Neither of those sound like good news for Oracle Health. After the lofty proclamations of the last couple years. still…
News 11/21/14
Top News
Emdeon will acquire Change Healthcare for $135 million. The company offers consumer messaging, lookup, and education tools to improve engagement.
Reader Comments
From Former McKesson: “Re: McKesson reorg. McKesson Technology Solutions has another big reorg, the third in three years, this time in the MCCA business unit. MTS has lots three good GMs in the past 12 months and middle managers are fleeing.” Unverified. An attached internal email from Jeff Felton, president of McKesson Connected Care and Analytics, says that several RelayHealth business lines have been combined into McKesson Connectivity & Analytics under Ken Tarkoff and that several reporting changes have been made.
From Judge Smails: “Re: country club brawl, with a healthcare IT twist.” Police responding to a 911 call break up a fistfight at the tony Boston-area Weston Golf Club, started when the club’s president ordered jeans-wearing guests to leave the premises because of their dress code violations. The club president who apologized and then resigned was Tom Ferry, president and CEO of hospital software vendor Curaspan. I interviewed him a couple of years ago. I’m siding with him: people everywhere (restaurants, cruises, meetings, etc.) are offended at the idea that clearly stated dress-related rules might inconveniently apply to them and being loudly obnoxious usually gets them a quiet exemption.

From Mike Kovner: “Re: Medicare ACO Shared Savings Program results. CMS has posted the Performance Year 1 final financial reconciliation and quality performance results for all MSSP ACOs with 2012 and 2013 agreement start dates. Kudos to the 52 ACOs that produced real savings and met the threshold for clinical quality measures. Memorial Herman ACO was the big winner with a $28M earned Shared Savings payment, followed by Palm Beach ACO with $19M. Tough break for the six ACOs that produced savings but did not meet the quality threshold, leaving real money on the table.” Mike sent over a detailed worksheet that I’m sure he would be willing to share.
From Ohio MD: “Re: ICD-10. We’re a busy orthopaedic EP. Both 5010 claims and HCFA 1500 can handle both code sets, so why not allow a phase-in over several years? There’s no way to do end-to-end testing since you can send a claim to CMS, but you don’t get payment, and no other payers allow testing as far as I know. Plus getting signed up for CMS testing is an absolute nightmare, especially for small providers.” Readers are welcome to weigh in: is a hard compliance date for ICD-10 necessary? CMS has had plenty of time to prepare with the one-year delay, so why can’t it start accepting either version now?
From Sinking Ship: “Re: [consulting firm name omitted]. Earlier this week rumors were spreading that the company has over 50 percent of its consulting staff on the bench due to poor performance by the sales teams.” Unverified and likely not possible to verify, so I left the large company’s name out. Maybe the sales team is underperforming, but I believe we may be seeing a downturn in the healthcare IT consulting business in general due to fewer go-lives and government meddling with ICD-10 dates and Meaningful Use tweaks. That could be my own incorrect perception from talking to a couple of folks. If you’re on the front lines, tell me what you think.
HIStalk Announcements and Requests
This week on HIStalk Practice: Greenway, CVS, and Quirk open new facilities. CMS Compare websites come under GAO’s fire. Pediatrician Sapna Mukherjee, MD discusses her use of HIT at her concierge practice. Healthcare.gov sees fewer glitches than several state-run exchanges. Seacoast Orthopedics & Sports Medicine physicians achieve MUS2. ONC welcomes several new staff members. Thanks for reading.
This week on HIStalk Connect: Harvard public health researchers launch a heart health calculator that evaluates lifestyle choices rather than blood pressure and cholesterol levels. Walgreens rolls out on demand lab tests across its 8,200 facilities. Cue, a digital health startup making smartphone-based lab analyzers, raises a $7.5 million Series A.
Acquisitions, Funding, Business, and Stock

