Giving a patient medications in the ER, having them pop positive on a test, and then withholding further medications because…
News 2/18/15
Top News

A Wall Street Journal editorial by Phoenix surgeon Jeffrey Singer, MD — mostly known for his ongoing anti-Obamacare rants via the libertarian Cato Institute — says doctors like himself were forced to implement EHRs, adding that he’s an “unwilling participant” (meaning he would rather ruin his practice by using an EHR than take a 1 percent Medicare pay cut, which sounds to me like a voluntary business decision rather than conscription). He blames EHRs for lowering the quality of care and increasing costs, the former because he has to look away from the patient to see the screen. He misfires in urging that the Republican Party end the EHR program started by Democrats, possibly forgetting that it was Republican President George W. Bush who in 2004 said that every American should have an electronic medical record within 10 years and who created ONC to make it happen. President Obama had been in office only a few days when he signed ARRA in February 2009 and the Affordable Care Act had nothing to do with EHRs.
HIStalk Announcements and Requests

It’s your last chance to tell me “I want to come” to HIStalkapalooza. Frontline providers get priority and I’d like to see a lot of them at the event. Meanwhile, I appreciate the support of the HIStalkapalooza sponsors who are cool enough to be willing to pay for a fun evening for non-prospects (and in fact, even the employees of competitors) in accepting the cross-section of HIStalk readership that attends.
Gold Sponsors
Webinars
March 5 (Thursday) 2:00 ET. “Care Team Coordination: How People, Process, and Technology Impact Patient Transitions.” Sponsored by Zynx Health. Presenters: Grant Campbell, MSN, RN, senior director of nursing strategy and informatics, Zynx Health; Siva Subramanian, PhD, senior VP of mobile products, Zynx Health. This webinar will explore the ways in which people, process, and technology influence patient care and how organizations can optimize these areas to enhance communication, increase operational efficiency, and improve care coordination across the continuum.
The recording of John Gomez’s well-attended webinar, “Inside Anthem: Dissecting the Breach” is available above or here. I received quite a few emails from attendees who enjoyed his presentation even though it’s obviously not the cheeriest topic on the IT agenda.
Acquisitions, Funding, Business, and Stock

MedAssets announces Q4 results: revenue up 16 percent, adjusted EPS $0.39 vs. $0.30. The company wrote off $52.5 million worth of goodwill in its revenue cycle services business due to growth that mostly came from low-margin business. Above is the one-year share price chart of MDAS (blue, down 5.6 percent) vs. the Nasdaq (red, up 15.3 percent).


MedAssets announces that board member Halsey Wise (Lime Barrel Advisors, left)) will replace John Bardis as chairman and CEO, effective immediately. Wise joined the board less than a year ago.
Sales
Greenway Health chooses Orion Health’s Rhapsody Integration Engine for financial transaction processing.
People

Bradley Cordes (Accretive Health) joins T-System as VP/GM of the company’s charge capture and coding business.

