier-to-understand health insurance, and affordable medications.
- It will use data and technology in unspecified ways to meet those goals.
- Haven seeks to become an ally of rather than a competitor to healthcare stakeholders.
- Profits will be reinvested.
- It may one day share its solutions with other interested parties.
Of its nine-member team, only CEO Atul Gawande, MD and Head of Communications Brooke Thurston have health system experience. CTO Serkan Kutan comes from Zocdoc, Head of Measurement Dana Safran from BCBS, and COO Jack Stoddard and Chief of Staff Megan McLean from Comcast.
Reader Comments
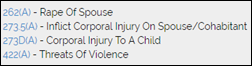
From La Vida Loca: “Re: [company CEO name omitted]. Have you seen his arrest record?If I were on the board, which he controls, I would be investigating moral turpitude as a cause. What does that do to the business?” I hadn’t heard that, but Googling turns up a September 2018 arrest and his co-founder wife has since left the company. I’m not naming him because I don’t see that he ever went to trial.
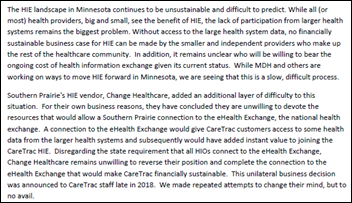
From Cranapple: “Re: CareTrac HIE. Reading between the lines, it is folding because the big Epic hospitals in Minnesota won’t share data.” The forwarded announcement from Southern Prairie Community Care says the HIE doesn’t have a business case because large health systems won’t share their data, adding that HIE’s technology vendor Change Healthcare won’t devote the resources to connecting the HIE to the EHealth Exchange (which the state requires of HIOs) that would have given the smaller players at least some big-hospital data.
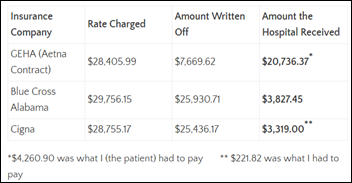
From Amy Gleason: “Re: healthcare costs. Check out what my daughter wrote about her monthly infusions. Her newest insurance pays $202K per year more than the last insurance. She is horrified and doesn’t understand why there isn’t an app that would help her.” First off, Amy has moved on from the shuttered CareSync and is now working for the White House’s US Digital Service on HHS/CMS interoperability projects. Her daughter Morgan’s write-up describes the situation – she gets the same infusion every month from the same doctor, same hospital, and same nurses, but the three insurers that have covered her have paid wildly different prices. Like normal humans, she’s wondering exactly how forcing hospitals to publish their chargemasters accomplishes anything when the healthcare world revolves around confidential discounting with each insurance company. I wish I had something encouraging to say, but Morgan has already wisely concluded that “I am thinking that we might really need to just burn the healthcare system to the ground and completely start over,” although I won’t burst her bubble by mentioning that fire trucks – in the form of politicians who are well paid by the profitable status quo – always manage to squelch those flames.
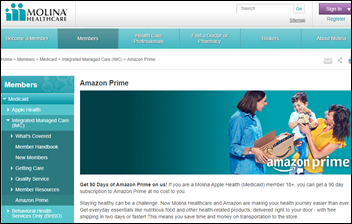
From Odd Bedfellows: “Re: Molina Healthcare. Offering its Washington State Medicaid members a free 90-day subscription to Amazon Prime.” There’s so much wrong here that I don’t know where to start, so I’ll save my snarkiness for this – even after the free subscription ends, the Medicaid members pay just $5.99 per month and that’s a lot less than I pay. You folks in Washington are generous to provide your less-fortunate neighbors with two-day delivery and Prime Video streaming while you’re off working. Still, I’ll table my cynicism temporarily in noting that for those who have transportation issues and who live in food desert neighborhoods, Prime could indirectly improve health and lower costs and I assume that Amazon is footing some or most of the cost in its attempt to get every American on Prime (and 100 million of us have already signed up).
HIStalk Announcements and Requests
Welcome to new HIStalk Platinum Sponsor Artifact Health. The Boulder, CO-based company made headlines this week for its just-announced work with AHIMA to deliver compliant physician query templates (documentation clarification) via its cloud-based platform. Health systems using Artifact reduced their AR days by increasing response rates to nearly 100 percent and reducing average response time by 80 percent. Doctors can respond from their computers or smartphones (often in just three taps) and appreciate receiving the same format for all queries (CDI, inpatient, outpatient, and pro fee). Their responses are recorded directly in Cerner, Epic, or Meditech to become part of the legal medical record with no manual recordkeeping by CDI specialists and coders. Thanks to Artifact Health for supporting HIStalk.