Valence Health receives a $15 million growth equity investment, raising its total to $45 million.
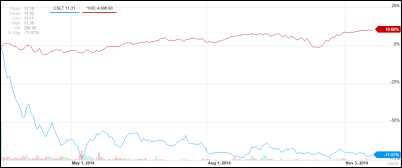
A questionable Fortune article called “Digital healthcare investments soaring again. Here’s why.” spends most of its pointless meandering talking up Castlight Health, which is hardly the poster child for why digital investments should be soaring. All of those sharp investors who jumped all over Castlight right after “the most overpriced IPO of the century” have seen their investments shed 72 percent of their value in just seven months (blue) vs. the Nasdaq’s gain of nearly 11 percent (red) over the same period as the company continues to lose big money. Castlight is still mysteriously worth $1 billion, or 28 times annual sales.
Sales
Providence Health & Services chooses NantHealth’s Clinical Operating System and eviti|Advisor for genomic analysis and evidence-based cancer treatments.
Providence Anesthesiology Associates (NC) chooses TigerText secure messaging.

WellSpan Health (PA) selects the Visage 7 Enterprise Imaging Platform.
People


EHR scribe provider Essia Health names Anita Pramoda (TangramCare) to its board and William Moore (4medica) as CFO.

Dave Morgan (Vista Consulting Group) joins Greenway Health as CFO. He apparently replaces Laurens Albada, but I’m not quite sure since the company’s leadership page lists Morgan but Albada still has a leadership profile that lists him as CFO. I haven’t seen any announcements either way, so I’m going with Dave.
Announcements and Implementations

CommonWell Health Alliance announces (in a poorly written press release that makes it impossible to figure out what they’re actually announcing) that is offering its services to a broader market, that RelayHealth is its technology provider, and that Aprima and CareCloud have signed up as members.

Greenway Health will open a technology development center in Cobb County, GA in early 2015 that will create 150 jobs.
Revenue cycle and coding products vendor VitalWare launches VitalABN, a medical necessity validation tool that automates the Advance Beneficiary Notice of Noncoverage process.
MModal announces that its Fluency for Image Reporting can notify radiologists of documentation deficiencies in real time.

Johns Hopkins Medicine and Premier will collaborate on educational, clinical, and analytics projects.
A Salesforce blog post suggests that its rumored healthcare push is underway as it describes how Johns Hopkins Healthcare is using the company’s platform in an engagement program to keep high-risk patients out of the ED and to coordinate the schedules of home care workers.
GE Healthcare, a 50-50 joint venture partner in Caradigm along with Microsoft, will resell Caradigm’s single sign-on and context management solutions to integrate anatomic pathology information systems.
Merge Healthcare launches Merge One, a cloud-based, transaction-priced solution for ambulatory radiology sites that includes PACS, RIS, financials, universal viewer, cloud archive, document management, and analytics.
Government and Politics
Newly discovered emails from former CMS COO Michelle Snyder say her boss, CMS Administrator Marilyn Tavenner, used threats and tantrums to insist that Healthcare.gov be launched on time no matter what. Snyder retired weeks after the failed launch. Meanwhile, the House Committee on Science, Space, and Technology gets its subpoena-powered audience with former US CTO Todd Park on Healthcare.gov. Republican members hammered away, while the ranking Democrat member apologized to Park for making him a target for Affordable Care Act venting and said it will make it harder for Park to carry out his current job of recruiting wealthy technical entrepreneurs to federal government work once they see how he was treated.
The GAO says the consumer transparency tools created by CMS aren’t user friendly and fall short on cost and quality information. HHS agrees.
Another GAO report finds that the VA violates its own policy in failing to push out critical OS patches to desktops and laptops within 30 days.

CMS forms the Office of Enterprise Data and Analytics and names Niall Brennan as its chief data officer.
HHS’s OIG lists the agency’s top challenges for FY 2014, one of which calls for HHS to make sure that Meaningful Use policies align with its goals and reflect “the changing health IT landscape,” adding that HHS should provide guidance on adoption, Meaningful Use, and interoperability and that HHS, CMS, and ONC stay focused on privacy, security, and fraud prevention.
Vermont cuts ties with economist Jonathan Gruber over his unflattering comments about lack of transparency in passing the Affordable Care Act. The state is ending Gruber’s economic modeling contract in which he bills his time at $500 per hour and that of programmers at $100 per hour. He and his associates collected more than $6 million in federal and state grants and contracts and he’s still working on an NIH project that will pay him $2 million.
Innovation and Research
Two University of Windsor researchers say their newly patented predictive software can monitor EEG waveforms and give someone with epilepsy a 17-minute advance warning that they’re about to have a seizure, although they studied only 21 patients. They also recognize that while it would be nice to let an epileptic know they need to pull their car over or surf one last wave before hitting the beach, it won’t do much good unless someone develops a portable, continuous EEG monitor (waterproof, in my second example).