McKesson hires Bansi Nagji (Deloitte) as EVP of corporate strategy and business development.
Announcements and Implementations
HCS adds barcode charge capture to Interactant Charge Management.
Imprivata announces that its new Confirm ID product has been integrated with Symantec’s security offerings to meet the DEA’s identity-proofing requirements for electronic prescribing of controlled substances.
Surescripts creates a step-by-step video guide and tools to help health systems and practices meet New York’s I-STOP mandatory e-prescribing law.
Several health-related features didn’t make the cut for the initial Apple Watch release because they didn’t work, were too complex, or would have triggered FDA’s interest. The watch won’t be able to run an EKG, measure blood pressure, or capture blood oxygen.
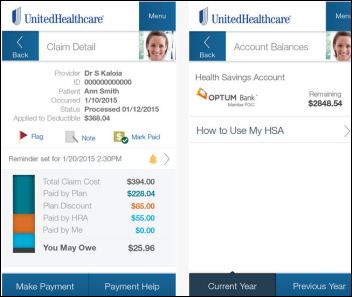
UnitedHealthcare enhances its mobile patient app to allow members to pay their medical bills online, track their Fitbit activity, and stream the company’s video channel.
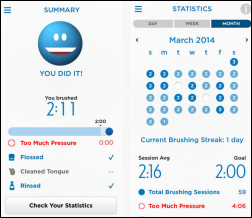
New to the Internet of Pointless Things: a Bluetooth-connected electric toothbrush that not only eliminates the tedious back-and-forth arm movement that almost involves actual exercise, but also gives “real-time information about brushing modes, times, and areas.” One can only imagine what personal health and hygiene devices the “solution looking for a problem” techies will connect to next. I fear toothbrush terrorism in which devious hackers breach Oral-B’s site and send thousands of Bluetooth-connected toothbrushes into enamel-damaging hyperdrive. Or that dental insurance companies will buy toothbrushing Big Data to cancel policies for infrequent brushers and flossers.
Sony one-ups Google Glass by developing an even dorkier-looking, puck-powered virtual reality headset called SmartEyeglass, now available in a developer’s edition with a planned March GA. It will allow users to use Facebook and Twitter, the need for that functionality in itself being quite disturbing.
Other
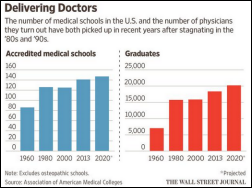
The Wall Street Journal describes changes being made to the outdated curricula of US medical schools. One school starts new students by putting them through an eight-week emergency medical technician program, while another requires the first-years to work as patient navigators. A required New York University School of Medicine course assigns students to analyze a database of hospital encounters to discuss the wide variation in cost. Mayo’s new Arizona medical school will offer lectures in electronic form so that class time can be dedicated to discussion and case studies and will offer a course called Checkbook in which students track all services performed on their assigned patients to identify possible waste. Mayo students also shadow non-physician employees and manage panels of patients as care coordinators. That’s interesting, but it would also be relevant to review how residencies are managed as hospitals get CMS-paid cheap medical labor that adds several more years to their education and forms nearly all of the habits (good and bad) that will persist through each physician’s medical career.

Computers at Australia’s Fiona Stanley Hospital go down for 14 hours when lightning strikes a Fujitsu-owned data center.

St. Joseph’s Hospital Health Center (NY), which lost nearly $22 million in 2014 mostly due to one-time Epic implementation costs, will join an unnamed health system (most likely Trinity Health).
A study of inpatient satisfaction following construction of an expensive new hospital wing at Johns Hopkins featuring healing gardens, soaring lobbies, extensive artwork, and patient rooms equipped with an interactive TV system and “quiet” features finds that while patients understandably scored the new facilities higher, those amenities didn’t raise the physician evaluation component of HCAHPS. In other words, the doctors didn’t enjoy the halo effect of practicing in fancier surroundings.
A former Duke University football lineman co-founds Logistical Athletic Solutions, which allows athletes and staff to exchange messages, manage schedules, and track medical records. A Duke study found that the system saved the university $244,000 in six months by reducing material costs and data entry hours.
An attorney-authored Medscape article suggesting that doctors allow their patients to make audio or video recordings of their encounters is met with a host of negative comments from physicians, some suggesting that patients don’t need anything more than the EHR-generated visit summary and those patients wanting to record their visits are likely to sue. The author says, however, that only a handful of states require both parties to consent that their conversation be recorded – no matter how the recording is made, it’s a legal record.
I’m not sure I want these guys writing about medical apps – their attention to detail is pretty much a waist.
Hospitals in St. Louis are using their EHR information to remind parents that their children should be given measles vaccine.
A doctor in Canada sets a five-minute timer at the beginning of a patient visit with the encouragement of a militant doctor’s advocacy group. He doesn’t stop the conversation at five minutes, but points out to each patient when it rings that Ontario’s government pays him for only that time. He declined to explain how he came up with the five-minute number except to say represents an hourly rate similar to that of dentists and lawyers.
An article in The Atlantic says that tweeting is a waste of time for companies and online publications whose goal is to send traffic to their websites. Instead, short attention span readers skim Twitter’s frothy observations (sometimes tweeted by people who barely read the original article themselves) as standalone material, generating revenue and traffic only for Twitter. As Bill Murray (aka Nick Ocean) says, “Twitter is basically just you having a conversation with yourself hoping that someone else will join in.”
Sponsor Updates
- The Advisory Board Company adds Zynx Health’s heart failure intervention checklist to its online heart failure toolkit.
- ZeOmega posts “The Key to Delivering Healthier Babies.”
- Life Monitor Pty Ltd. will sell AirStrip’s solutions in Australia and New Zealand.
- Rockdale Medical Center (GA) replaces pre-printed forms with electronic versions from Access.
- Impact Advisors publishes a white paper titled ONC Nationwide Interoperability Roadmap: Driver’s Handbook.”
- Practice Fusion integrates medication electronic prior authorization from CoverMyMeds with its EHR.
- PerfectServe President and CEO Terry Edwards posts “The Consumerization of Healthcare: Can Providers Keep Pace?”
- Navicure ended 2014 with $74 million in revenue,, a 96 percent customer retention rate, and a top three clearinghouse ranking by KLAS.
- TeleTracking Technologies joins the NPSF Patient Safety Coalition.
- Anthelio, Certify Data Systems, and Aventura will exhibit at the Texas Regional HIMSS Conference February 18-20 in Austin.
- Caradigm writes about “The Population Health Marathon.”
- ClinicalArchitecture offers the fourth installment of its blog series on “The Road to Precision Medicine.”
- CareTech will exhibit at the Center for Healthcare Governance Winter Symposium February 22-25 in Michigan.
- ADP AdvancedMD offers a guide to “The Top 5 Technologies in Healthcare for 2015 and Beyond.”
- Besler Consulting publishes an e-book focused on readmission reduction strategies.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.
