I decided to leave my HIMSS19 burner phone active for a bit longer, just in case you want to text me something interesting.
I’ve received a few reader inquiries lately about not getting my email updates because of spam-blocking or other email filtering on their end. Sign up again if you are among them – you only need to enter your email address and there’s no risk otherwise.
Webinars
March 27 (Wednesday) 2:00 ET. “Waiting on interoperability: What can payers and providers do to collaborate?” Sponsored by Casenet. Presenter: Amy Simpson, RN, director of clinical solutions, Casenet. A wealth of data exists to identify at-risk patients and to analyze populations, allowing every payer and provider to operate readmissions intervention and care management programs. Still, payer and provider care managers are challenged to coordinate and collaborate to improve outcomes because of the long road ahead to interoperability. Attend this webinar to learn what payers and providers can do now to share information and to coordinate their efforts to create the best healthcare journey for members and patients.
Previous webinars are on our YouTube channel. Contact Lorre for information.
Acquisitions, Funding, Business, and Stock
Long-term and post-acute care software vendor PointClickCare acquires LTPAC-focused medication management company QuickMar.

Chronic disease management-focused digital health company Livongo hires underwriters to prepare a Q3 IPO that’s expected to bring in $1 billion. The company has raised $240 million since former Allscripts CEO Glen Tullman started it in 2014.
Philips acquires Carestream Health’s imaging IT solutions business – which includes VNA, diagnostic and enterprise viewers, and clinical, operational, and analytics tools — for an unspecified amount.
People

Impact Advisors hires Jay Backstrom (Schumacher Clinical Partners) to lead its newly expanded telehealth consulting service.


Apixio hires Jennifer Pereur (Hill Physicians Medical Group) as VP of solutions and Terry Ward (Change Healthcare) as SVP of solutions.
Sales
- Allina Health (MN) selects patient engagement software from PatientWisdom.
- In Texas, Arise Austin Medical Center and The Hospital at Westlake Medical Center will adopt Allscripts Sunrise.
- The Escambia County Healthcare Authority in Alabama will implement Cerner Millenium at D.W. McMillan Memorial Hospital, Atmore Community Hospital, and four clinics. Atmore appears to be running Epic under Infirmary Health. The hospitals will also run Cerner RCM, ancillary, and ambulatory as well as outsource its business office to Cerner.
- The University of Kansas Health System chooses Connexient’s MediNav digital wayfinding software.
- WakeMed Health & Hospitals (NC) selects PeraHealth’s Rothman Index predictive analytics.
Government and Politics

VA officials tell members of a House appropriations committee that it will roll out its new Cerner EHR at three facilities in the Pacific Northwest early next year. John Windom, head of the VA’s EHR modernization effort, told lawmakers the pilot had been slowed down to give end users more training time. Also on the VA’s to-do list: finish converting VistA data into a Cerner-friendly format for migration, getting a permanent deputy secretary installed to oversee the roll out, and ensuring VA providers have security clearance to access DoD health records.
This op-ed lays part of the blame for the spectacular rise and self-destructive fall of Theranos at the feet of the US Patent and Trademark Office, which it says has done “a terrible job” of ensuring that whether inventions actually work. The office has admitted to operating on an honor code, a system that worked well for founder Elizabeth Holmes:
Yet more than a decade after Holmes’ first patent application, Theranos had still not managed to build a reliable blood-testing device. By then the USPTO had granted it hundreds of patents. Holmes had been constructing a fantasy world from the minute she started writing her first application, and the agency was perfectly happy to play along.
Privacy and Security
Northwestern Memorial Hospital fires dozens of employees for looking at the EHR records of actor Jussie Smollett, who was treated in its ED following his claim of being attacked in a racially motivated incident. One terminated nurse says that she and co-workers were fired for simply scrolling past the actor’s name on an EHR list while looking for other patients. The real crime in this story is that a grown man named Justin thinks Jussie sounds better.

Medical billing vendor Wolverine Solutions Group notifies hundreds of thousands of patients from an undisclosed number of providers and health plans of a ransomware attack that occurred last September. The company has been sending out notifications on a rolling basis since December, and expects to wrap up messaging by the end of this month, at which point it will have a better idea of how many people were affected.
Other

Auditors blame a 2017 implementation of Cerner’s billing system for the $38 million revenue loss of Glen Falls Hospital (NY), which was forced to lay off employees after losing 12 percent of its annual patient services revenue due to bills that went out late or were never sent.