Finalists in Harvard’s Health Acceleration Challenge are Twine Health (personalized treatment plans), Boston Children’s Hospital’s I-PASS (care team communication), Bloodbuy (a Priceline-like bidding system for hospitals to buy blood products), and Medalogix (predictive identification of patients as candidates for palliative care).
Technology

The city of Cleveland will reportedly announce Friday that the Euclid Avenue area, home to several health-related organizations and vendors and locally branded the “Health-Tech Corridor,” will get 100-gigabit fiber optic broadband connectivity courtesy of a federal grant that will pay for it.
Apple publishes WatchKit tools and guidelines to help developers move their iPhone apps to Apple Watch.

A Santa Barbara, CA group that treats homeless people from temporary clinics it sets up in public parks uses a self-developed mobile EMR running Microsoft Access on $200 Chromebooks and a Wi-Fi hotspot. Its author says, “I do not have nearly as many coding options to control both the styling and the function as I would if I had coded the platform from scratch. What we gained was security, instant accessibility of all past charts for a patient, legibility, more detailed records, more accurate reporting, and much more.”
Other

Botsford Hospital (MI), which recently merged with Beaumont Health System and Oakwood Healthcare to create $3.8 billion system, will replace McKesson Paragon with Epic, which is used by the other members of the new system.
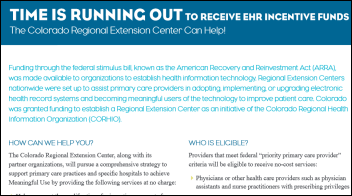
Colorado RHIO announces that its Regional Extension Center will no longer offer free services now that its ONC grant has run out. The REC will be replaced with a fee-based services division. I would opine that dwindling Meaningful Use activity makes it even more unlikely (if that’s possible) that providers will spend their own money on its services.
A Truven Health Analytics-NPR poll finds that 75 percent of Americans see an EHR-using doctor, 68 percent are OK with having their de-identified health information shared with researchers, but only 22 percent would let their doctor or insurance company review their credit card transactions or social media information even if it might improve their health. More than half the respondents claim they have reviewed their information as kept by their provider.
EClinicalWorks CEO Girish Navani writes an Entrepreneur article called “The Case for Never Selling Your Company,” saying that eCW “is, and always will be, a privately-held company. I have no interest in selling it, regardless of any offer I may get. In addition, we don’t use investor cash or spend money we don’t have.” He says selling a company often changes its founding principles, threatens its longevity, and takes away the independence of its leaders.
Sponsor Updates