Feeling a little cynical today Tim? Don’t you worry, I share many of your beliefs with regards to IoT. A lot of crapola being thrown out there on the market, reminds me quite a bit of the dot com days of yore.
Au contraire, the ACA had all to do w EHRs, or vice versa.
Obama needed the (exagerated) savings supposedly from the efficiencies of EHRs to help pay for ACA in response to queries from Congress and the CBO. Recall the RAND study commissioned by the vendors?
He did not fathom upcoding, slower workflow, and the litany of problems that surfaced after widespread use.
Why are you trying to denigrate Dr Singer by using language like: “known for his ongoing anti-Obamacare rants” rather than addressing the points of his article.
I think you may want to check your own facts. While the “Republicans” under George Bush wished to see every American with an electronic medical record, it was President Obama who signed HITECH into law on Feb. 17, 2009, as part of the American Recovery and Reinvestment Act of 2009 (ARRA) economic stimulus bill, that provided the EMR subsidies for meaningful use (MU). It was the current president who essentially mandated EMR use via MU.
Excuse me, but why the heck is the healthcare industry so populated by dinosaurs tat anyone had to mandate EHRs?
Cry me a river Dr. Singer. My guess is he doesn’t know how to efficiently use whatever EMR he has. Either that or he’s on athenahealth or Cerner.
Current EMR systems are inefficient, have lousy user interfaces and do not really address the needs of physicians. It’s well known that healthcare. IT lags far behind the ease of use of consumer apps. Why is this the case? You’d like to blame the doctors I’m sure, but it’s because EMRs have not been allowed to evolve through the natural cycle of competitive innovation as in the consumer space. The vast maze of regulatory constraints (MU etc) has stifled innovation and is destroying competition. In the end, we’ll be left with just a handful of large EMR vendors, such as Epic.
I would suggest that Docinfo and Keith McItkin check their “facts”. The Affordable Care Act (ACA or “Obamacare”) had nothing to do with EHRs or Meaningful Use, which is exactly what was originally said. The incentives for Meaningful Use come from the American Recovery and Reinvestment Act (ARRA). In 2004, George W. Bush set a goal for every American to have an electronic medical record within ten years. The ONC, along with other organizations, was tasked with setting priorities and creating policies to achieve that goal. It would be a very hard goal to achieve without “mandating” the use of such EMRs, and it is unfortunate that such a “mandate” was necessary to incentivize the healthcare industry to jump into the 20th century and use electronic medical records. Instead of whining and erroneously blaming Obama for making him use EHRs, Dr. Singer could opt for the financial penalty instead. Or, he could make better use of his time by working with his EHR vendor to improve upon the product that he claims is ruining his practice. But, I suppose that wouldn’t get printed in the WSJ. I don’t think Dr. Singer was “denigrated” by pointing out that he has a history of anti-Obamacare rants – it is useful to know existing bias when considering whether his latest rant holds any merit.