A brilliant article in Science looks at how the public relations chief of the American Diabetes Association came up with the term “prediabetes” in trying to scare doctors and their patients to take action to address slightly elevated blood glucose levels, a mostly benign, symptom-free condition that had previously been labeled “impaired glucose tolerance.” ADA rolled out the term on a wide scale and keeps broadening the definition to include more people, now counting one in three Americans as being prediabetic even though studies show that only single-digit percentages of them will ever have diabetes. Since then, billions of dollars have been spent to address the observed blood glucose levels – mostly weight loss and exercise programs that have shown few results – and the now-medicalized “condition” has created a cottage industry of fitness coaches, dietary products, glucose monitors, and prescription drugs that now consume at least $44 billion of US healthcare spending each year and line the coffers of the ADA with up to $27 million annually in drug company contributions. A researcher who advocates wider use of prescription drugs to treat prediabetes has earned $5 million from the companies that sell those drugs and many doctors who wrote the ADA’s standards of care have also made millions. A Mayo diabetes clinician concludes, “The people who lose are the people who go from being a healthy person to being a patient. Now, they have the sick role. They have to go for checkups and tests and treatments … I just don’t think we [prevent diabetes] by making every healthy person a patient.” @EricTopol lauded the article, calling prediabetes “mass, dumbed, down medicine and scaremongering one of three (84 million) adults and 1 billion people worldwide, supported by pharma, propelled by guidelines from trusted organizations … with 80 percent of such individuals at no risk.”

Dear HIMSS Media, I’m confused – is this event in Santa Clara or LA?
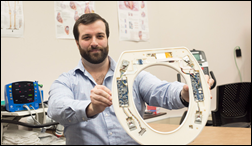
In an attempt to prevent hospital readmissions, researchers at the Rochester Institute of Technology in New York develop a sensor-embedded toilet seat they say can detect deteriorating conditions in congestive heart failure patients.
Sponsor Updates
- PMC Regional Hospital (IN) completes its Meditech Expand implementation with help from Engage Consulting.
- EClinicalWorks will exhibit at the AAPM Annual Meeting March 7-9 in Denver.
- Ellkay will exhibit at the ACMG Annual Clinical Genetics Meeting April 2-6 in Seattle.
- EPSi will exhibit at the Metro New York HFMA Chapter’s Joseph A. Levi 60th Annual Institute March 7-8 in Uniondale.
- Healthfinch publishes the third e-book in its refill optimization series, “Achieving Refill Protocol Consensus.”
- Huntzinger achieves a score of 96.4 in the HIT Advisory Services Category of the “Best in KLAS Software & Services 2019” report.
- Hyland releases a new enterprise search solution as part of OnBase content management platform.
- Imprivata will exhibit at SoCal HIMSS March 12 in Duarte.
- Mobile Heartbeat invites vendors with complementary solutions to integrate with its CURE Connect API Suite via its new CURE Connect Interoperability Program.
- NPR profiles Kentucky Hospital Association, Kentucky Office of Rural Health, and Collective Medical efforts to develop a statewide care coordination network.
- Apixio announces that it has grown its customer base to 36 health plans and provider groups, and has analyzed 11 million documents for Medicare Advantage and private plan beneficiaries.
- Netsmart earns multiple top Black Book awards across behavioral health and post-acute healthcare settings.
- Sansoro Health makes available a cloud-hosted test environment for digital health companies and health IT developers to test application workflows in a real EHR environment.
- PatientPing announces that its national network of ACOs generated over $100 million in shared savings for 2017 under the CMMI Next Generation ACO Program.
Blog Posts
- Enhancing the Patient Experience from Start to Finish (Formativ Health)
- How taking my pup to the vet is like an IT solution health check (Hyland)
- Interoperability and Information Blocking Proposed Rules from CMS & ONC (Impact Advisors)
- Balance for Better: Women in Health IT Talk Success and Inspiration (InterSystems)
- 4 common pitfalls to avoid during your EHR implementation [Executive Summary] (Nordic)
- Taking a Consumer-Centric Approach to Access: Insights from Banner Health (Kyruus)
- International Women’s Day 2019 (Optimum Healthcare IT)
- Sometimes When Things Don’t Go As Planned, It Might Be For The Best (PMD)
- 4 common pitfalls to avoid during your EHR implementation [Executive Summary] (Nordic)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates. Send news or rumors.
Contact us.








“Still, payer and provider care managers are challenged to coordinate and collaborate to improve outcomes because of the long road ahead to interoperability.”
There is no long road to interoperability. There are data solutions right now that can curate and harmonize all the data that’s out there. FHIR is not going to be a magic bullet either. Healthcare organizations have to stop waiting for Judy to figure it out and invest in an enterprise data strategy and platform.
Why should healthcare organizations want to invest in such a thing? I suspect many of them have left out a key motivation from their mission statements.