- Wellcentive SVP Mason Beard and CTO Kirk Elder accepted a finalist plaque for the Intel Innovation Award at the 2014 Health IT Leadership Summit in Atlanta on Thursday.
- T-System is providing free flu T Sheets that include the latest CDC guidelines to all providers
- NextGen Healthcare earns top ranking among healthcare IT vendors providing outsourced billing / RCM.
EPtalk by Dr. Jayne
I received a fair amount of reader feedback about this week’s Curbside Consult on proposed measures for Meaningful Use Stage 3.
From Ski Dude: “I enjoyed your article on MU Stage 3. Ever so true, as an IT consultant and patient I find the overly inquisitive requirements to be a burden. I have a customer, a primary care physician group with approximately 120 providers, that has a spread sheet for all the metrics they need to capture and for whom they have to report them. It is a 17 x 160 cell grid. I’m sure it’s costing these providers way more than they’ll gain in incentives or lose in reimbursements just trying to collect all the data and deliver it to the 17 data consumers.” I’m right there with you on that. Back before MU, we had approximately 20 metrics that we were tracking for providers as part of our internal Clinical Score Card. Every one of them was evidence-based and had a direct impact on patients: influenza vaccination, colorectal cancer screening, diabetes screening / glucose control / foot exams, etc. that had a real return on investment, either financial or in reduced patient morbidity and mortality.
Now we’re tracking hundreds of measures, some of which have not been directly proven to benefit patients. I wonder what our Institutional Review Board would think about the fact that our entire patient population (not to mention all of our staff) is part of an unapproved research project involving human subjects?
I’ve been asked to judge a local science fair this year. Looking at the packet of rules and regulations, what MU is doing to the healthcare community wouldn’t even pass muster for the seventh grade.
I received a couple of replies that surprised me, generally stating that the proposed measures didn’t go far enough to allow providers to make significant advances in MU3. Various suggestions included: tying the payments to actual data scores (not merely reporting the data); requiring HIE exchange on each and every patient visit; and requiring interfaces with data reported by patient mobile devices and apps.
If MU wasn’t already on its deathbed, I’m sure including those factors will push it into full arrest. It’s not that many of us disagree with these ideas, but including them in MU3 without significant financial support and adequate time to plan, code, test, and implement the features just makes them untenable. Not to mention that there is little evidence that wholesale implementation of these features (especially if it’s at the expense of tried and true population health work) may not have significant demonstrable benefit.
I also received one comment that made me smile.
From Thoughtful, Albeit Weird: “Great Column on MU3. It made me think of this: When you brought your car in for repairs, you would have to provide information to the counter person on how you had driven your car and when. What about the other cars in the house? Did you have an accident in the past couple of years? Parking or speeding tickets? What kind of gas do you use? When your mechanic is working on your car, would they have to check the brake, power steering, coolant, and other fluids and document the findings? Tire pressure? Document the state of the belts and hoses? What was the brand of brake shoes they installed? Why did they use that brand and not a different one? When they replaced the brake fluid, did they document that the old fluid was properly drained and that no water was in the line? Did they scan the brake fluid they installed? Did the software automatically check it was of the approved type for the car? If they did have to document these things the cost of every visit would have to go up because of the time involved in documenting these items (not to mention the purchase of the system they use to do the documentation) which leads to fewer customers seen per day. Instead, they use a sheet of paper with checkboxes that they give you (probably so they don’t get sued if something happens to your car). The government is setting the map for the marketplace instead of letting the market do it. I do not favor that approach.”
There are so many comparisons you can make here. At the hair salon, did my stylist counsel me on the risks and benefits of adding highlights and lowlights to my hair? Did he warn me that my elderly grandmother would think reddish lowlights to be tacky? Did he suspect that my wanting to change my color was a potential sign of emotional distress? Did he arrange follow up evaluation on exactly WHY I wanted a different color? Did he caution me that being a blonde might not actually mean that I would have more fun? Did he scan the bar code, document the lot number, and record other information about the chemicals in case there is a recall? Did he conduct a time-out prior to actually applying the color to make sure he had mixed the right combination and to ensure I was fully aware of what I was getting myself into?
Of course I’m just being sassy, but if you look at most industries that we depend on or use regularly, if they were being run like healthcare IT (not to mention healthcare in general) it would be like living in a dystopian sci-fi movie.
How do we stop the madness? Or should I change fields and start designing that hair stylist tracking software? Email me.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.







Will be interesting to see how Cerner and McKesson continue to commercialize / monetize CommonWell (to bad CommonWEALTH is already taken – by David Blumenthal).
Lots of money in controlling interoperability. Epic does it for free, but we’ll see the public companies swoop in here and try to make buku bucks in this area.
RE: Cash is King.
Your statement about Epic controlling interoperability for free misses the point. Epic controls interoperability in order to create a competitive advantage and therefore increase its prices to its customers. Epic’s use of proprietary standards and pushing interoperability only within its own customers hurts its customers and prevents “Commonwealth” in the true definition for the rest of us.
@David – I keep hearing this claim that Epic is using “proprietary standards”. What would those “proprietary standards” be? Or is this just another lie that needs to be repeated thousand times to become true?
As for “pushing interoperability only within its own customers”, my understanding is that all Epic customers who use the Care Everywhere interoperability framework have to agree to respond to (properly identified and authorized) requests from other Epic customers. I am not aware of any other way of Epic “controlling interoperability” for their customers, and both Epic to Epic and Epic to non-Epic exchanges use the same open standards for transport and content.